
2 | P a g e
Medicaid Behavioral Health State Plan Services
Provider Requirements and Reimbursement Manual
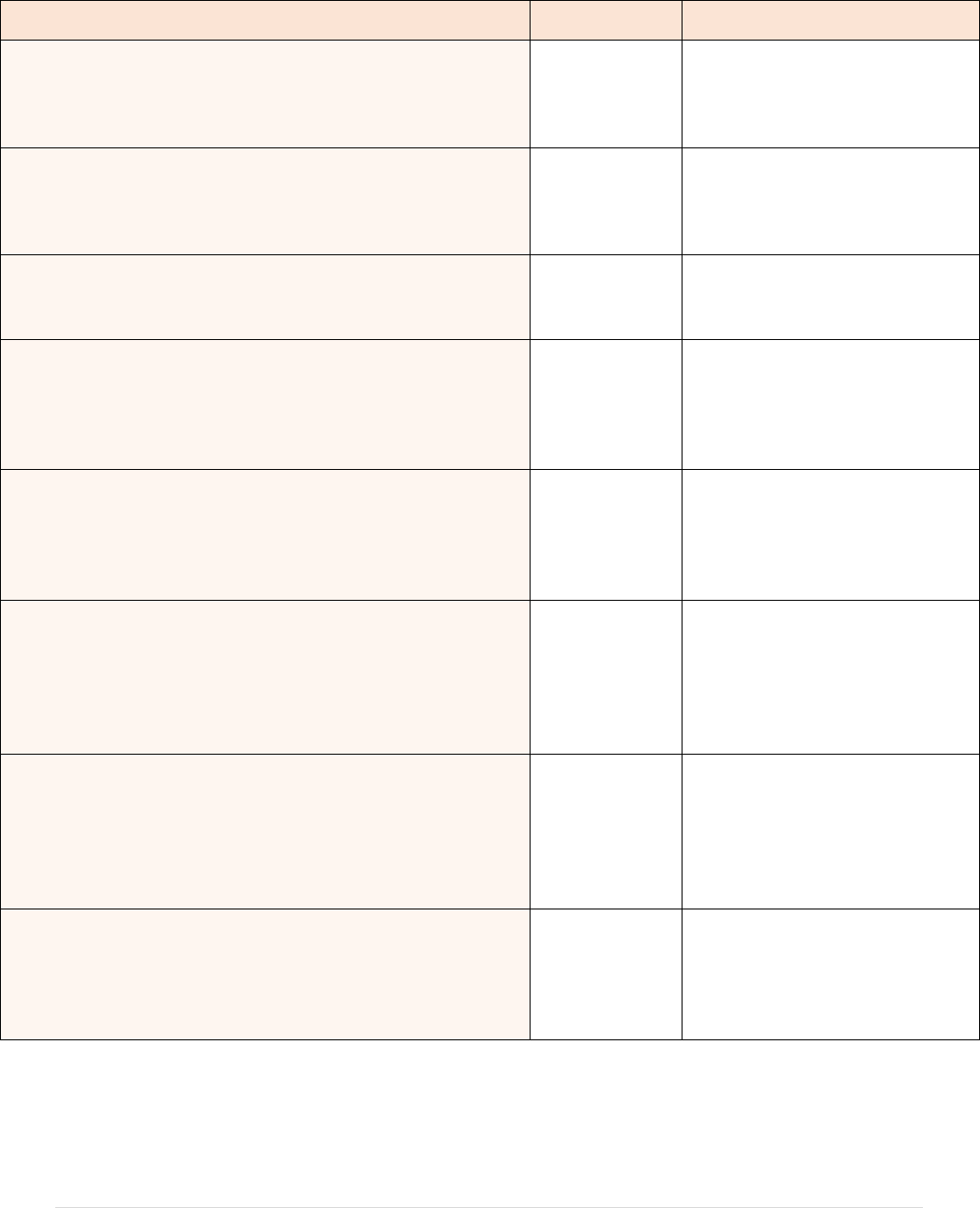
Version
Description of Changes
Last Editor
Release Date
Version 1.0
Initial Draft
State Policy
Team
6-14-16
Version 1.1
Cont’d Draft Manual Development
State Policy
Team
6-24-16
Version 1.2
Third Party Coordination of Benefits
Coordination of Benefits for clients assigned to Managed Care Plans
Modifier-position of modifier
Treatment Plans/plan updates-provisionally active timeframe/review/update timeframes
Supervision-Supervisor Absences
False Claims Act-New Section
Time Based CPT codes -New Section
ECG-Chart updated
Adult Vaccines language added
TBS Removed pharmacist as an approved provider
POS added to individual charts
SUD Assessment Chart update
CLIA certificate Types added
PERM Audits
OTP and Methadone administration codes
TBS Chart
SUD Nursing Chart
ACT
Claims Rolling
ASAM Staffing Levels updated
State Policy
Team
1-31-17
Version 1.3
Correction to U6 and U7 modifier in 3 code charts
Supervisor clarification to SUD residential code charts
HQ and UB corrections in 2 charts
Place of service modifications
H0014 rate correction
State Policy
Team
3-1-17
Version 1.4
Definition of place of service 99
Add information on GT modifier for select codes
Rate correction for H0005
State Policy
Team
3-10-17
Version 1.5
Remove MH and SUD nursing limit
Add GT modifier to applicable codes
QMHS +3 yrs experience – TBS Group Hourly/Per Diem
POS revisions to selected codes
State Policy
Team
3-17-17
Version 1.6
Collateral contacts
Add 96372
Clarify rate reduction for TBS/PSR in excess of 6 units per day
State Policy
Team
3-31-2017
Version 1.7
Procedure modifier added for oral naltrexone
Clarified that 96372 medication administration code is not available to SUD residential providers
Add POS 99 to MH nursing codes
Add POS 04 homeless shelter to TBS Group Hourly/Per Diem
Added modifiers HN and HO to peer recovery to reflect educational level
Added POS 99 to H0004 SUD counseling when provided for crisis
Added POS 99 to SUD nursing
Added POS 11 and 57 to group SUD nursing
Rates paid for trainees and assistance with and without supervision
Removed collateral examples
96372 rate correction
State Policy
Team
4-14-2017
Version 1.8
Add RN/LPN to 96372
POS 99 added to 90838, 90840
Clarify SUD residential needs rendering practitioner
PSY assistant rate correction for 96116, 96118
PSY assistant rate clarification for CPT codes
Clarification that crisis codes (with UT) can be done in POS 23, 99
State Policy
Team
5-10-2017

3 | P a g e
Final Version
1.0
Addition of MD, DO, CNS, CNP, PA to +99355
QMHS +3 rate for TBS Group per diem
POS 99 added to 90846 and 90847
Update Table 1-3 for peer support modifiers
State Policy
Team
6-16-2017
Final Version
1.1
Corrected ACT modifiers for CNS, CNP in Table 1-4
Clarify direct and general supervision language
Correct rates for 96101 and 96111
Add MH H0004
Add dependently licensed practitioners to SUD H0004
Add “Day Treatment” to rate chart for H2012, H2020
State Policy
Team
8-3-2017
Final
Version 1.2
Rendering Practitioner section modified (page 10)
Paraprofessional enrollment language (pages 13, 17)
Procedure modifier UT added to applicable rate charts
Remove POS 99 from H0004 UT as POS 99 always available
SUD residential codes now in Section 5
Edited legal disclaimer
Implementation dates updated
State Policy
Team
9-29-2017
Final
Version 1.3
Replace UT modifier with KX
State Policy
Team
11-15-2017
Final
Version 1.4
Clarified places of service for CPT codes for 84s and 95s
Clarified for CPT codes, LICDC, LCDC, CDC-A are for SUD agencies only
H0001 is now an encounter code
State Policy
Team
12-4-2017
Final Version
1.5
Multi –licensure for independent and medical practitioners
H0014 AT
Clarification for ASAM Levels 3.2 and 3.7
+99355 unit correction
Clarification for ACT Master’s and Bachelor’s levels
State Policy
Team
1-30-2018
Final
Version 1.6
Update psych testing codes
Update MHAS certification information
H0014 AT rates added
Remove hyperlinks no longer working
Various other updates
State Policy
Team
12-15-2018
Final
Version 1.7
Updated psych testing section to include new codes and rates, description of the new codes, and
edits/audits when PA needed
Rendering clarifications
Noted practitioner modifiers are optional unless dually licensed and referenced MCP Resource
Guide
Referenced dual licensure grid on BH site
Removed language about not reporting NPI if second license is dependent since all report NPIs
now
Added SUD Peer Recovery to the PA table (4 hours per day maximum)
99354 for first 60 minutes
Updated laboratory section about enrolling as a laboratory
TBS service chart – not for high school QMHS
H0001 place of service 57
Kept H0004 MH/SUD for historical reference
H0014 AT rate
Updated SUD residential to clearly state per diems do not include room and board costs/payments
Updated hyperlinks
General cleanup
State Policy
Team
3-4-2019
Final
Version 1.8
August 1, 2019 rate increases
Additional practitioners rendering H2019
E&M, diagnostic evaluation rate increases for CNS, CNP, PA
New smoking cessation codes added – Table 3-6.5
Pregnancy lab code added for MH and SUD
State Policy
Team
7-23-2019
Final
Version 1.9
Addition of modifier AT to Table 1-4
Addition of place of service 18 to 99406-07
Column headings for 90849, page 51
H2019 modifiers for group for LSW, LPC, LMFT
Clarify H2019 Psy Asst with Bachelor’s
Updated OTP two week admin procedure modifier to UB
State Policy
Team
7-26-2019
Final
Version 1.10
Add POS 99 to H0005
Updated language regarding dependently licensed enrolling in Medicaid
State Policy
Team
11-27-2019
Final Version
1.11
Emergency Version issued to identify additional procedure codes now available with GT modifier
State Policy
Team
4-1-2020

4 | P a g e
Final Version
1.12
Emergency Version updated
State Policy
Team
6-17-2020
Final Version
1.13
Emergency Version updated
State Policy
Team
7-17-2020
Final Version
1.14
GT modifier requirement
90785 covered under telehealth
State Policy
Team
11-2-2020
Final Version
1.15
E&M coding changes effective 1/1/2021
State Policy
Team
12-31-2020
Final Version
1.16
Addition of pharmacist as an eligible provider type for certain services
State Policy
Team
1-17-2021
Final Version
1.17
Addition of COVID-19 vaccine services (Pfizer and Moderna)
State Policy
Team
2-11-2021
Final Version
1.18
Addition of COVID-19 vaccine services (Johnson & Johnson)
State Policy
Team
3-18-2021
Final Version
1.19
Prolonged services coding changes effective 1/1/2022
Addition of Report of Pregnancy code (T1023)
Inclusion of additional claims rollup examples
Addition of “community” as allowable POS for vaccine administration
Addition of Hep B Vaccine code (90759)
Updated COVID-19 vaccine services resources
State Policy
Team
12-3-2021
Final Version
1.20
Addition of Table 4-3 (SUD individual counseling) which was removed from version 1.19 in error
State Policy
Team
12-23-2021
Final Version
1.21
Addition of Table 3-15(b) reflecting IHBT changes effective 3/1/2022
Addition of Preventive Medicine Counseling code (99401 & 99402)
State Policy
Team
2-1-2022
Final Version
1.22
Addition of table 2-12 for CANS Assessment
Addition of Table 2-13, 2-14, 2-15 for MRSS services
Addition of Section 8 for OhioRISE
State Policy
Team
5-27-2022
Final Version
1.23
Clarified CANS assessments must be entered in Ohio’s CANS IT system to establish and maintain
OhioRISE eligibility
Updated Table 3-15(b) to clarify for dates of service between March 1,2022 – June 30, 2022. Effective
July 1, 2022, services in table 3-15(b) will be available only under OhioRISE
State Policy
Team
6-14-2022
Final Version
1.24
Updated provider enrollment references throughout given PNM implementation effective 10/1/2022
Clarifications to MRSS services section
State Policy
Team
9-29-2022
Final Version
1.25
CPT coding changes (including prolonged services updates) effective 1/1/2023
Additions to Table 2-9: Provider Administered Pharmaceuticals
Updated CANS rate effective 1/1/2023
Updated Table 2-4 to remove coverage for code 99343 effective 1/1/2023
Updated tables 2-5 and 3-4 to remove coverage for prolonged services codes 99354 and 99355 when the
codes are used with E&M home visits and individual and group psychotherapy services effective
1/1/2023
Additions to Table 1-5 to clarify that PA for these services was required for dates of service between
March 1, 2022 – June 30, 2022
Addition to Table 3-11 to clarify HM as a required modifier to indicate PSR versus MH LPN nursing
State Policy
Team
12-19-2022
Final Version
1.26
Updated Table 1-3 to include Psych Intern and Psych Trainee practitioner type numbers in the PSY
Assistant definition
Additions of TD and TE modifiers to Table 1-3 to indicate RN and LPN
Updated Table 1-5 to include MRSS and explain the authorization requirements for stabilization
services
Updated Care Management Specialist (CMS) description
Updated Documentation Guidelines for E&M services references
Addition of information previously found in Opioid Treatment Program Manual to Section 6 (Opioid
Treatment Program), including tables 6-1 through 6-4
Addition of tables 7-1 (SRS Supported Employment) and 7-2 (SRS Peer Recovery Support) to Section 7
(SRS Program)
Removed detailed summary of Vaccines for Children section and added ODH VFC resources
Replaced False Claim Act summary language with reference to OAC rule 5160-1-29
Removed interactive complexity narrative, adding reference to CPT book
State Policy
Team
12-11-2023

5 | P a g e
Removed psychological testing narrative, adding reference to CPT book
Removed table 3-15(a) (Intensive Home Based Treatment for dates of service prior to March 1, 2022)
Removed table 5-1 (SUD Withdrawal Management with Extended On Site Monitoring)
Replaced list of requirements for BHP-Ps with reference to OAC rule 5160-27-01
Removed modifier columns from tables when modifiers were not relevant
Correction to Table 3-2 for code 90832 on 12/11/2023
Correction to Table 2-6 to remove plus signs on 12/22/2023
Correction to Table 3-2 to remove dashes on 12/22/2023
Correction to Table 3-8 H2019 rate on 12/22/2023
Correction to Table 3-10 H2020 rate on 12/22/2023
Correction to Table 7-1 rule citation 5160-27-01 on 12/22/2023
Correction to Table 3-2 90832 MD/DO rate on 12/22/2023
Correction to Table 3-8 H2019 HN, UK rates on 12/22/2023
Correction to Table 3-7 96131 rate on 12/22/2023
Correction to Table 3-11 H2017 HM Community rate on 12/22/2023
Correction to Table 3-2 90832 KX MD/DO rate on 01/24/2024
Correction to table 3-8 H2019 HN,UK rates on 01/24/2024
Correction to table 3-11 H2017 HM Community rate on 01/24/2024
Correction to table 3-8 provider modifiers on 01/24/2024
Revision to Section 7 to clarify provider requirements 01/24/2024
12-22-2023
01-24-2024
Contents
SECTION 1 ................................................................................................................................................ 11
Introduction................................................................................................................................................ 11
Organization of the Provider Manual ...................................................................................................... 11
Provider Enrollment – OhioMHAS-certified providers (organizations) ............................................. 11
Provider Type 84 or 95 ............................................................................................................................ 12
Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) ................................... 12
Out of State MH/SUD Providers ............................................................................................................. 12
Rendering Practitioners ........................................................................................................................... 12
Paraprofessionals ..................................................................................................................................... 13
Multi-licensed Practitioners ..................................................................................................................... 13
Qualified Providers Overview .................................................................................................................. 13
Medical Behavioral Health Practitioners (M-BHPs) ............................................................................... 14
Licensed Independent Behavioral Health Practitioners (I-BHPs) ........................................................... 14
Behavioral Health Practitioners (BHPs) .................................................................................................. 14
Behavioral Health Paraprofessional Practitioners (BHP-Ps) ................................................................... 15
Overview of Supervision ........................................................................................................................... 16
Table 1-1: Supervision for Current Procedural Terminology (CPT®) Codes ................................ 16
Table 1-2: Supervision for Healthcare Common Procedure Coding System (HCPCS) Codes ...... 17
Incident to Services .................................................................................................................................... 17
Practitioner Modifiers ............................................................................................................................... 17
Table 1-3: Practitioner Modifiers ......................................................................................................... 18
Procedure Modifiers .................................................................................................................................. 19

6 | P a g e
Table 1-4: Procedure Modifiers ........................................................................................................... 19
Place of Service (POS) ............................................................................................................................... 19
Claims Detail Rollup for Same Day Services .......................................................................................... 20
Third Party Payer (TPP) Coordination of Benefits (COB) ................................................................... 20
Benefits and Prior Authorization ............................................................................................................. 21
Table 1-5: Prior Authorization ............................................................................................................. 22
Non-Covered Services ............................................................................................................................... 23
Fraud, Waste, and Abuse .......................................................................................................................... 23
Review of Provider Records ..................................................................................................................... 24
Payment Error Rate Measurement (PERM) .......................................................................................... 24
Medicaid National Correct Coding Initiative ......................................................................................... 24
NCCI Procedure-To-Procedure (PTP) Edits ........................................................................................... 24
Medically Unlikely Edits (MUEs) ........................................................................................................... 25
Time-Based CPT Codes ............................................................................................................................ 26
Prolonged Services ..................................................................................................................................... 26
SECTION 2 ................................................................................................................................................ 27
Behavioral Health Services ....................................................................................................................... 27
Evaluation and Management Codes ........................................................................................................ 28
Table 2-1: Evaluation & Management Office Visit ............................................................................ 28
Table 2-2: Prolonged Service codes for E&M Office Visits ............................................................... 29
Table 2-3 Evaluation and Management Office Visit - Report of Pregnancy ................................... 30
Table 2-4: Evaluation & Management Home Visit ............................................................................ 31
Table 2-5: Prolonged Service codes for E&M Home Visits ............................................................... 32
Table 2-6: Preventive Medicine Counseling ........................................................................................ 32
Table 2-7: Psychiatric Diagnostic Evaluation ..................................................................................... 33
Table 2-8 – Electrocardiogram ............................................................................................................. 34
Table 2-9: Provider Administered Pharmaceuticals .......................................................................... 35
National Drug Code (NDC)....................................................................................................................... 36
Laboratory Services ................................................................................................................................... 37
Table 2-10: Laboratory Services .......................................................................................................... 37
Laboratory Codes ...................................................................................................................................... 37
Vaccines ...................................................................................................................................................... 38
Table 2-11: Covered Vaccines for Behavioral Health Providers ...................................................... 38
COVID-19 Vaccine Administration ........................................................................................................ 39
Vaccines for Children (VFC) Program .................................................................................................... 39

7 | P a g e
Vaccines for Adults ................................................................................................................................. 40
Child and Adolescent Needs Strengths (CANS) Assessment ................................................................. 40
Table 2-12: Child and Adolescent Needs and Strengths (CANS) Assessment ................................. 41
Mobile Response and Stabilization Service (MRSS) .............................................................................. 42
Table 2-13: MRSS Crisis Mobile Response ......................................................................................... 43
Table 2-14: MRSS Crisis Mobile Response Follow Up ...................................................................... 45
Table 2-15: MRSS Stabilization Service .............................................................................................. 46
SECTION 3 ................................................................................................................................................ 48
Psychotherapy Services ............................................................................................................................. 48
Table 3-1: Psychotherapy for Crisis .................................................................................................... 48
Table 3-2: Individual Psychotherapy ................................................................................................... 50
Table 3-3: Family Psychotherapy......................................................................................................... 53
Table 3-4: Prolonged Service Codes for Psychotherapy .................................................................... 56
Table 3-5: Group Psychotherapy ......................................................................................................... 58
Interactive Complexity .............................................................................................................................. 59
Table 3-6: Interactive Complexity ....................................................................................................... 59
Psychological Testing................................................................................................................................. 60
Table 3-7: Psychological Testing .......................................................................................................... 60
Table 3-7.5: Smoking Cessation ........................................................................................................... 65
Healthcare Common Procedure Coding System (HCPCS) Mental Health Services .......................... 67
Table 3-8: Therapeutic Behavioral Services (TBS) ............................................................................ 67
Table 3-9: RN and LPN Nursing Services ........................................................................................... 70
Table 3-10: TBS Group Service-Hourly and Per Diem (Day Treatment) ........................................ 71
Table 3-11: Psychosocial Rehabilitation (PSR) ................................................................................... 73
Table 3-12: Screening, Brief Intervention and Referral to Treatment ............................................. 74
Table 3-13: Community Psychiatric Supportive Treatment (CPST) ............................................... 75
Assertive Community Treatment (ACT) ................................................................................................. 77
Table 3-14: Assertive Community Treatment (ACT) ........................................................................ 77
Intensive Home Based Treatment (IHBT) .............................................................................................. 78
SECTION 4 ................................................................................................................................................ 78
Substance Use Disorder (SUD) Coverage ................................................................................................ 78
Table 4-1: SUD Assessment .................................................................................................................. 78
Table 4-2: SUD Peer Recovery Support .............................................................................................. 79
Table 4-3: Individual Counseling ......................................................................................................... 79
Individual Counseling .............................................................................................................................. 79

8 | P a g e
Table 4-4: Group Counseling ............................................................................................................... 80
Table 4-5: SUD Case Management ...................................................................................................... 81
Table 4-6: SUD Drug Screening ........................................................................................................... 82
Table 4-7: SUD RN and LPN Nursing Services .................................................................................. 83
Table 4-8: Intensive Outpatient Level of Care Group Counseling ................................................... 84
Table 4-9: Partial Hospitalization (PH) Level of Care Group Counseling ...................................... 85
Table 4-10: SUD Withdrawal Management with Extended On Site Monitoring ............................ 86
SUD Residential Treatment ...................................................................................................................... 86
SUD Withdrawal Management with Extended On Site Monitoring ....................................................... 86
Table 5-1: Clinically Managed Low-Intensity Residential Treatment ............................................. 87
Table 5-2: Clinically Managed Residential Withdrawal Management ............................................ 87
Table 5-3: Clinically Managed Population-Specific High Intensity Residential Treatment (Adults)
................................................................................................................................................................. 88
Table 5-4: Clinically Managed High Intensity Residential Treatment ............................................. 88
Table 5-5: Medically Monitored Intensive Inpatient Treatment (Adults) and Medically
Monitored High-Intensity Inpatient Services (Adolescent) ............................................................... 89
Table 5-6: Medically Monitored Inpatient Withdrawal Management ............................................. 89
SECTION 6 ................................................................................................................................................ 90
Opioid Treatment Programs .................................................................................................................... 90
Provider Network Management (PNM) Enrollment for Opioid Treatment Programs ............................ 90
Buprenorphine Administration for SUD Treatment Programs ................................................................ 90
OTP Billing Guidance ............................................................................................................................. 90
Table 6-1: Opioid Treatment Programs .............................................................................................. 92
Table 6-2: Opioid Treatment Programs .............................................................................................. 93
Coordination of Benefits: Medicare Opioid Treatment Program Benefit ........................................... 94
Table 6-3: Medicare Opioid Treatment “Bundle” Billing Codes ...................................................... 95
SECTION 7 ................................................................................................................................................ 96
Specialized Recovery Services (SRS) Program [1915(i)] ....................................................................... 96
Table 7-1: SRS Supported Employment.............................................................................................. 97
Table 7-2: SRS Peer Recovery Support ............................................................................................... 97
SECTION 8 ................................................................................................................................................ 98
OhioRISE.................................................................................................................................................... 98
Appendix: Ohio Medicaid List of Place of Service Codes...................................................................... 99
To return to the Table of Contents after reviewing a section: Click Alt and left arrow.

9 | P a g e

10 | P a g e
Legal Disclaimer: Ohio Department of Medicaid (ODM) strives to make the information in this manual
as accurate, complete, reliable, and timely as possible. However, ODM makes no claims, promises, or
guarantees about the accuracy, completeness, or adequacy of this information. This is the most current
version of the Medicaid Behavioral Health State Plan Services-Provider Requirements and
Reimbursement Manual, which is being released as an informational and educational tool; however, this
manual is subject to change and future revisions as the implementation and operations of the Ohio
Medicaid program changes. ODM, its employees, agents, or others who provide the answers will not be
liable or responsible to you for any claim, loss, injury, liability, or damages related to your use of or
reliance upon this information. This manual is intended solely as an informational and educational
resource for providers intending to participate in the Medicaid behavioral health programs and for the
public. The information contained in this manual is not intended to set new standards and requirements
beyond the scope of those standards and requirements found in the Ohio Administrative Code. In the case
of any conflict between the information contained in this manual and Ohio Administrative Code or Ohio
Revised Code, the Ohio Administrative Code or Ohio Revised Code, as applicable, prevails. This
information is not intended to be a substitute for professional legal, financial, or business advice. This
manual does not create, nor is it intended to create, an attorney-client relationship between you and Ohio.
You are urged to consult with your attorney, accountant, or other qualified professional if you require
advice or opinions tailored to your specific needs and circumstances.

11 | P a g e
SECTION 1
Introduction
The Ohio Department of Medicaid (ODM) has created this manual to help providers of community
behavioral health services understand coverage and reimbursement for services provided under the fee-
for-service program. For purposes of this manual, community behavioral health providers are those who
are certified by the Ohio Department of Mental Health and Addiction Services (OhioMHAS) as described
in Ohio Administrative Code (OAC) rule 5160-27-01. The Ohio Administrative Code contains specific
regulatory information that is the basis for the information contained in this manual. Chapter 5160-1
contains regulatory information on the Medicaid program in general. Additional information is available
in the following administrative rule chapters:
• Chapter 5160-1 General Provisions (includes telehealth)
• Chapter 5160-4 Medical and Surgical Services
• Chapter 5160-8 Therapeutic and Diagnostic Services
• Chapter 5160-27 Community Mental Health Agency Services
• Chapter 5160-28 Federally Qualified Health Center and Rural Health Clinic Services
• Chapter 5160-43 Specialized Recovery Services Program
Organization of the Provider Manual
This manual is organized into eight sections.
• Section 1 includes information regarding provider enrollment, rendering provider, supervisor
requirements, benefit and claims related requirements, and information on fraud, waste and abuse.
• Section 2 is dedicated to medical and behavioral health services that can be provided by both
mental health and substance use disorder (SUD) agencies.
• Section 3 provides specific service requirements and claims billing information for services
which can only be performed by mental health agencies. This section includes evidence-based
practices.
• Section 4 provides specific service requirements and claims billing information for services
which can only be performed by SUD outpatient agencies.
• Section 5 provides specific service requirements and claims billing information for services
which can only be performed by SUD residential agencies.
• Section 6 provides information on Opioid Treatment Programs (OTPs). .
• Section 7 provides information on the Specialized Recovery Services (SRS) program and related
resources.
• Section 8 provides information on OhioRISE (Resilience through Integrated Systems and
Excellence), a program to help children who have complex and serious behavioral health needs.
Provider Enrollment – OhioMHAS-certified providers (organizations)
All provider enrollment applications must be submitted using Ohio Medicaid’s Provider Network
Management (PNM) module. The PNM module is the single point for providers to complete provider
enrollment, centralized credentialing, and provider self-service. For more information about the PNM
please visit www.managedcare.medicaid.ohio.gov/managed-care/centralized-credentialing.
To participate in the Ohio Medicaid program, including contracting with the managed care plans,
OhioMHAS-certified providers must enroll in the Ohio Medicaid program. The IT system that supports
Ohio Medicaid provider functions is the Provider Network Management (PNM) module. There are two

12 | P a g e
provider types associated with behavioral health benefits; provider type 84 is used for accessing the
mental health benefit while provider type 95 is used for accessing the substance use disorder benefit.
Organizations that will be providing both benefits will need to enroll as BOTH provider types.
Provider Type 84 or 95
Prior to enrollment in the Ohio Medicaid program, a provider must be certified by OhioMHAS as a
provider of behavioral health (BH) services. Information on OhioMHAS’s service certification can be
obtained from the OhioMHAS Bureau of Licensure & Certification by calling 614-752-8880 or by
visiting the OhioMHAS licensure and certification webpage here: Licensure & Certification | Department
of Mental Health and Addiction Services (ohio.gov). Once certified by OhioMHAS as a BH service
provider, an online application or applications for enrollment in the Ohio Medicaid program must be
submitted using the PNM module. There may be an application fee for applying as provider type 84
and/or 95. During the enrollment process, a provider specialty will need to be selected for each provider
type. ODM will add or change specialties as necessary based upon the OhioMHAS/SAMHSA
certification(s) and/or OhioMHAS licensure documentation received with the application.
For more information about enrolling as a Medicaid provider, please visit the following link:
https://managedcare.medicaid.ohio.gov/managed-care/centralized-credentialing/about-pnm
Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)
FQHCs and RHCs may be certified by OhioMHAS for the provision of community behavioral health
services by enrolling as a provider type 84 and/or 95. OAC Rule 5160-28-03 describes requirements for
FQHC and RHC services, including services that are considered FQHC and RHC Prospective Payment
System (PPS) services. For OhioMHAS certified providers who are also FQHCs or RHCs, behavioral
health services that are not FQHC or RHC PPS services are covered under OAC Chapter 27 and may be
billed under their Ohio Medicaid Provider type 84 or 85 enrollment and will be paid in accordance with
OAC Chapter 27 as described in this manual.
Out of State MH/SUD Providers
Pursuant to Ohio Administrative Code (OAC) rule 5160-27-01, MH and/or SUD agencies/programs
operating outside of the state of Ohio must be recognized (regulated) in the state in which it operates as a
provider of community-based MH and/or SUD services. That documentation must be submitted along
with the organization’s Medicaid application.
Rendering Practitioners
ODM requires that the rendering practitioner for behavioral health services be listed on claims submitted
to Ohio Medicaid for payment. Their personal NPI must be reported in the rendering field on the claim
for each service they provide.
All rendering practitioners are required to have a National Provider Identifier (NPI) to render services to
Medicaid enrollees AND they will be required to enroll in the Ohio Medicaid program and affiliate with
their employing/contracting agency. An NPI can be obtained by visiting
https://nppes.cms.hhs.gov/NPPES.
Once the provider has obtained an NPI, they must visit the PNM and enroll as a provider in the Ohio
Medicaid Program. More details on this process are available at:
https://managedcare.medicaid.ohio.gov/managed-care/centralized-credentialing/about-pnm

13 | P a g e
Paraprofessionals
• Paraprofessionals, practitioners without a professional license, may render some mental health
and/or SUD services. They must enroll in Ohio Medicaid following the instructions above. The
provider type in Ohio’s PNM system is “96”. Paraprofessionals may select more than one
specialty. For example, one could enroll as a Qualified Mental Health Specialist (QMHS) and
may also enroll as a Care Management Specialist (CMS) by selecting specialties 960 (QMHS)
and 962 (CMS).
If a QMHS or CMS practitioner obtains additional educational credentials or years of experience after
their initial enrollment, the employing/contracting agency should provide documentation of the
educational credential or experience by submitting a provider update to the ODM Provider Enrollment
mailbox: medicaid_provider_update@medicaid.ohio.gov. Once the documentation has been received and
approved, the provider’s enrollment status will be updated to match. (See more information below about
QMHS, CMS and Peer Specialists).
Multi-licensed Practitioners
ODM recognizes that some individuals may hold more than one (1) license or an assistant/trainee
credential with differing scopes of practice. In order to allow these practitioners to operate under the
scope of multiple professional credentials, ODM is allowing these practitioners to add a multi-license
specialty. This multi-license specialty will allow the practitioner to render services available under their
second license or credential. Please refer to the Dual Licensure Grid located at
https://bh.medicaid.ohio.gov/manuals under the Billing Resources section.
To enroll with multi-license specialty:
If a practitioner has more than one credential/paraprofessional recognition, please include a comment in
the Notes section of the enrollment application indicating what additional credential/paraprofessional
recognition is held. Paraprofessionals can select a primary, a secondary or multiple secondary specialty.
Be certain to upload the necessary documentation for each license/certificate. If already enrolled with
ODM, email [email protected] with necessary information to support the
second specialty.
Claim submission:
• Reporting additional licensure on claims - Practitioners with the multi‐licensed practitioner
specialty submit claims as follows:
o For their original license according to information found elsewhere in this manual:
rendering NPI, applicable procedure modifiers, etc.
o For services under their additional license(s), the claims will require an additional
modifier to reflect under what additional license they are operating.
o For example, a person enrolled with ODM as an RN who is also an LPCC must have the
UH modifier in addition to their individual practitioner NPI on to the detail line of the
claim in order for ODM’s claims payment system to recognize this practitioner as an
allowable renderer of the service.
See the “Modifiers” tab on the Dual Licensure Grid referenced above.
Qualified Providers Overview
It is the state’s expectation that a practitioner will work within their scope of practice.

14 | P a g e
Medical Behavioral Health Practitioners (M-BHPs)
Medical Behavioral Health Providers are professionals who are licensed by a professional board in the
state of Ohio and are authorized to practice some level of general medicine and have specialty experience
and/or training related to persons with behavioral health conditions. M-BHPs are:
• Physicians as defined in Chapter 4731 of the Ohio Revised Code who are licensed by the state of
Ohio Medical Board and legally authorized to practice in the state of Ohio.
• Clinical nurse specialists (CNS), certified nurse practitioners (NP), registered nurses (RN),
and licensed practical nurses (LPN) as defined in Chapter 4723 of the Ohio Revised Code who
are licensed and certified by the state of Ohio Nursing Board and legally authorized to practice in
the state of Ohio.
• Physician assistants as defined in Chapter 4730 of the Ohio Revised Code who are licensed by
the state of Ohio Medical Board and legally authorized to practice in the state of Ohio.
• Pharmacists as defined in OAC rule 5160-8-52 who are licensed by the state of Ohio Board of
Pharmacy. Tables 2-1, 2-6 and 2-9 provide further details.
Licensed Independent Behavioral Health Practitioners (I-BHPs)
The following are professionals who are licensed by a professional board in the state of Ohio and are
authorized to practice independently (they are not subject to professional supervision) and have specialty
experience and/or training related to persons with behavioral health conditions. I-BHPs are:
• Psychologists and school psychologists as defined in Chapter 4732 of the Ohio Revised Code
who are licensed by the state of Ohio Board of Psychology and legally authorized to practice in
the state of Ohio.
• Licensed professional clinical counselors (LPCC), licensed independent social workers
(LISW), and licensed independent marriage and family therapists (LIMFT) as defined in
Chapter 4757 of the Ohio Revised Code who are licensed by the state of Ohio Counselor, Social
Worker, and Marriage & Family Therapist Board and legally authorized to practice in the state of
Ohio.
o For the purposes of this manual, LIMFT has the same meaning as IMFT as used by the
Counselor, Social Worker, and Marriage & Family Therapist Board.
• Licensed independent chemical dependency counselors (LICDC) as defined in Chapter 4758
of the Ohio Revised Code who are licensed by the Ohio Chemical Dependency Professionals
Board and legally authorized to practice in the state of Ohio.
Behavioral Health Practitioners (BHPs)
Please Note: In the following descriptions, the term “registered with the state of Ohio” means an individual
is known to the state professional and/or licensing boards as a practitioner who has met the applicable
professional requirements.
The following are professionals who are licensed by a professional board in the state of Ohio and are
authorized to practice under direct or general clinical supervision and have specialty experience and/or
training related to persons with behavioral health conditions These paraprofessionals must be enrolled
with ODM and affiliated with their community behavioral health agency. BHPs are:
Licensed
• Board licensed school psychologists as defined in Chapter 3301 of the Ohio Revised Code and
who are licensed by the Ohio Department of Education and legally authorized to practice in the
state of Ohio.

15 | P a g e
• Licensed professional counselors (LPC), licensed social workers (LSW), and licensed
marriage and family therapists (LMFT) licensed by the Ohio Counselor, Social Worker, and
Marriage & Family Therapist Board in accordance with Chapter 4757 of the Ohio Revised Code
and legally authorized to practice in the state of Ohio.
o For the purposes of this manual, LMFT has the same meaning as MFT as used by the
Counselor, Social Worker, and Marriage & Family Therapist Board.
• Licensed chemical dependency counselor IIIs and licensed chemical dependency counselor
IIs licensed by the Ohio Chemical Dependency Professional Board in accordance with Chapter
4758 of the Ohio Revised Code and legally authorized to practice in the state of Ohio.
Trainees/Assistants
• Psychology assistant/intern/trainees working under the supervision of a psychologist licensed
by the Ohio Board of Psychology and legally authorized to practice in the state of Ohio.
• School psychology assistant/intern/trainees working under the supervision of a psychologist or
school psychologist licensed by the Ohio Board of Psychology and legally authorized to practice
in the state of Ohio.
• Counselor trainees registered with the Ohio Counselor, Social Worker, and Marriage & Family
Therapist Board in accordance with Chapter 4757 of the Ohio Revised Code and legally
authorized to practice in the state of Ohio. A counselor trainee is seeking licensure as a
professional counselor and is enrolled in a practicum or internship in a counselor education
program.
• Social work trainees registered with the Ohio Counselor, Social Worker, and Marriage & Family
Therapist Board in accordance with Chapter 4757 of the Ohio Revised Code and legally
authorized to practice in the state of Ohio. A social work trainee is completing their school
approved field placement under a council on social work education accredited master’s level
program.
• Social work assistants registered with the Ohio Counselor, Social Worker, and Marriage &
Family Therapist Board in accordance with Chapter 4757 of the Ohio Revised Code and legally
authorized to practice in the state of Ohio.
• Marriage and family therapist trainees registered with the Ohio Counselor, Social Worker, and
Marriage & Family Therapist Board in accordance with Chapter 4757 of the Ohio Revised Code
and legally authorized to practice in the state of Ohio. A marriage and family therapist trainee is a
student enrolled in a marriage and family therapist practicum or internship in Ohio.
• Chemical dependency counselor assistants certified by the Ohio Chemical Dependency
Professionals Board in accordance with Chapter 4758 of the Ohio Revised and legally authorized
to practice in the state of Ohio.
Behavioral Health Paraprofessional Practitioners (BHP-Ps)
The following are eligible paraprofessionals who are NOT licensed by a professional board in the state of
Ohio but are specially trained to provide a specialty service or services to persons with or in recovery
from substance use disorders (SUDs) and/or mental health (MH) conditions. BHP-Ps are:
• Peer Recovery Supporter (PRS): For purposes of this manual, “peer recovery supporter” (PRS)
has the same meaning as a “certified peer supporter” as certified by OhioMHAS. This includes
certified peer recovery supporters, certified youth peer supporters, and certified family peer
supporters as described in OAC rule 5122-29-15.1.
• Care Management Specialist (CMS) - An individual who has received training for or education
in alcohol and other drug addiction, abuse, and recovery and who has demonstrated, prior to or
within ninety days of hire, competencies in fundamental alcohol and other drug addiction, abuse,
and recovery.

16 | P a g e
• Qualified Mental Health Specialist (QMHS) - an individual who has received training or
education in mental health competencies and who has demonstrated, prior to or within ninety
days of hire, competencies in basic mental health skills along with competencies established by
the agency, and who are not otherwise designated as providers or supervisors, and who are not
required to perform duties covered under the scope of practice according to Ohio professional
licensure. Additional information may be found in OAC rule 5160-27-01.
• Qualified Mental Health Specialist +3 (QMHS +3) - an individual who has received training or
education in mental health competencies and has a minimum of three years of relevant work
experience and has demonstrated, prior to or within ninety days of hire, competencies in basic
mental health skills along with competencies established by the agency, and who are not
otherwise designated as providers or supervisors, and who are not required to perform duties
covered under the scope of practice according to Ohio professional licensure.
Overview of Supervision
Ohio Medicaid covers services provided by practitioners who, under state licensing, require supervision.
The types of practitioners who may supervise are determined according to the appropriate licensing
boards.
General supervision: The supervising practitioner must be available by telephone to provide assistance
and direction if needed.
Direct supervision: The supervising practitioner must be “immediately available” and “interruptible” to
provide assistance and direction throughout the performance of the procedure; however, he or she does
not need to be present in the room when the procedure is performed.
Ohio Medicaid requires the following practitioners to practice under either direct or general supervision.
Reporting the supervising NPI on the claim is optional. For those practitioners listed below with direct
supervision, the service will be paid at direct supervisor’s rate when supervisor NPI is included in the
header of the claim. If the supervisor NPI is not included on the claim indicating the service is provided
under general supervision, the service will be paid at 72.25% of maximum fee.
Table 1-1: Supervision for Current Procedural Terminology (CPT®) Codes
Practitioner Providing the Service:
Type of Supervision
Licensed professional counselor
General
Licensed chemical dependency counselor II or III
General
Licensed social worker
General
Licensed marriage and family therapist
General
Psychology assistant, intern, trainee
Direct/General
Chemical dependency counselor assistant
Direct/General
Counselor trainee
Direct/General
Social worker trainee
Direct/General
Marriage and family therapist trainee
Direct/General

17 | P a g e
Table 1-2: Supervision for Healthcare Common Procedure Coding System (HCPCS) Codes
Practitioner Providing the Service:
Type of Supervision
Psychology assistant, intern, trainee
General
Chemical dependency counselor assistant
General
Counselor trainee
General
Social worker assistant
General
Social worker trainee
General
Marriage and family therapist trainee
General
Qualified Mental Health Specialist
General
Care Management Specialist
General
Certified peer supporters
General
Practitioners requiring supervision must have supervision available to them at all times, including
supervisor sick days, trainings, vacations, etc. Each licensing board regulates supervision requirements for
their provider types and may have specific requirements pertaining to supervisor coverage during
absences. In the absence of board guidance on supervisor coverage, Ohio Medicaid does not require
practitioners to be assigned to a specific supervisor, therefore, any qualified supervising practitioner
permitted by the practitioner’s respective licensing board’s OAC may provide coverage during absences
but must assume all supervision responsibilities, including signing off on services provided. The
following websites contain further guidance on supervision:
• State of Ohio Medical Board - http://med.ohio.gov/
• Ohio Nursing Board - http://www.nursing.ohio.gov/
• Counselor, Social Worker and Marriage and Family Therapist Board –
https://cswmft.ohio.gov/wps/portal/gov/cswmft/home
• Ohio Chemical Dependency Professionals Board - http://ocdp.ohio.gov/
• Ohio Board of Psychology - http://psychology.ohio.gov/
*This is a brief overview concerning licensure and scope of practice. It is each agency or provider’s
responsibility to understand the laws, rules, and requirements applicable to their licensure and scope
of practice.
Incident to Services
The term “incident to” refers to the services or supplies that are a key part of the physician’s personal
professional services in the course of diagnosis or treatment of an illness or injury. In plain language:
under the “incident to” provision of Medicare, services are submitted under the physician’s NPI but are
actually performed by someone else. There are restrictions on the types of services that ancillary
personnel may perform under this provision. Ohio Medicaid follows the CMS guidelines on “incident to
services”. More information is available in The “Incident To” Provision of Medicare Fact Sheet.
Additional Resources for CMS “incident to” billing information:
• Medicare Benefit Policy Manual, Chapter 15 Section 60.1
• CMS Medicare Learning Network Articles
Practitioner Modifiers
In order to communicate detailed information in an efficient, standardized way, modifiers are two-
character suffixes that healthcare providers or coders attach to a CPT or HCPCS code to provide
additional information about the practitioner or procedure. It is extremely important to accurately report

18 | P a g e
modifiers as they are used to count towards soft limits, price services, and adjudicate claims
appropriately. Modifiers are always two characters in length. They may consist of two numbers, two
letters, or a combination of a letter and a number (alphanumeric). Ohio Medicaid will accept modifiers in
any order, however, modifier fields on the claim must be populated in order from one to four (the first
modifier field must be populated before the second modifier field, etc.).
Table 1-3: Practitioner Modifiers
Practitioner Providing the Service:
Professional Abbreviation
Practitioner
Modifier
Licensed professional counselor
LPC
U2*
Licensed chemical dependency counselor III
LCDC III
U3*
Licensed chemical dependency counselor II
LCDC II
U3*
Licensed social worker
LSW
U4*
Licensed marriage and family therapist
LMFT
U5*
Licensed practical nurse
LPN
TE*
Registered nurse
RN
TD*
Psychology assistant, psychology intern, psychology trainee
PSY assistant
U1*
Chemical dependency counselor assistant
CDC-A
U6*
Counselor trainee
C-T
U7*
Social worker assistant
SW-A
U8*
Social worker trainee
SW-T
U9*
Marriage and family therapist trainee
MFT-T
UA*
QMHS – high school
QMHS
HM
QMHS – Associate’s
QMHS
HM
QMHS – Bachelor’s
QMHS
HN
QMHS – Master’s
QMHS
HO
QMHS – 3 years’ experience
QMHS
UK
Care management specialist – high school
CMS
HM
Care management specialist – Associate’s
CMS
HM
Care management specialist – Bachelor’s
CMS
HN
Care management specialist – Master’s
CMS
HO
Peer recovery supporter – high school
PRS
HM
Peer recovery supporter – Associate’s
PRS
HM
Peer recovery supporter – Bachelor’s
PRS
HN
Peer recovery supporter – Master’s
PRS
HO
*For fee for service, these modifiers are optional except when the rendering practitioner holds multi-
license specialties and is rendering a service only available under a secondary license/certificate.
Additional modifiers (HM, HN, HO, and UK) to designate education level are required for services as
listed in this table. For information on MCP requirements, please refer to
https://bh.medicaid.ohio.gov/Provider/Medicaid-Managed-Care-Plans.

19 | P a g e
Procedure Modifiers
The following modifiers are required to describe specific circumstances that may occur during a service:
Table 1-4: Procedure Modifiers
Service Circumstance
Modifier
Group service
HQ
Physician, team member (ACT)
AM
CNP team member (ACT)
UC
PA or CNS, team member (ACT)
SA
Master’s level, RN, LPN, team member (ACT)
HO
Bachelor’s level, team member (ACT)
HN
Peer recovery supporter, team member (ACT)
HM
Required to indicate PSR (rather than MH LPN nursing services)
HM
Pregnant/parenting women’s program
HD
Complex/high tech level of care
TG
Cognitive Impairment (SUD residential ASAM level 3.3)
HI
Licensed practitioners providing TBS Group Hourly/Per Diem (day treatment) or SUD
intensive outpatient, partial hospitalization, or group counseling
HK
OTP Daily Administration
HF
OTP One Week Administration (2 – 7 Days)
TV
OTP Two Week Administration (8 – 14 Days)
UB
OTP Three Week Administration (15 – 21 Days)
TS
OTP Four Week Administration (22 – 28 Days)
HG
Significant, separately identifiable Evaluation & Management (E&M) service by
physician or other qualified health professional on the same day of the procedure or
other service
25
NCCI modifiers (See NCCI Section)
59, XS, XE, XU and XP
CLIA waived test- certificate of waiver – CMS certificate type code 2 or higher
required
QW
Crisis modifier used on T1002, H2017 (PSR only, not LPN nursing service), H2019,
H0004 and 90832
KX
Physician delivering SUD group counseling
AF
The GT Modifier is required for any service delivered via secured video-conferencing
or other allowable telehealth delivery methods in accordance with OAC 5160-1-18
(See the rule appendices for the list of services that may be delivered via telehealth)
GT
Withdrawal management 2-3 hours
AT
Place of Service (POS)
Providers must accurately identify and report on each claim detail line where a service took place using
the most appropriate CMS place of service code. Each billing chart in this manual will list the place of
service codes covered by Medicaid.
“Other Place of Service” Setting

20 | P a g e
Place of service “99-Other Place of Service” has been redefined for Ohio Medicaid as “Community”. See
this manual’s Appendix for a more complete definition of this and other places of service.
Claims Detail Rollup for Same Day Services
When the same service is rendered to the same client by the same practitioner at more than one time
during the same day, those services should be “rolled up” into a single detail line on a claim. However, if
anything differs except the time the service was rendered, the claims should be reported separately.
Services that need to be rolled must be rolled by the same date of service, same client, same HCPCS code,
same modifier(s), same individual rendering practitioner NPI, same supervisor NPI, and same place of
service. Services that are not appropriately rolled up may result in a denial for duplicate services.
Example 1: Amy Smith, RN renders TBS to a client in the office in the morning and then again in the
office later that afternoon. This is acceptable to roll up the two patient contacts into the same claim line
because there is the same service, the same rendering practitioner, the same client, and the same place of
service.
Example 2: Amy Smith, RN renders TBS to a client in the office in the morning and then again in the
client’s home later that afternoon. The services should be reported on separate detail lines with
appropriate place of service identifying home or office.
Third Party Payer (TPP) Coordination of Benefits (COB)
Coordination of benefits is the process of determining the payment obligations of each health plan,
insurance policy, or third-party resource when two or more resources cover the same benefits for a
Medicaid recipient. Coordination of benefits is a federal requirement set forth in 42 CFR 433 Subpart D
and includes specific activities for state Medicaid agencies related to third-party liability (TPL).
Medicaid, or a Medicaid Managed Care Entity (MCE) must be the payer of last resort, except as allowed
in OAC rules 5160-1-08 and 5160-26-09.1.
After a provider has gone through all reasonable measures to obtain all third-party payments as described
in OAC rules 5160-1-08 and 5160-26-09.1 a claim may be submitted to ODM/MCEs requesting
reimbursement for the rendered service(s). Providers who have received a zero payment from a third-
party payer (TPP) or a partial payment will need to use the appropriate claim adjustment reason codes
(CARCs) from the primary’s Explanation of Benefits (EOB) on the claim submission to ODM/MCEs.
ODM maintains a list of specific service procedure codes or combinations of procedure codes and
rendering providers that are covered by Ohio Medicaid but are not generally covered by commercial
payers or Medicare. This list, known as the BH Medicare and TPL list is located at
https://medicaid.ohio.gov/resources-for-providers/bh/manuals under Billing Resources/Medicare and TPL
Bypass list. The list is separated into three sections – Medicare, Medicare Opioid Treatment Program
(OTP), and TPL Bypass (for commercial payers).
• The Medicare list includes procedure codes and procedures code/rendering provider type
combinations not covered by Medicare.
• The Medicare OTP list is only applicable to opioid treatment providers serving individuals with
Medicare coverage.
• The TPL Bypass list is applicable to other payers (other than Medicare or Medicaid payers).
For the procedure codes on each of these payer lists, respectively, the provider may “bypass” the
requirement to first bill the Third Party Payer (commercial or Medicare payer) and submit the claim
directly to Medicaid.

21 | P a g e
The BH Medicare and TPL Bypass List was created to allow payment for certain services ODM identified
that are not typically covered by TPPs. However, if TPP coverage is later discovered through ODM’s or
an MCE’s post payment recovery process, payment may be recouped in accordance with federal
Medicaid requirements. Therefore, if a provider is unsure of a specific TPP’s coverage policy for any of
the services or procedure codes, the provider should confirm coverage prior to billing for the service
directly to Medicaid to avoid a future recoupment. As Medicare and commercial insurance coverage
changes, the Bypass List will be updated.
The BH Medicare and TPL Bypass List only applies to claims submitted by Medicaid provider types 84
(Community Mental Health Agencies) and 95 (Substance Use Disorder Treatment Providers). ODM
recommends:
• BH providers require individuals to provide TPP information at the time of service as a best
practice.
• BH providers should use the Electronic Data Interchange 270/271 eligibility transaction, check
the payer portal, and exhaust any other sources for any TPP information on file, prior to
submitting a claim to Medicaid.
• BH providers are required to bill the TPP prior to billing Medicaid for all services except for the
service procedure codes listed on the BH Medicare and TPL Bypass List.
• BH providers should always notify ODM when they identify incorrect TPL information.
Benefits and Prior Authorization
In the behavioral health benefit package, there are services and/or levels of care that are subject to prior
authorization. Table 1-5 summarizes those services/levels of care and their associated prior authorization
policy.
Certain services may have prior authorization requirements when provided on the same day as
other services. Please refer to OAC Chapter 5160-27 and rule 5160-8-05 for service-specific
requirements.
22 | P a g e
Table 1-5: Prior Authorization
Description and Code
Benefit Period
Authorization Requirement
Assertive Community Treatment (ACT)
H0040
Based on prior
authorization
approval
ACT must be prior authorized and
SUD services above ASAM level
1 must be prior authorized for
ACT enrollees.
Intensive Home Based Treatment (IHBT) H2015
Functional Family Therapy (FFT) H2015 TF
1
Both services are
based on prior
authorization
approval
Both services must be prior
authorized.
SUD Partial Hospitalization
H0015 TG
Calendar year
Prior authorization is required for
this level of care for adults and
adolescents.
Psychiatric Diagnostic Evaluations
90791, 90792
Calendar year
1 encounter per person per
calendar year per code per billing
agency for 90791 and 90792. Prior
authorization is required for
additional service.
Psychological Testing
96112, 96113, 96116, 96121, 96130, 96131, 96132, 96133,
96136, 96137
Calendar year
Up to 20 hours/encounters per
patient per calendar year for all
psychological testing codes. Prior
authorization is required for
additional service.
Screening Brief Intervention and Referral to Treatment
(SBIRT) G0396, G0397
Calendar year
One of each code (G0396 and
G0397), per billing agency, per
patient, per year. Cannot be billed
by provider type 95. Prior
authorization is required for
additional service.
Alcohol or Drug Assessment H0001
Calendar year
2 assessments per patient per
calendar year per billing agency.
Does not count toward ASAM
level of care benefit limit. Prior
authorization is required for
additional service.
TBS Group Per Diem
H2020
Calendar year
1 per day. Prior authorization is
required for an additional per diem
service to the same client on the
same day rendered by a different
billing agency.

23 | P a g e
Description and Code
Benefit Period
Authorization Requirement
SUD Residential
H2034, H2036
Calendar year
Up to 30 consecutive days without
prior authorization. Prior
authorization then must support
the medical necessity of continued
stay, if not, only the initial 30
consecutive days are reimbursed.
This applies to first two stays.
Third and subsequent stays in the
same year require prior
authorization from the first day of
admission.
SUD Peer Recovery
H0038
Calendar year
Up to 4 hours per day without
prior authorization. Prior
authorization would be needed to
cover more than 4 hours in a day
once limit is reached.
MRSS Stabilization Service
S9482
Based on prior
authorization
approval
Prior Authorization is needed for
stabilization services rendered
more than six weeks from the
completion of a mobile response.
1
For dates of service between March 1, 2022 – June 30, 2022. Effective July 1, 2022, these services are
available only under OhioRISE
Fee for service prior authorization instructions are available on the ODM website -
http://medicaid.ohio.gov/PROVIDERS/PriorAuthorizationRequirements.aspx. Training on how to submit
a fee for service prior authorization request for a behavioral health service is available at
http://bh.medicaid.ohio.gov/training. Information regarding prior authorization requests for Medicaid
clients enrolled with a managed care or MyCare Ohio plan can be found in the Medicaid Managed Care
Plan Resource Guide.
Requirements for medical necessity are found here: OAC 5160-1-01
Non-Covered Services
Non-covered services are described in OAC rules 5160-1-61 and 5160-27-02 . Additionally, Ohio
Medicaid does not cover services to individuals that meet the criteria described in OAC rule 5160:1-1-03.
A missed appointment is considered a non-service and is not reimbursable by Ohio Medicaid as described
in OAC rule 5160-1-13.1.
Fraud, Waste, and Abuse
OAC rule 5160-1-29 sets forth the Ohio Medicaid policy on Medicaid Fraud, Waste, and Abuse. Under
the Ohio Medicaid provider agreement, providers are required to comply with the terms of the agreement,
Ohio Revised Code, Administrative Code, and federal statutes and rules. In Ohio, the Attorney General is
authorized under ORC 109.85 to create a Medicaid Fraud and Control Unit (MFCU) for investigating and

24 | P a g e
prosecuting Medicaid provider fraud in Ohio. Additional information regarding Ohio’s Medicaid Fraud
Control unit can be found on their website, Health Care Fraud - Ohio Attorney General Dave Yost.
Review of Provider Records
OAC rule 5160-1-27 sets forth the Ohio Medicaid policy on Review of Provider Records. Please review
this rule for more information about Ohio Medicaid audit and review activities.
Payment Error Rate Measurement (PERM)
The CMS Payment Error Rate Measurement (PERM) program measures and reports improper payments
in Medicaid and Children’s Health Insurance Program (CHIP). Please visit CMS’ PERM website for
more information.
Medicaid National Correct Coding Initiative
The National Correct Coding Initiative (NCCI) was established by the Centers for Medicare & Medicaid
Services (CMS) to promote national correct coding methodologies with the goal to reduce improper
coding that results in inappropriate payments for both Medicare and Medicaid. A complete and up-to-date
list of NCCI edits can be found at https://www.medicaid.gov/medicaid/program-integrity/national-
correct-coding-initiative/medicaid-ncci-edit-files/index.html. These edits are updated quarterly.
NCCI procedure-to-procedure (PTP) edits and medically unlikely edits (MUEs) are only applicable to a
single provider to a single individual on the same date of service. NCCI contains two types of edits:
NCCI Procedure-To-Procedure (PTP) Edits
PTP edits define pairs of Healthcare Common Procedure Coding System (HCPCS) / Current Procedural
Terminology (CPT) codes that should not be reported together for a variety of reasons. The purpose of the
PTP edits is to prevent improper payments when incorrect code combinations are reported.
Example 1: The same physician performs a psychotherapy service and Evaluation and Management
(E&M) service on the same day for the same client (significant and separately identifiable services).
NCCI will not allow the psychotherapy code 90834 to be billed with an E&M office visit code 99212, as
there are separate add-on codes (+90833, +90836, and +90838) for psychotherapy services provided in
conjunction with E&M services.
Example 2: A qualified practitioner working for ABC Behavioral Health Agency renders 90791, a
psychiatric diagnostic assessment, for a client. On the same day, the same client receives an “evaluation
and management” primary care service (e.g. 99202-99205) rendered by another qualified practitioner
working for ABC Behavioral Health Agency. According to the NCCI practitioner to practitioner (PTP)
edit guidance, this is acceptable because in this scenario, the services were rendered by two different
rendering practitioners. The NCCI PTP edits apply only to the same practitioner.
Medicaid PTP, MUE edits, and other relevant information can be found at:
https://www.medicaid.gov/medicaid/program-integrity/ncci/edit-files/index.html.
For PTP edits that have a Correct Coding Modifier Indicator (CCMI) of “0,” the codes should never be
reported together by the same provider for the same individual on the same date of service. If they are

25 | P a g e
reported on the same date of service, the column one code is eligible for payment and the column two
code is denied.
For PTP edits that have a CCMI of “1,” the codes may be reported together only in defined circumstances
which are identified on the claim by the use of specific NCCI-associated modifiers. Where services are
“separate and distinct,” it may be necessary to override the procedure-to-procedure edit using a specific
modifier:
• XE – “Separate encounter, A service that is distinct because it occurred during a separate
encounter” (This modifier should only be used to describe separate encounters on the same date
of service).
• XS – “Separate Structure, A service that is distinct because it was performed on a separate
organ/structure.”
• XP – “Separate Practitioner, A service that is distinct because it was performed by a different
practitioner.”
• XU – “Unusual Non-Overlapping Service, The use of a service that is distinct because it does not
overlap usual components of the main service.”
Documentation must support a different session, different procedure or surgery, different site or organ
system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive
injuries) not ordinarily encountered or performed on the same day by the same individual. However,
when another already established modifier is appropriate, it should be used rather than modifier 59.
Modifier 59 should only be utilized if no other more specific modifier is appropriate.
Medically Unlikely Edits (MUEs)
MUEs define for each HCPCS / CPT code the maximum units of service (UOS) that a provider would
report under most circumstances for a single individual on a single date of service. MUEs cannot be
overridden with the 59, XE, XS, XP, XU modifiers.
Example 1: The same physician performs two diagnostic evaluations (2 units of 90791) to the same client
on the same day. NCCI will deny the second evaluation, as it is medically unlikely that one client would
need two complete diagnostic evaluations in the same day.
There is extensive guidance regarding Medicaid agencies and national correct coding available at The
National Correct Coding Initiative in Medicaid.

26 | P a g e
Time-Based CPT Codes
When billing time-based codes, the CPT/HCPCS time rule applies, unless otherwise specified: For the
minimum billable service of the code, divide the time by two and add one minute in order to determine if
that code can be billed. For example; 90832 = 30 minutes, therefore the minimum length of service must
be 16 minutes (30/2 = 15 then 15 + 1 = 16) in order for the service to be billable.
Conversion Chart
Reported in 15 Minute Increments
Minimum
Maximum
Billing
Minutes
Minutes
Unit(s)
Hour 1
0
7
N/A
8
22
1
23
37
2
38
52
3
53
67
4
Hour 2
68
82
5
83
97
6
98
112
7
113
127
8
Hour 3
128
142
9
143
157
10
158
172
11
173
187
12
Hour 4
188
202
13
203
217
14
218
232
15
233
247
16
Prolonged Services
Effective January 1, 2023, the American Medical Association (AMA) discontinued prolonged service
codes 99354 and 99355 for use with psychotherapy codes. ODM and MCE billing systems were updated
to reflect this change. Providers should refer to AMA and National Correct Coding Initiative (NCCI)
guidance with regard to billing psychotherapy codes for dates of service on or after January 1, 2023.
Effective January 1, 2022, ODM adopted for Medicaid community behavioral health providers the use of
AMA procedure codes of 99415 and 99416 to indicate prolonged E&M services. Providers should refer to
the CPT manual for additional information about appropriate use of codes 99415 and 99416.
Also effective January 1, 2022, ODM’s claims payment system was updated to follow NCCI Procedure to
Procedure (PTP) edits to not allow the use of 99354 and 99355 with E&M codes 99202-99205 and
99211-99215.
Conversion Chart
Hour Based Services
Reported in Whole Unit Increments
Minimum Maximum Billing
Minutes Minutes Increment
1 30 N/A
31 90 1
91 150 2
151 210 3
211 270 4
271 330 5
331 390 6
391 450 7
451 510 8
511 570 9

27 | P a g e
Providers serving individuals with primary insurance coverage other than Medicaid are advised to follow
billing guidance for the primary payer when determining which prolonged services code to use before
submitting to Medicaid for secondary payment.
For more information regarding prolonged services codes, please review the prolonged services section of
the latest edition of the CPT manual. The link to the CPT website can be found here.
SECTION 2
Behavioral Health Services
For behavioral health billing, CPT service codes consist of E&M office visits, psychotherapy, psychiatric
diagnostic evaluations, psychiatric testing, and appropriate add-on codes. The American Medical
Association (AMA) publishes annual CPT reference books, which provide the CPT l codes, their
associated descriptions, and guidance on appropriate use, including use of add-on codes. Please note,
providers are responsible for utilizing the appropriate AMA and/or CMS guidance for documentation and
billing. Therefore, it is recommended that all providers obtain a copy of a current CPT manual and, for
those providers/practitioners that participate in the Original Medicare program, the most current guidance
is available through the Medicare Learning Network (MLN). This section also includes billing guidance
for HCPCS codes that are also available to both MH and SUD agencies. Practitioner abbreviations are
used in the service tables provided in the remaining sections of this manual. The chart below may be used
as a reference to these abbreviations.
Practitioner Abbreviations Key
MD/DO
Physician
LSW
Licensed social worker
CNS
Clinical nurse specialist
LMFT
Licensed marriage and family
therapist
CNP
Certified nurse practitioner
LPC
Licensed professional counselor
PA
Physician assistant
LCDC II or LCDC
III
Licensed chemical dependency
counselor II or III
RN
Registered nurse
SW-A
Social worker assistant
LPN
Licensed practical nurse
SW-T
Social worker trainee
PSY
Psychologist
MFT-T
Marriage and family therapist
trainee
LISW
Licensed independent social worker
C-T
Counselor trainee
LIMFT
Licensed independent marriage and family
therapist
CDC-A
Chemical dependency counselor
assistant
LPCC
Licensed professional clinical counselor
CMS
Care management specialist
LICDC
Licensed independent chemical
dependency counselor
QMHS
Qualified mental health specialist
Lic
school PSY
Board licensed school psychologist
QMHS +3
Qualified mental health specialist
with 3 years’ experience
PSY
assistant
Psychology assistant
PRS
Peer recovery supporter
RPH
Pharmacist

28 | P a g e
Evaluation and Management Codes
Table 2-1: Evaluation & Management Office Visit
MH / SUD
Service
Provider Type
Code
Rate through
December 31, 2023
Rate effective
January 1, 2024
E&M New Patient
MD/DO
99202
99203
99204
99205
$84.67
$122.93
$188.51
$236.92
$93.14
$135.22
$207.36
$260.61
CNS
CNP
PA
99202
99203
99204
99205
$84.67
$122.93
$188.51
$236.92
$93.14
$135.22
$207.36
$260.61
RPH
99202
99203
$33.09
$49.09
$35.08
$52.04
E&M Established
Patient
MD/DO
99211
99212
99213
99214
99215
$22.31
$48.97
$82.85
$122.27
$165.15
$24.54
$53.87
$91.14
$134.50
$181.67
CNS
CNP
PA
99211
99212
99213
99214
99215
$22.31
$48.97
$82.85
$122.27
$165.15
$24.54
$53.87
$91.14
$134.50
$181.67
RN
LPN
99211
$22.31
$24.54
RPH
99211
99212
99213
$12.32
$22.72
$37.06
$13.06
$24.42
$39.30
Unit Value
Encounter
Permitted POS
11, 13, 31, 32
MH also has 53
SUD also has 57
Telehealth allowed with GT modifier. GT modifier is required when
service rendered via telehealth.

29 | P a g e
Table 2-2: Prolonged Service codes for E&M Office Visits
MH / SUD
Service
Provider Type
Code
Rate through
December 31, 2023
Rate effective
January 1, 2024
Prolonged Visit –
First 60 minutes
MD/DO
CNS
CNP
PA
+99415
-
$12.03
Prolonged Visit –
Each Additional 30
Minutes
MD/DO
CNS
CNP
PA
+99416
-
$6.18
Prolonged Visit –
Each Additional 15
Minutes
(for use with codes
99205 and 99215
only)
MD/DO
+99417
$38.53
$42.38
CNS
CNP
PA
+99417
$38.53
$42.38
Prolonged Visit –
Each Additional 15
Minutes
(for use with codes
99205 and 99215
only)
MD/DO
+G2212
$38.53
$42.38
CNS
CNP
PA
+G2212
$38.53
$42.38
Unit Value
+99415 – first 60 minutes
+99416 – each additional 30 minutes
+99417 – each additional 15 minutes
+G2212 – each additional 15 minutes
Permitted POS
Same as base code
Telehealth allowed with GT modifier. GT modifier is required
when service rendered via telehealth.

30 | P a g e
Table 2-3 Evaluation and Management Office Visit - Report of Pregnancy
MH / SUD
Service
Provider Type
Code
Rate through
December 31, 2023
Rate effective
January 1, 2024
Report of
Pregnancy*
MD/DO
CNS
CNP
PA
T1023
$30.00
$30.00
HCPCS code T1023 is to be used for a “Report of Pregnancy” (ROP). Payment may be made for one
report of a pregnancy diagnosed in conjunction with an E&M service that is not associated with a normal
obstetrics/gynecology visit. The report must be submitted through NurtureOhio, available here:
https://progesterone.nurtureohio.com/login. The report of pregnancy must occur in conjunction with an
E&M service and be rendered by a physician, advanced practice registered nurse, or physician assistant.
The payment is paid in addition to the E&M visit.
To access the ROP on the NurtureOhio site, the user needs to have an OH|ID linked to their provider in
the PNM. For additional information and NurtureOhio login instructions, review the Provider User Guide
here: https://progesterone.nurtureohio.com/media/PRAFProviderUserGuide10-1-22.pdf.

31 | P a g e
Table 2-4: Evaluation & Management Home Visit
MH / SUD
Service
Provider
Type
Code
Rate through
December 31, 2023
Rate effective
January 1, 2024
E&M Home Visit
New Patient
MD/DO
99341
99342
99343*
99344
99345
$63.65
$91.90
$150.80
$210.7
$255.5
$70.02
$101.09
*
$231.86
$281.13
CNS
CNP
PA
99341
99342
99343*
99344
99345
$63.65
$91.90
$150.80
$210.78
$255.57
$70.02
$101.09
*
$231.86
$281.13
E&M Home Visit
Established
Patient
MD/DO
99347
99348
99349
99350
$64.00
$97.38
$148.16
$205.79
$70.40
$107.12
$162.98
$226.37
CNS
CNP
PA
99347
99348
99349
99350
$64.00
$97.38
$148.16
$205.79
$70.40
$107.12
$162.98
$226.37
Unit Value
Encounter
Permitted POS
04, 12, 16
*CPT® code 99343 has been deleted effective January 1, 2023. For dates of service on or after January 1,
2023, providers should report appropriate evaluation and management codes in accordance with the
AMA.

32 | P a g e
Table 2-5: Prolonged Service codes for E&M Home Visits
For dates of service prior to January 1, 2023*
MH / SUD
Service
Provider Type
Code
Rate
Prolonged Visit –
First 60 minutes
(Use in conjunction
with covered BH
codes 99341 -
99350)
MD/DO
+99354
$89.90
CNS
CNP
PA
+99354
$76.42
Prolonged Visit –
Each Additional 30
minutes
(Use in conjunction
with covered BH
codes 99341 -
99350)
MD/DO
+99355
$89.24
CNS
CNP
PA
+99355
$75.85
Unit Value
+99354 – first 60 minutes
+99355 – each additional 30 minutes
Permitted POS
Same as base code
Telehealth allowed with GT modifier. GT modifier is required when
service rendered via telehealth.
Table 2-6: Preventive Medicine Counseling
MH / SUD
Service
Provider Type
Code
Rates
Preventive
Medicine
Counseling – 15
minutes
MD/DO
CNS
CNP
PA
RPH
99401
For rates, see the Medicine, Surgery, Radiology and
Imaging, and Additional Procedures (Non-Institutional
Services) schedule on the Fee Schedule and Rates page
of the ODM website.
Preventive
Medicine
Counseling – 30
minutes
MD/DO
CNS
CNP
PA
RPH
99402
Unit Value
See code description
Permitted POS
Same as base code
Telehealth allowed with GT modifier. GT modifier is required when
service rendered via telehealth.

33 | P a g e
Table 2-7: Psychiatric Diagnostic Evaluation
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychiatric
Diagnostic
Evaluation w/o
Medical
MD/DO
PSY
90791
-
$130.72
$147.39
CNS
CNP
PA
90791
-
$130.72
$147.39
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
90791
$111.11
$125.28
LSW
LMFT
LPC
LCDC III (SUD only)
LCDC II (SUD only)
90791
U4
U5
U2
U3
U3
$111.11
$125.28
PSY assistant
90791
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included
SW-T
MFT-T
CDC-A (SUD only)
C-T
90791
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 72.25%
of maximum fee if
supervisor NPI not
included
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at
72.25% of maximum
fee if supervisor NPI
not included
Psychiatric
Diagnostic
Evaluation w/
Medical
MD/DO
90792
-
$144.35
$162.75
CNS
CNP
PA
90792
-
$144.35
$162.75
Unit Value
Encounter
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 31, 32, 99
MH also has 53
SUD also has 57
Telehealth allowed with GT modifier. GT
modifier is required when service rendered via
telehealth.

34 | P a g e
Table 2-8 – Electrocardiogram
MH / SUD
Service
Provider Type
Code
Rate through
December 31, 2023
Rate effective
January 1, 2024
Electrocardiogram- at
least 12 leads w/
interpretation and
report
MD/DO
93000
$15.90
$17.49
CNS
CNP
93000
$13.52
$14.87
PA
93000
$13.52
$14.87
Electrocardiogram-
tracing only w/o
interpretation and
report
MD/DO
93005
$6.90
$7.59
CNS
CNP
93005
$5.87
$6.45
PA
93005
$5.87
$6.45
Electrocardiogram-
interpretation and
report only
MD/DO
93010
$7.90
$8.69
CNS
CNP
93010
$6.72
$7.39
PA
93010
$6.72
$7.39
Unit Value
Encounter
Permitted POS
11
MH also has 53
SUD also has 57

35 | P a g e
Table 2-9: Provider Administered Pharmaceuticals
MH / SUD
Service
Medication
Code
Procedure
Modifier
Rate
Medication
Administered by
Medical Personnel
(J-Codes)
Injection, aripiprazole (Abilify), intramuscular,
0.25 mg
J0400
None
For rates, see the
Provider
Administered
Pharmaceuticals
schedule on the Fee
Schedule and Rates
page of the ODM
website.
Injection, aripiprazole (Abilify), 1 mg
J0401
None
Cogentin (benztropine mesylate), per 1 mg
J0515
None
Buprenorphine, oral, 1 mg
J0571
None
Diphenhydramine hcl (Benadryl), up to 50 mg
J1200
None
Haloperidol injection, up to 5 mg
J1630
None
Haloperidol Decanoate injection, per 50 mg
J1631
None
Injection, aristada initio, 1mg
J1943
None
Injection, aripiprazole lauroxil, 1 mg
J1944
None
Lorazepam injection, 2 mg
J2060
None
Injection, methylnaltrexone (Relistor), 0.1 mg
J2212
None
Injection, naloxone (Narcan), 1 mg
J2310
None
Injection, naloxone hydrochloride (zimhi),
1mg
J2311
None
Injection, naltrexone (Vivitrol), depot form,
1 mg
J2315
None
Olanzapine long acting injectable, 1 mg
J2358
None
Paliperidone Palmitate injection (Invega
Sustenna or Invega Trinza), 1 mg
J2426
None
Injection, Invega Hafyera/Trinza
J2427
None
Fluphenazine Decanoate injection, 25 mg
J2680
None
Risperidone, long acting, .5 mg
J2794
None
Naloxone (nasal route)
J3490
None
Valium injection, up to 5 mg
J3360
None
Oral Naltrexone
J8499
HG
Unit Value
Based on HCPCS descriptor
Unit Value
03, 04, 11, 12, 14
MH also has 53
SUD also has 55, 57

36 | P a g e
MH / SUD *
Service
Description
Provider
Type
Code
Rate through
December 31,
2023
Rate effective
January 1, 2024
Other Medication
Administration
Therapeutic,
prophylactic, or
diagnostic injection
(specify substance or
drug); subcutaneous or
intramuscular
MD/DO
CNS
CNP
PA
RN/LPN
RPH
*96372
$21.39
$23.53
Unit Value
CPT designation
Permitted POS
03, 04, 11, 12, 14, 16, 18
MH also has 53
SUD also has 57
* 96372 is not covered in substance use disorder (SUD) residential treatment programs (provider type 95
with provider specialty 954) due to the per diem payment methodology for SUD residential treatment.
National Drug Code (NDC)
Federal law requires that any claim detail line for a drug covered by Medicaid must be submitted with the
11-digit NDC assigned to each drug package. The NDC specifically identifies the manufacturer, product
and package size. Each NDC is an 11-digit number, sometimes including dashes in the format 55555-
4444-22. When submitting claims to Medicaid, providers should submit each NDC using the 11-digit
NDC without dashes or spaces. The NDC included on the claim must be the exact NDC that is on the
package used by the provider.
Some drug packages include a 10-digit NDC. In this case, the provider should convert the 10 digits to 11
digits when reporting this on the claim. When converting a 10-digit NDC to an 11-digit NDC, a leading
zero should be added to only one segment:
• If the first segment contains only four digits, add a leading zero to the segment;
• If the second segment contains only three digits, add a leading zero to the segment;
• If the third segment contains only one digit, add a leading zero to the segment.
All claims reporting NDC information must be submitted either as an Electronic Data Interchange (EDI)
transaction or through the Provider Network Management (PNM) module. The NDC will be required at
the detail level when a claim is submitted with a code that represents a drug (e.g., J-codes and Q-codes).

37 | P a g e
Laboratory Services
Table 2-10: Laboratory Services
MH / SUD
Service
Service
Code
Rate
Laboratory
Services
Skin test; tuberculosis,
intradermal
86580
For rates, see the Medicine, Surgery, Radiology and
Imaging, and Additional Procedures (Non-
Institutional Services) schedule on the Fee Schedule
and Rates page of the ODM website.
Collection of venous blood by
venipuncture
36415
Alcohol (ethanol), breath
82075
Urine pregnancy test
81025
Unit Value
CPT designation
Permitted POS
03, 04, 11, 12, 14
MH also has 53
SUD also has 55, 57
Other
Considerations
Code 36415 collection of venous blood by venipuncture may be billed for blood draws associated
with covered external lab services.
Laboratory Codes
Community substance use disorder (SUD) treatment providers (provider type 95) with appropriate CLIA
certification are provided the laboratory contract. This provides coverage for clinical laboratory services
provided on-site if the provider has the appropriate CLIA certificate for the clinical lab services being
performed. See ChapMedicaid-11 for Medicaid coverage policies related to laboratory services.
CLIA Certification Overview
To bill laboratory codes besides those listed above, a provider must obtain the appropriate CLIA
certification and enroll as a laboratory Medicaid provider with Ohio Medicaid. ODM must have the CLIA
certification on file for the SUD provider to access the appropriate laboratory codes. Once the certificate
is uploaded to the PNM, the appropriate laboratory contract will be made available to the SUD agency.
More information on the CLIA certification process can be found at:
https://odh.ohio.gov/wps/portal/gov/odh/home.

38 | P a g e
Vaccines
Ohio Medicaid allows BH providers to receive reimbursement for certain vaccines to their adult clients
and to children under the Vaccines for Children program, operated by the Ohio Department of Health
(ODH). Vaccines are covered when administered at the following places of service: office, inpatient and
outpatient residential facilities, in the community, and Community Mental Health Centers (CMHC).
The Vaccines for Children (VFC) program is a federally funded program overseen by the Centers for
Disease Control and Prevention (CDC) and administered by ODH. More information about the VFC
program can be found on ODH’s website and CDC’s website.
Table 2-11: Covered Vaccines for Behavioral Health Providers
Vaccine
Administration Code
Description
90460
Immunization administration through 18 years of age via any route of administration, with
counseling by physician or other health care professional; first or only component of each
vaccine or toxoid administered
90471
Immunization administration (includes percutaneous, intradermal, or intramuscular
injections); 1 vaccine (single or combination vaccine/toxoid)
+90472 (add-on to
90471)
Immunization administration; each additional vaccine. List separately in addition to code
for primary procedure
90473
Administration of 1 nasal or oral vaccine
90474
Immune administration oral or nasal additional
Vaccine CPT
Description
90633
Hepatitis A vaccine (HepA), pediatric/adolescent dosage-2 dose schedule, for intramuscular
use
90634
Hepatitis A vaccine (HepA), pediatric/adolescent dosage-3 dose schedule, for intramuscular
use
90632
Hepatitis A vaccine (HepA), adult dosage, for intramuscular use
90371
Hepatitis B immune globulin (HBIg), human, for intramuscular use
90650
Human Papillomavirus vaccine, types 16, 18, bivalent (2vHPV), 3 dose schedule, for
intramuscular use
90649
Human Papillomavirus vaccine, types 6, 11, 16, 18, quadrivalent (4vHPV), 3 dose schedule,
for intramuscular use
90644
Vaccine for meningococcal and Hemophilus influenza B (4 dose schedule) injection into
muscle, children 6 weeks-18 months of age
90698
Diphtheria, tetanus toxoids, acellular pertussis vaccine, Haemophilus influenza type b, and
inactivated poliovirus vaccine (DTaP-IPV/Hib), for intramuscular use
90654
Influenza virus vaccine, trivalent (IIV3), split virus, preservative-free, for intradermal use
90658
Vaccine for influenza for administration into muscle, 0.5 ml dosage
90660
Influenza virus vaccine, trivalent, live (LAIV3), for intranasal use
90670
Pneumococcal conjugate vaccine, 13 valent (PCV13), for intramuscular use
90680
Rotavirus vaccine, pentavalent (RV5), 3 dose schedule, live, for oral use
90681
Rotavirus vaccine, human, attenuated (RV1), 2 dose schedule, live, for oral use

39 | P a g e
Vaccine CPT
Description
90696
Diphtheria, tetanus toxoids, acellular pertussis vaccine and inactivated poliovirus vaccine
(DTaP-IPV), when administered to children 4 through 6 years of age, for intramuscular use
90713
Poliovirus vaccine, inactivated (IPV), for subcutaneous or intramuscular use
90707
Measles, mumps and rubella virus vaccine (MMR), live, for subcutaneous use
90710
Measles, mumps, rubella, and varicella vaccine (MMRV), live, for subcutaneous use
90714
Tetanus and diphtheria toxoids adsorbed (Td), preservative free, when administered to
individuals 7 years or older, for intramuscular use
90715
Tetanus, diphtheria toxoids and acellular pertussis vaccine (Tdap), when administered to
individuals 7 years or older, for intramuscular use
90716
Varicella virus vaccine (VAR), live, for subcutaneous use
90736
Shingles vaccine (HZV), live, for subcutaneous injection (individuals 60+ years old)
90732
Pneumococcal polysaccharide vaccine, 23-valent (PPSV23), adult or immunosuppressed
patient dosage, when administered to individuals 2 years or older, for subcutaneous or
intramuscular use
90733
Meningococcal polysaccharide vaccine, serogroups A, C, Y, W-135, quadrivalent
(MPSV4), for subcutaneous use
90734
Vaccine for meningococcus for administration into muscle
90740
Hepatitis B vaccine (HepB), dialysis or immunosuppressed patient dosage, 3 dose schedule,
for intramuscular use
90746
Hepatitis B vaccine (HepB), adult dosage, 3 dose schedule, for intramuscular use
90747
Hepatitis B vaccine (HepB), dialysis or immunosuppressed patient dosage, 4 dose schedule,
for intramuscular use
90759
Hepatitis B vaccine (HepB) 10 mcg dosage, 3 dose schedule, for intramuscular use
For rates, see the Medicine, Surgery, Radiology and Imaging, and Additional Procedures (Non-Institutional Services)
schedule on the Fee Schedule and Rates page of the ODM website.
For rates and coding information regarding COVID-19 vaccine counseling and administration, please refer to the ODM
COVID-19 resource page for guidance.
COVID-19 Vaccine Administration
Please refer to the ODM COVID-19 resource page for COVID-19 vaccine administration guidance.
Vaccines for Children (VFC) Program
Ohio’s Vaccines for Children Program is administered by the Ohio Department of Health. For more
information about the program and eligibility criteria for children visit the ODH website resources here:
• Vaccines for Children (VFC) | Ohio Department of Health
• ODH VFC FAQs

40 | P a g e
Vaccines for Adults
Each year, the Advisory Committee on Immunization Practices (ACIP) approves immunization schedules
recommended for persons living in the United States. The adult immunization schedule provides a
summary of ACIP recommendations on the use of licensed vaccines routinely recommended for adults
aged 19 years or older. The adult immunization schedule is also approved by the American College of
Physicians (ACP), the American Academy of Family Physicians (AAFP), the American College of
Obstetricians and Gynecologists (ACOG), and the American College of Nurse-Midwives (ACNM).
Medicaid may not cover all recommended vaccinations. See Table 2-11 above for the list of covered
vaccines for behavioral health providers.
Child and Adolescent Needs Strengths (CANS) Assessment
The CANS is completed at prescribed intervals or whenever there is a significant change in a member's
condition or circumstances. CANS assessors should aim to conduct minimally invasive practice and
maintain the best interest of youth/caregivers throughout the assessment process. Accordingly, assessors
should not over-assess youth/caregivers or ask them to tell their stories multiple times. The Ohio
Children’s Initiative CANS assessment and the state CANS IT system supports the practice of building
upon what we already know about the youth/caregiver’s story and avoiding over-assessment. Prior to
engaging the youth/caregiver in the CANS assessment process, the CANS assessors should access the
CANS IT System to determine if a recent CANS assessment has been completed with the
youth/caregiver. If a recent CANS assessment is available in the CANS IT system, the assessor should
use their professional judgment to determine if an update needs to occur or if the most recent assessment
can be used.
The Ohio Children’s Initiative CANS was launched for use in October 2021. While waiting for the
system work necessary to identify this as a stand-alone service, ODM issued interim billing guidance that
allowed for billing of community psychiatric supportive treatment (CPST), therapeutic behavioral service
(TBS), and/or psychiatric diagnostic evaluation for administration of a CANS assessment. Beginning July
1, 2022, the Ohio Children’s Initiative CANS assessment may only be billed using the H2000 code.
CPST, TBS, and/or psychiatric diagnostic evaluation may no longer be billed for administration of a
CANS assessment for dates of service on/after July 1, 2022.
Requirements for Billing:
• Rendering practitioner must be appropriately certified and trained in the administration of the
Ohio Children’s Initiative CANS assessment
• The rendering practitioner must have an NPI, be enrolled in Medicaid, add the “ORC” specialty
to the individual Ohio Medicaid enrollment and be affiliated with the billing provider (add
specialty by sending email request to MEDICAID_PROV[email protected])
• CANS assessments must be entered in Ohio’s CANS IT system to establish and maintain
OhioRISE eligibility

41 | P a g e
Table 2-12: Child and Adolescent Needs and Strengths (CANS) Assessment
MH/SUD
Requires the addition of the “ORC” specialty to the rendering provider’s enrollment
Service
Rendering
Provider Type
Code
Practitioner
Modifier
Rate
(dates of service
7/1/2022-
12/31/2022)
Rate
(dates of service
1/1/2023-
12/31/2023)
Rate effective
January 1,
2024
Child and
Adolescent
Needs and
Strength
(CANS)
Assessment
MD/DO
H2000
*
$341.60
$527.25
$594.47
PA
CNS
CNP
H2000
*
$211.74
$324.67
$366.07
PSY
LPCC
LISW
LIMFT
LICDC
Lic school PSY
H2000
*
$112.86
$170.43
$192.16
LPC
LSW
LMFT
LCDC II
LCDC III
H2000
*
$109.38
$165.00
$186.04
PSY assistant
SW-A
SW-T
MFT-T
C-T
CDC-A
QMHS
CMS
H2000
*
$98.31
$147.72
$166.55
Unit Value
Per Assessment (Brief or Comprehensive)
Permitted POS
Any valid place of service code may be used
Billing
Instructions
• If the CANS is completed over multiple dates of service, the claim date of service is the date the
CANS was completed
• Telehealth allowed with GT modifier. GT modifier is required when service rendered via
telehealth.
Diagnosis code is required – any valid ICD-10 diagnosis code may be used, including “Z-codes”
*For individuals with a primary enrollment in Medicaid as one of the allowable provider types listed in
Table 2-12 above, a practitioner modifier is not required. However, a practitioner modifier (see Table 1-3)
may be required if an individual is enrolled with additional specialties and the primary enrollment is not
one of the allowable provider types listed above. Please refer to the “Modifiers” worksheet found in the
“Dual Licensure Grid” at bhmedicaid.ohio.gov for additional information.
The CANS billing Table 2-12 above is specific to those services billed by Ohio Medicaid Provider types
84, 95, and OhioRISE Care Management Entities (CME). Other relevant billing providers will follow the
claims submission policies consistent with their billing provider type.

42 | P a g e
Mobile Response and Stabilization Service (MRSS)
Information about service descriptions, eligibility, clinical criteria, and limitations can be found in OAC
rules 5160-27-13 (ODM) and 5122-29-14 (OhioMHAS). The MRSS Practice Standards and other
provider resources can be found on the OhioMHAS MRSS site: https://mha.ohio.gov/community-
partners/early-childhood-children-and-youth/resources/mobile-response-stabilization-services.
Requirements for Billing:
• Addition of the “ORM” specialty to the primary Ohio Medicaid billing provider type
• The rendering practitioner must have an NPI, be enrolled in Medicaid, and be affiliated with
the billing provider
• MRSS hourly and 15-minute codes cannot be billed for time spent administering a CANS
assessment during an MRSS event

43 | P a g e
Table 2-13: MRSS Crisis Mobile Response
MH/SUD
Requires the billing provider have the “ORM” specialty
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Crisis Mobile Response
PSY
LPCC
LISW
LIMFT
Licensed school
PSY
LICDC
S9485
*
$476.64
$537.41
LPC
LSW
LMFT
LCDC II
LCDC III
S9485
*
$466.34
$525.80
PSY assistant
SW-A
SW-T
MFT-T
C-T
CDC-A
QMHS
CMS
S9485
*
$432.63
$487.79
PRS
S9485
*
$365.55
$412.16
Unit Value
Per diem
Permitted POS
Any valid place of service code may be used
Billing Information
• Billed on the date the initial mobile response is initiated by the MRSS provider; or
to report the MRSS team’s first encounter after the crisis response is initiated**
• Code can be billed by all practitioners participating in the initial mobile response
• May not be billed more than once in the Mobile Response period
• Do not use for follow-up after the initial mobile response
• Diagnosis code is required – any valid ICD-10 code may be used, including “Z-
codes”
• Telehealth allowed in accordance with MRSS practice standards - GT modifier is
required when service rendered via telehealth
*For individuals with a primary enrollment in Medicaid as one of the allowable provider types listed in
Table 2-13 above, a practitioner modifier is not required. However, a practitioner modifier (see Table 1-3)
may be required if an individual is enrolled with additional specialties and the primary enrollment is not
one of the allowable provider types listed above. Please refer to the “Modifiers” worksheet found in the
“Dual Licensure Grid” at bhmedicaid.ohio.gov for additional information.

44 | P a g e
** For MRSS providers using an external entity that is not part of the MRSS billing provider agency to
support 24/7 coverage, as allowed during an MRSS provider’s first year of initial certification, there may
be situations where the external entity initiates the crisis response prior to handing off to the MRSS
provider. When this occurs, the MRSS provider will use the initial Crisis Mobile Response code S9485 to
report services provided during the MRSS team’s first encounter with the youth/family after hand-off
from the external entity who initiated the crisis response. If the external entity is a Medicaid provider, the
external entity may bill for any Medicaid-covered services rendered prior to handing-off to the MRSS
team (e.g. psychotherapy for crisis). After the first encounter by the MRSS team reported using the initial
Crisis Mobile Response code S9485, subsequent services rendered by the MRSS team during the mobile
response phase are billed using the Crisis Mobile Response Follow-up code, S9484.
Table 2-13 is specific to Community BH Agency (Ohio Medicaid PT 84 and 95) billing. Hospitals
certified to provide this service should use the code set and billing instructions for Outpatient Hospital
Behavioral Health Services.

45 | P a g e
Table 2-14: MRSS Crisis Mobile Response Follow Up
MH/SUD
Requires the billing provider have the “ORM” specialty
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Crisis Mobile Response
Follow-Up
PSY
LPCC
LISW
LIMFT
Licensed school
PSY
LICDC
S9484
*
$139.92
$157.76
LPC
LSW
LMFT
LCDC II
LCDC III
S9484
*
$136.49
$153.89
PSY assistant
SW-A
SW-T
MFT-T
C-T
CDC-A
QMHS
CMS
S9484
*
$125.25
$141.22
PRS
S9484
*
$102.89
$116.01
Unit Value
Per hour
Permitted POS
Any valid place of service code may be used
Billing Information
• Billed for follow-up activities during the mobile response phase (up to 72 hours
from the initial mobile response)
• Dates of service should be within 3 calendar days of the initial mobile response
• The initial mobile response (S9485) code must be billed before this code can be
billed
• Code can be billed by all practitioners participating in the follow up response
• Can be billed on the same date of service as the initial response if the initial
response concluded and follow-up activities were provided later the same date
• Code may not be billed for time spent administering the CANS assessment
• Diagnosis code is required – any valid ICD-10 code may be used, including “Z-
codes”
• Telehealth allowed - GT modifier is required when service rendered via telehealth.
*For individuals with a primary enrollment in Medicaid as one of the allowable provider types listed in
Table 2-14 above, a practitioner modifier is not required. However, a practitioner modifier (see Table 1-3)
may be required if an individual is enrolled with additional specialties and the primary enrollment is not

46 | P a g e
one of the allowable provider types listed above. Please refer to the “Modifiers” worksheet found in the
“Dual Licensure Grid” at bhmedicaid.ohio.gov for additional information.
Table 2-14 is specific to Community BH Agency (Ohio Medicaid PT 84 and 95) billing. Hospitals
certified to provide this service should use the code set and billing instructions for Outpatient Hospital
Behavioral Health Services.
Table 2-15: MRSS Stabilization Service
MH/SUD
Requires the billing provider have the “ORM” specialty
Service
Rendering
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
MRSS Stabilization Service
PSY
LPCC
LISW
LIMFT
Licensed school PSY
LICDC
S9482
*
$34.95
$39.41
LPC
LSW
LMFT
LCDC II
LCDC III
S9482
*
$34.01
$38.35
PSY assistant
SW-A
SW-T
MFT-T
C-T
CDC-A
QMHS
CMS
S9482
*
$30.92
$34.86
PRS
S9482
*
$24.77
$27.93
Unit Value
Per 15 minutes
Permitted POS
Any valid place of service code may be used
Billing Information
• The initial mobile response (S9485) code must be billed before this code can be
billed
• Code can be billed by all practitioners providing the stabilization service
• Requires prior authorization to extend beyond 6 weeks from the end of the de-
escalation phase
• Cannot be billed for youth enrolled in IHBT, MST, FFT or ACT
• Code may not be billed for time spent administering the CANS assessment
• Diagnosis code is required – any valid ICD-10 code may be used, including “Z-
codes”
• Telehealth allowed - GT modifier is required when service rendered via telehealth
*For individuals with a primary enrollment in Medicaid as one of the allowable provider types listed in
Table 2-15 above, a practitioner modifier is not required. However, a practitioner modifier (see Table 1-3

47 | P a g e
Behavioral Health Manual) may be required if an individual is enrolled with additional specialties and the
primary enrollment is not one of the allowable provider types listed above. Please refer to the “Modifiers”
worksheet found in the “Dual Licensure Grid” at bhmedicaid.ohio.gov for additional information.
Table 2-15 is specific to Community BH Agency (Ohio Medicaid PT 84 and 95) billing. Hospitals
certified to provide this service should use the code set and billing instructions for Outpatient Hospital
Behavioral Health Services.

48 | P a g e
SECTION 3
Psychotherapy Services
Table 3-1: Psychotherapy for Crisis
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychotherapy for
Crisis – first 60
minutes
MD/DO
PSY
90839
-
$171.70
$193.59
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
90839
-
$145.95
$164.55
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
90839
U4
U5
U2
U3
U3
$145.95
$164.55
PSY assistant
90839
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD only)
C-T
90839
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.

49 | P a g e
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychotherapy for
Crisis – add’l 30
minutes
MD/DO
PSY
+90840
-
$81.95
$92.40
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
+90840
-
$69.65
$78.54
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
+90840
U4
U5
U2
U3
U3
$69.65
$78.54
PSY assistant
+90840
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD only)
C-T
+90840
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Unit Value
+90839: 1 which represents first 60 minutes
+90840: 1 which represents each additional 30 minutes
Permitted POS
01, 03, 04, 11, 12, 13, 14, 15, 16, 17, 18, 20,
23, 24, 25, 31, 32, 33, 34, 41, 42, 99
MH also has 53
SUD also has 57
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.

50 | P a g e
Table 3-2: Individual Psychotherapy
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Individual
Psychotherapy –
30 minutes
MD/DO
PSY
90832
-
$63.11
$82.04 (KX)
$71.16
$92.50 (KX)
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
90832
-
$53.64
$69.73 (KX)
$60.49
$78.63 (KX)
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
90832
U4
U5
U2
U3
U3
$53.64
$69.73 (KX)
$60.49
$78.63 (KX)
PSY assistant
90832
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included (both KX
and non-KX).
Paid at direct
supervisor rate
when supervisor
NPI on claim. Paid
at 85% of maximum
fee if supervisor
NPI not included.
(both KX and non-
KX).
SW trainee
MFT trainee
CDC-A (SUD only)
C-T
90832
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included (both KX
and non-KX).
Paid at direct
supervisor rate
when supervisor
NPI on claim. Paid
at 72.25% of
maximum fee if
supervisor NPI not
included. (both KX
and non-KX).

51 | P a g e
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Individual
Psychotherapy –
45 minutes
MD/DO
PSY
90834
-
$82.05
$92.51
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
90834
-
$69.74
$78.63
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
90834
U4
U5
U2
U3
U3
$69.74
$78.63
PSY assistant
90834
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate
when supervisor
NPI on claim. Paid
at 85% of maximum
fee if supervisor
NPI not included.
SW trainee
MFT trainee
CDC-A (SUD only)
C-T
90834
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate
when supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Individual
Psychotherapy –
60+ minutes
MD/DO
PSY
90837
-
$120.36
$135.71
CNS
CNP
PA
90837
-
$102.31
$115.35

52 | P a g e
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Individual
Psychotherapy –
60+ minutes
(continued)
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
90837
-
$102.31
$115.35
LSW
LMFT
LPC
LCDC III (SUD
only) LCDC II
(SUD only)
90837
U4
U5
U2
U3
U3
$102.31
$115.35
PSY assistant
90837
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included
Paid at direct
supervisor rate
when supervisor
NPI on claim. Paid
at 85% of maximum
fee if supervisor
NPI not included
SW-T
MFT-T
CDC-A (SUD only)
C-T
90837
U9
UA
U6
U7
Paid at direct
supervisor rate when
Supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate
when Supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Individual
Psychotherapy w/
E&M Service
MD/DO
+90833
+90836
+90838
-
$65.37
$83.03
$109.53
$73.70
$93.62
$123.50
CNS
CNP
PA
+90833
+90836
+90838
-
$55.56
$70.58
$93.10
$62.65
$79.58
$104.98
Unit Value
1 which represents encounter
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 31, 32, 34, 99
MH also has 53
SUD also has 57
For 90832 KX – POS 23 is also available
Telehealth allowed with GT modifier. 90832
KX telehealth allowed with GT modifier. GT
modifier is required when service rendered
via telehealth.
Crisis
psychotherapy of
16 to 30 minutes
Add KX modifier to 90832 to indicate when service is crisis psychotherapy between 16 and 30
minutes, as allowable within the practitioner’s scope of practice. For crisis psychotherapy of 31
or more minutes, please use crisis psychotherapy coding above.

53 | P a g e
Table 3-3: Family Psychotherapy
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through December
31, 2023
Rate effective
January 1, 2024
Family
Psychotherapy
w/o patient –
50 minutes
MD/DO
PSY
90846
-
$102.28
$115.32
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD
only)
Lic school
PSY
90846
-
$86.94
$98.02
LSW
LMFT
LPC
LCDC III
(SUD only)
LCDC II
(SUD only)
90846
U4
U5
U2
U3
U3
$86.94
$98.02
PSY assistant
90846
U1
Paid at direct supervisor rate
when supervisor NPI on
claim. Paid at 85% of
maximum fee if supervisor
NPI not included.
Paid at direct supervisor
rate when supervisor
NPI on claim. Paid at
85% of maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD
only)
C-T
90846
U9
UA
U6
U7
Paid at direct supervisor rate
when supervisor NPI on
claim
Paid at 72.25% of maximum
fee if supervisor NPI not
included.
Paid at direct supervisor
rate when supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Family
psychotherapy
(conjoint, w/
patient
present) – 50
minutes
MD/DO
PSY
90847
-
$100.72
$113.56

54 | P a g e
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through December
31, 2023
Rate effective
January 1, 2024
Family
psychotherapy
(conjoint, w/
patient
present) – 50
minutes
(continued)
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD
only)
Lic school
PSY
90847
-
$85.61
$96.53
LSW
LMFT
LPC
LCDC III
(SUD only)
LCDC II
(SUD only)
90847
U4
U5
U2
U3
U3
$85.61
$96.53
PSY assistant
90847
U1
Paid at direct supervisor rate
when supervisor NPI on
claim. Paid at 85% of
maximum fee if supervisor
NPI not included.
Paid at direct supervisor
rate when supervisor
NPI on claim. Paid at
85% of maximum fee if
supervisor NPI not
included.
SW trainee
MFT trainee
CDC-A (SUD
only)
C-T
90847
U9
UA
U6
U7
Paid at direct supervisor rate
when supervisor NPI on
claim
Paid at 72.25% of maximum
fee if supervisor NPI not
included.
Paid at direct supervisor
rate when supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Multiple-
family group
psychotherapy
MD/DO
PSY
90849
-
$40.66
$45.84
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD
only)
Lic school
PSY
90849
-
$34.57
$38.96

55 | P a g e
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through December
31, 2023
Rate effective
January 1, 2024
Multiple-
family group
psychotherapy
(continued)
LSW
LMFT
LPC
LCDC III
(SUD only)
LCDC II
(SUD only)
90849
U4
U5
U2
U3
U3
$34.57
$38.96
PSY assistant
90849
U1
Paid at direct supervisor rate
when supervisor NPI on
claim. Paid at 85% of
maximum fee if supervisor
NPI not included.
Paid at direct supervisor
rate when supervisor
NPI on claim. Paid at
85% of maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD
only)
C-T
90849
U9
UA
U6
U7
Paid at direct supervisor rate
when supervisor NPI on
claim
Paid at 72.25% of maximum
fee if supervisor NPI not
included.
Paid at direct supervisor
rate when supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Unit Value
1 which represents an encounter
Permitted
POS
03, 04, 11, 12, 13, 14, 16, 31, 32, 34
MH also has 53
SUD also has 57
For 90846 and 90847 – 99 is also
available
Telehealth allowed with GT modifier. GT modifier is
required when service rendered via telehealth.

56 | P a g e
Table 3-4: Prolonged Service Codes for Psychotherapy
Rate through December 31, 2022*
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through December
31, 2022
Prolonged Visit – First 60
minutes
(Use in conjunction with
covered BH codes 90837,
90847)
MD/DO
PSY
+99354
-
$89.90
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
+99354
-
$76.42
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
+99354
U4
U5
U2
U3
U3
$76.42
PSY assistant
+99354
U1
Paid at direct supervisor rate
when supervisor NPI on
claim. Paid at 85% of
maximum fee if supervisor
NPI not included.
SW-T
MFT-T
C-T
CDC-A (SUD only)
+99354
U9
UA
U7
U6
Paid at direct supervisor rate
when supervisor NPI on claim
Paid at 72.25% of maximum
fee if supervisor NPI not
included.

57 | P a g e
Prolonged Visit – Each
Additional 30 Minutes
(Use in conjunction with
covered BH codes 90837,
90847)
MD/DO
PSY
+99355
-
$89.24
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
+99355
-
$75.85
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
+99355
U4
U5
U2
U3
U3
$75.85
PSY assistant
+99355
U1
Paid at direct supervisor rate
when supervisor NPI on
claim. Paid at 85% of
maximum fee if supervisor
NPI not included.
SW-T
MFT-T
C-T
CDC-A (SUD only)
+99355
U9
UA
U7
U6
Paid at direct supervisor rate
when supervisor NPI on claim
Paid at 72.25% of maximum
fee if supervisor NPI not
included.
Unit Value
+99354 – first 60 minutes
+99355 – each additional 30 minutes
Permitted POS
Same as base code
Telehealth allowed with GT modifier. GT modifier is
required when service rendered via telehealth.
*CPT® codes 99354 and 99355 have been deleted effective January 1, 2023. Providers can refer to AMA
and NCCI guidance with regard to billing psychotherapy for dates of service on or after January 1, 2023.

58 | P a g e
Table 3-5: Group Psychotherapy
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Group
Psychotherapy
(not multi-
family group)
MD/DO
PSY
90853
-
$33.09
$37.31
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD
only)
Lic school PSY
90853
-
$28.12
$31.71
LSW
LMFT
LPC
LCDC III (SUD
only)
LCDC II (SUD
only)
90853
U4
U5
U2
U3
U3
$28.12
$31.71
PSY assistant
90853
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD only)
C-T
90853
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 72.25%
of maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 72.25%
of maximum fee if
supervisor NPI not
included.
Unit Value
1 which represents an encounter
Permitted POS
03, 04, 11, 12, 13, 14, 16, 31, 32, 34, 99
MH also has 53
SUD also has 57
Telehealth allowed with GT modifier. GT
modifier is required when service rendered via
telehealth.

59 | P a g e
Interactive Complexity
The use of interactive complexity codes is further described in CPT guidance. For more information,
please reference the CPT book.
Table 3-6: Interactive Complexity
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Interactive
Complexity
MD/DO
PSY
+90785
-
$13.81
$15.57
CNS
CNP
PA
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
+90785
-
$11.74
$13.23
LSW
LMFT
LPC
LCDC III (SUD only)
LCDC II (SUD only)
+90785
U4
U5
U2
U3
U3
$11.74
$13.23
PSY assistant
+90785
U1
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD only)
C-T
+90785
U9
UA
U6
U7
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Interactive Complexity is an add-on code that is only valid in conjunction with codes as determined by the AMA.
Unit Value
1 which represents an encounter
Permitted
POS
POS must be the same
as the base code to
which interactive
complexity is being
added.
Telehealth allowed with GT modifier for dates of service on and after
November 15, 2020. GT modifier is required on claim when service rendered
via telehealth.

60 | P a g e
Psychological Testing
The use of psychological testing codes is further described in CPT guidance. For more information,
please reference the CPT book.
Table 3-7: Psychological Testing
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychological
Testing
Administration
MD/DO
PSY
PA
CNS
CNP
LISW
LIMFT
LPCC
Lic school
PSY
96136
-
$30.86
$34.79
LSW
LMFT
LPC
PSY assistant
96136
U4
U5
U2
U1
$30.86
$34.79
SW-T
MFT-T
C-T
96136
U9
UA
U7
$30.86
$34.79
MD/DO
PSY
PA
CNS
CNP
LISW
LIMFT
LPCC
Lic school
PSY
+96137
-
$28.39
$32.01

61 | P a g e
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychological
Testing
Administration
(continued)
LSW
LMFT
LPC
PSY assistant
+96137
U4
U5
U2
U1
$28.39
$32.01
SW-T
MFT-T
C-T
+96137
U9
UA
U7
$28.39
$32.01
Psychological
Testing Evaluation
MD/DO
PSY
PA
CNS
CNP
LISW
LIMFT
LPCC
Lic school
PSY
96130
-
$59.26
$66.82
LSW
LMFT
LPC
PSY assistant
96130
U4
U5
U2
U1
$59.26
$66.82
SW-T
MFT-T
C-T
96130
U9
UA
U7
$59.26
$66.82

62 | P a g e
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychological
Testing Evaluation
(continued)
MD/DO
PSY
PA
CNS
CNP
LISW
LIMFT
LPCC
Lic school
PSY
+96131
-
$59.26
$66.82
LSW
LMFT
LPC
PSY assistant
+96131
U4
U5
U2
U1
$59.26
$66.82
SW-T
MFT-T
C-T
+96131
U9
UA
U7
$59.26
$66.82
Developmental
Testing
MD/DO
PSY
CNS
CNP
PA
LISW
LIMFT
LPCC
Lic school
PSY
96112
-
$56.11
$63.26
LSW
LMFT
LPC
PSY assistant
96112
U4
U5
U2
U1
$56.11
$63.26
SW-T
MFT-T
C-T
96112
U9
UA
U7
$56.11
$63.26

63 | P a g e
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Developmental
Testing
(continued)
MD/DO
PSY
CNS
CNP
PA
LISW
LIMFT
LPCC
Lic school
PSY
+96113
-
$28.06
$31.64
LSW
LMFT
LPC
PSY assistant
+96113
U4
U5
U2
U1
$28.06
$31.64
SW-T
MFT-T
C-T
+96113
U9
UA
U7
$28.06
$31.64
Neurobehavioral
Status Exam
MD/DO
PA
PSY
CNS
CNP
96116
-
$64.10
$72.27
PSY assistant
96116
U1
$64.10
$72.27
MD/DO
PA
PSY
CNS
CNP
+96121
-
$64.10
$72.27
PSY assistant
+96121
U1
$64.10
$72.27

64 | P a g e
MH / SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Neuropsychological
Testing
Administration
MD/DO
PA
PSY
CNS
CNP
96136
-
$30.86
$34.79
PSY assistant
96136
U1
$30.86
$34.79
MD/DO
PA
PSY
CNS
CNP
+96137
-
$28.39
$32.01
PSY assistant
+96137
U1
$28.39
$32.01
Neuropsychological
Testing Evaluation
MD/DO
PA
PSY
CNS
CNP
96132
-
$97.37
$109.78
PSY assistant
96132
U1
$97.37
$109.78
MD/DO
PA
PSY
CNS
CNP
+96133
-
$78.31
$88.29
PSY assistant
+96133
U1
$78.31
$88.29
Unit Value
96112, 96116, 96130, 96132: first 60 minutes
96136: first 30 minutes
+96113, +96137: additional 30 minutes
+96121, +96131, +96133: additional 60 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 31
MH also has 53
SUD also has 57
Telehealth allowed with GT modifier. GT
modifier is required when service rendered via
telehealth.

65 | P a g e
Table 3-7.5: Smoking Cessation
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Smoking and
Tobacco Use
Cessation
Counseling –
Intermediate:
Greater than 3
minutes and up
to 10 minutes
MD/DO
PSY
99406
-
$9.43
$10.37
CNS
CNP
PA
99406
-
$9.43
$10.37
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
99406
-
$8.02
$8.81
LSW
LMFT
LPC
LCDC III (SUD only)
LCDC II (SUD only)
99406
U4
U5
U2
U3
U3
$8.02
$8.81
PSY assistant
99406
U1
Paid at direct supervisor
rate when supervisor
NPI on claim. Paid at
85% of maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD only)
C-T
99406
U9
UA
U6
U7
Paid at direct supervisor
rate when supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
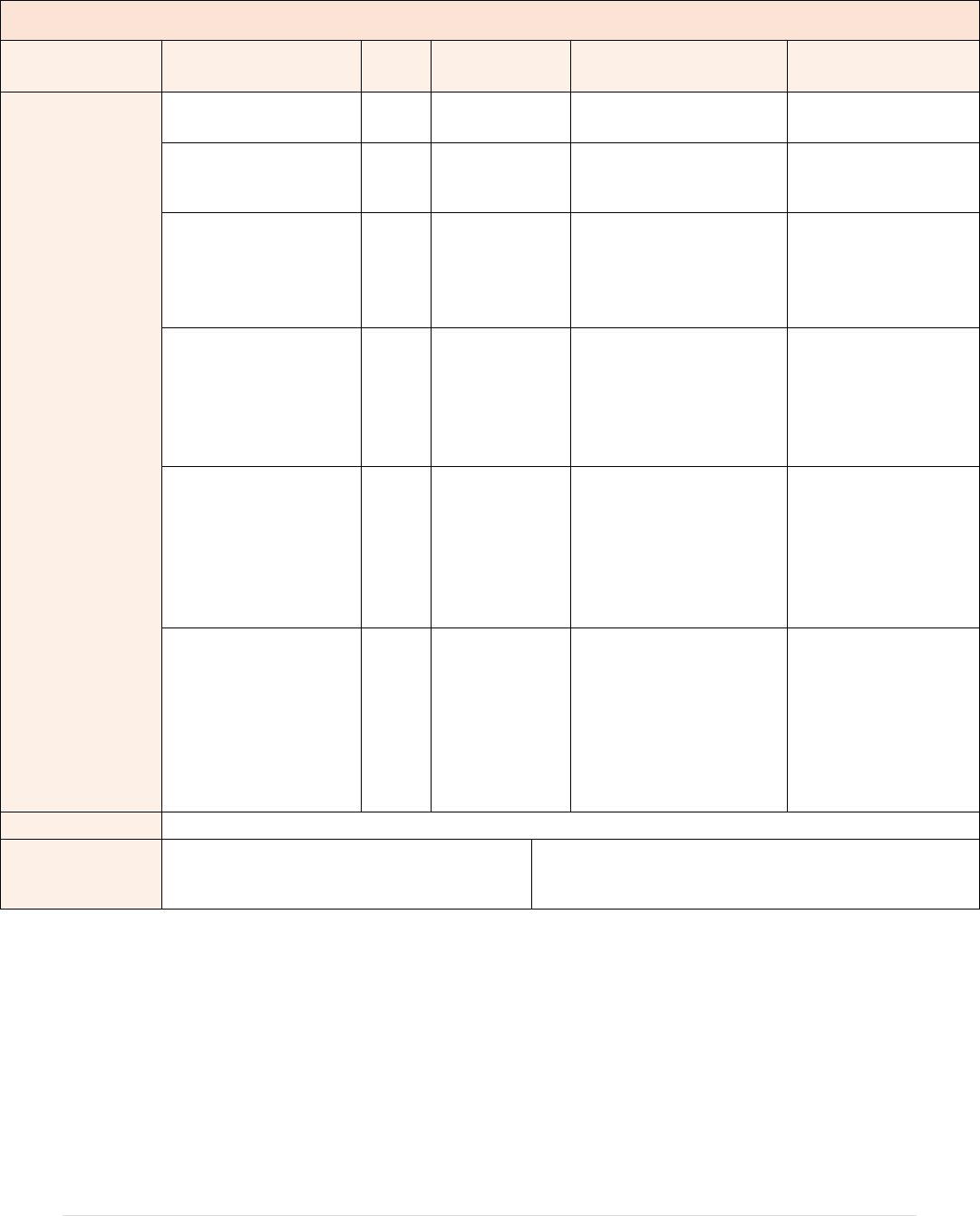
66 | P a g e
MH / SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Smoking and
Tobacco Use
Cessation
Counseling –
Intensive:
Greater than 10
minutes
MD/DO
PSY
99407
-
$19.00
$20.90
CNS
CNP
PA
99407
-
$19.00
$20.90
LISW
LIMFT
LPCC
LICDC (SUD only)
Lic school PSY
99407
-
$16.15
$17.77
LSW
LMFT
LPC
LCDC III (SUD only)
LCDC II (SUD only)
99407
U4
U5
U2
U3
U3
$16.15
$17.77
PSY assistant
99407
U1
Paid at direct supervisor
rate when supervisor
NPI on claim. Paid at
85% of maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim. Paid at 85% of
maximum fee if
supervisor NPI not
included.
SW-T
MFT-T
CDC-A (SUD only)
C-T
99407
U9
UA
U6
U7
Paid at direct supervisor
rate when supervisor
NPI on claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Paid at direct
supervisor rate when
supervisor NPI on
claim
Paid at 72.25% of
maximum fee if
supervisor NPI not
included.
Unit Value
1 which represents an encounter
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 31, 32, 34, 99
MH also has 53
SUD also has 57
Telehealth allowed with GT modifier. GT modifier is
required when service rendered via telehealth.

67 | P a g e
Healthcare Common Procedure Coding System (HCPCS) Mental Health Services
Table 3-8: Therapeutic Behavioral Services (TBS)
MH
Individual Therapeutic Behavioral Services (TBS) – 15 minutes
Service Code
Provider Type
Code
Modifiers
Rate through
December 31, 2023
Rate effective January
1, 2024
Individual
Therapeutic
Behavioral
Services (TBS) –
15 minutes
MD/DO
CNS
CNP
PA
PSY
LISW
LIMFT
LPCC
Lic school PSY
H2019
-
$22.47 in office
$28.59 in community
$29.21 in office (KX)
$37.17 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)
LSW
LMFT
LPC
H2019
U4
U5
U2
$22.47 in office
$28.59 in community
$29.21 in office (KX)
$37.17 (KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)
PSY assistant
(Master’s)
H2019
U1 and HO
$22.47 in office
$28.59
$29.21 in office (KX)
$37.17 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)
SW-T
(Master’s)
H2019
U9 and HO
$22.47 in office
$28.59 in community
$29.21 in office (KX)
$37.17 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)
SW-T
(Bachelor’s)
H2019
U9 and HN
$19.96 in office
$25.46 in community
$25.95 in office (KX)
$33.10 in community
(KX)
$22.50 in office
$28.71 in community
$29.26 in office (KX)
$37.32 in community (KX)
SW-A
(Master’s)
H2019
U8 and HO
$22.47 in office
$28.59 in community
$29.21 in office (KX)
$37.17 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)

68 | P a g e
Individual
Therapeutic
Behavioral
Services (TBS) –
15 minutes
(continued)
SW-A
(Bachelor’s)
H2019
U8 and HN
$19.96 in office
$25.46 in community
$25.95 in office (KX)
$33.10 in community
(KX)
$22.50 in office
$28.71 in community
$29.26 in office (KX)
$37.32 in community (KX)
MFT-T
(Master’s)
H2019
UA and
HO
$22.47 in office
$28.59 in community
$29.21 in office (KX)
$37.17 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)
MFT trainee
(Bachelor’s)
H2019
UA and
HN
$19.96 in office
$25.46 in community
$25.95 in office (KX)
$33.10 in community
(KX)
$22.50 in office
$28.71 in community
$29.26 in office (KX)
$37.32 in community (KX)
C-T
(Master’s)
H2019
U7 and HO
$22.47 in office
$28.59 in community
$22.47 in office (KX)
$28.59 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)
C-T
(Bachelor’s)
H2019
U7 and HN
$19.96 in office
$25.46 in community
$25.95 in office (KX)
$33.10 in community
(KX)
$22.50 in office
$28.71 in community
$29.26 in office (KX)
$37.32 in community (KX)
QMHS
(Bachelor’s)
H2019
HN
$19.96 in office
$25.46 in community
$25.95 in office (KX)
$33.10 in community
(KX)
$22.50 in office
$28.71 in community
$29.26 in office (KX)
$37.32 in community (KX)
QMHS
(Master’s)
H2019
HO
$22.47 in office
$28.59 in community
$29.21 in office (KX)
$37.17 in community
(KX)
$25.33 in office
$32.24 in community
$32.93 in office (KX)
$41.91 in community (KX)

69 | P a g e
Individual
Therapeutic
Behavioral
Services (TBS) –
15 minutes
(continued)
QMHS (3 yrs+
Exp.)
H2019
UK
$19.96 in office
$25.46 in community
$25.95 in office (KX)
$33.10 in community
(KX)
$22.50 in office
$28.71 in community
$29.26 in office (KX)
$37.32 in community (KX)
Group Therapeutic Behavioral Services (TBS) – 15 minutes
Service Code
Provider Type
Code
Modifiers
Rate through
December 31, 2023
Rate effective January
1, 2024
Group
Therapeutic
Behavioral
Services (TBS) –
15 minutes
MD/DO
CNS
CNP
PA
PSY
LISW
LIMFT
LPCC
Lic school PSY
H2019
HQ
$8.99
$10.14
LSW
LMFT
LPC
H2019
U4, HQ
U5, HQ
U2, HQ
$8.99
$10.14
PSY assistant
(Master’s)
H2019
U1, HO
HQ
$7.31
$8.24
SW-T (Master’s)
H2019
U9, HO
HQ
$7.31
$8.24
SW-T
(Bachelor’s)
H2019
U9, HN
HQ
$6.49
$7.32
SW-A
(Master’s)
H2019
U8, HO
HQ
$7.31
$8.24
PSY assistant
(Bachelor’s)
H2019
U1, HN,
HQ
$6.49
$7.32
SW-A
(Bachelor’s)
H2019
U8, HN
HQ
$6.49
$7.32
MFT-T
(Master’s)
H2019
UA, HO
HQ
$7.31
$8.24
MFT-T
(Bachelor’s)
H2019
UA, HN
HQ
$6.49
$7.32
C-T
(Master’s)
H2019
U7, HO
HQ
$7.31
$8.24
C-T
(Bachelor’s)
H2019
U7, HN
HQ
$6.49
$7.32

70 | P a g e
Group
Therapeutic
Behavioral
Services (TBS) –
15 minutes
(continued)
QMHS
(Bachelor’s)
H2019
HN
HQ
$6.49
$7.32
QMHS
(Master’s)
H2019
HO
HQ
$7.31
$8.24
QMHS (3 yrs+
Exp.)
H2019
UK
HQ
$6.49
$7.32
Unit Value
15 minutes
Permitted POS
Individual TBS – 03, 04, 11, 12, 13, 14,
16, 18, 23, 31, 32, 34, 53, 99
Group TBS – 11, 53
If more than six (6) units are delivered
on the same date of service by the same
agency in places of service 11 and/or 53,
subsequent units will be paid at 50% of
the above rates.
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.
TBS to address
a crisis
Add KX modifier to indicate TBS provided when a patient is experiencing a crisis, as allowable
within the practitioner’s scope of practice.
t
Table 3-9: RN and LPN Nursing Services
MH
Service
Provider
Type
Code
Procedure
Modifier
Rate through
December 31, 2023
Rate effective January
1, 2024
Nursing Services
– Individual
RN
H2019
-
$31.92 in office
$41.00 in community
$35.99 in office
$46.23 in community
LPN
H2017
-
$22.54 in office
$29.13 in community
$25.41 in office
$32.84 in community
Nursing Services
– Group
RN
H2019
HQ
$10.37
$11.69
Unit Value
15 minutes
Permitted POS
Individual RN/LPN nursing services - 03,
04, 11, 12, 13, 14, 16, 18, 31, 32, 34, 53, 99
Group RN nursing services – 11, 53
For H2019 KX – POS 23 is also available.
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.
RN nursing
service to
address a crisis
Add KX modifier to indicate RN nursing service provided when a patient is experiencing a crisis,
as allowable within the practitioner’s scope of practice. KX is not allowable with group RN
nursing services (HQ modifier).

71 | P a g e
Table 3-10: TBS Group Service-Hourly and Per Diem (Day Treatment)
MH
Service Code
Provider Type
Code
Modifiers
Rate through
December 31, 2023
Rate effective
January 1, 2024
TBS Group
Service (Day
Treatment) per
hour less than 2.5
hours (See hour-
based services,
pg. 27)
PSY
H2012
HK
HQ
$36.53
$41.19
LISW
LIMFT
LPCC
Lic school PSY
H2012
HK
HQ
$36.53
$41.19
LSW
LMFT
LPC
H2012
U4, HK, HQ
U5, HK, HQ
U2, HK, HQ
$36.53
$41.19
PSY assistant
(Master’s)
SW-T (Master’s)
SW-A (Master’s)
MFT-T (Masters)
C-T (Master’s)
QMHS (Master’s)
H2012
U1, HO, HQ
U9, HO, HQ
U8, HO, HQ
UA, HO, HQ
U7, HO, HQ
HO, HQ
$27.37
$30.86
PSY asst
(Bachelor’s)
SW-T (Bachelor’s)
SW-A (Bachelor’s)
MFT-T
(Bachelor’s)
C-T (Bachelor’s)
QMHS
(Bachelor’s)
H2012
U1, HN, HQ
U9, HN, HQ
U8, HN, HQ
UA, HN, HQ
U7, HN, HQ
HN, HQ
$24.10
$27.17
QMHS (3 yrs+
Exp.)
H2012
UK, HQ
$24.10
$27.17

72 | P a g e
TBS Group
Service (Day
Treatment)
2.5 or more hours
(per diem)
Provider Type
Code
Modifiers
Rate through
December 31, 2023
Rate effective
January 1, 2024
PSY
H2020
HK
$182.66
$205.95
LISW
LIMFT
LPCC
Lic school PSY
H2020
HK
$182.66
$205.95
LSW
LMFT
LPC
H2020
U4,HK
U5,HK
U2,HK
$182.66
$205.95
PSY assistant
(Master’s)
SW-T (Master’s)
SW-A (Master’s)
MFT-T (Master’s)
C-T (Master’s)
QMHS (Master’s)
H2020
U1,HO
U9,HO
U8,HO
UA,HO
U7,HO
HO
$152.17
$171.57
PSY asst
(Bachelor’s)
SW-T (Bachelor’s)
SW-A (Bachelor’s)
MFT-T
(Bachelor’s)
C-T (Bachelor’s)
QMHS
(Bachelor’s)
H2020
U1,HN
U9,HN
U8,HN
UA,HN
U7,HN
HN
$135.92
$153.25
QMHS (3 yrs+
Exp.)
H2020
UK
$135.92
$153.25
Unit Value
H2012: Hourly, maximum of 2 per day
H2020: Per diem
Permitted POS
03, 04, 11, 14, 53
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.

73 | P a g e
Table 3-11: Psychosocial Rehabilitation (PSR)
MH
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Psychosocial
Rehabilitation
SW-T
H2017
U9 and HM
$15.84 in office
$20.32 in community
$20.59 (KX) in office
$26.42 (KX) in
community
$17.86 in office
$22.91 in community
$23.22 (KX) in office
$29.79 (KX) in
community
SW-A
H2017
U8 and HM
$15.84 in office
$20.32 in community
$20.59 (KX) in office
$26.42 (KX) in
community
$17.86 in office
$22.91 in community
$23.22 (KX) in office
$29.79 (KX) in
community
MFT-T
H2017
UA and HM
$15.84 in office
$20.32 in community
$20.59 (KX) in office
$26.42 (KX) in
community
$17.86 in office
$22.91 in community
$23.22 (KX) in office
$29.79 (KX) in
community
C-T
H2017
U7 and HM
$15.84 in office
$20.32 in community
$20.59 (KX) in office
$26.42 (KX) in
community
$17.86 in office
$22.91 in community
$23.22 (KX) in office
$29.79 (KX) in
community
QMHS (high
school)
H2017
HM
$15.84 in office
$20.32 in community
$20.59 (KX) in office
$26.42 (KX) in
community
$17.86 in office
$22.91 in community
$23.22 (KX) in office
$29.79 (KX) in
community
QMHS
(Associate’s)
H2017
HM
$15.84 in office
$20.32 in community
$20.59 (KX) in office
$26.42 (KX) in
community
$17.86 in office
$22.91 in community
$23.22 (KX) in office
$29.79 (KX) in
community
Unit Value
15 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 23, 31, 32, 34,
53, 99
If more than six (6) units are delivered on the
same date of service by the same agency in
places of service 11 and/or 53, subsequent
units will be adjudicated at 50% of the above
rates.
Telehealth allowed with GT modifier.
GT modifier is required when service
rendered via telehealth. HM modifier is
required when billing PSR to differentiate
PSR and MH LPN nursing.

74 | P a g e
MH
PSR to address a
crisis
Add KX modifier to indicate PSR provided when a patient is experiencing a crisis, as allowable
within the practitioner’s scope of practice.
Table 3-12: Screening, Brief Intervention and Referral to Treatment
MH
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Screening, Brief
Intervention and
Referral to
Treatment
(SBIRT)
MD/DO
CNS
CNP
PA
PSY
RN
LPN
LISW
LIMFT
LPCC
Lic school PSY
G0396
-
$25.05
$27.56
LSW
LMFT
LPC
G0396
U4
U5
U2
$25.05
$27.56
PSY assistant
SW-T
MFT-T
C-T
G0396
U1
U9
UA
U7
$25.05
$27.56
Screening, Brief
Intervention and
Referral to
Treatment
(SBIRT)
MD/DO
CNS
CNP
PA
PSY
RN
LPN
LISW
LIMFT
LPCC
Lic school PSY
G0397
-
$47.68
$52.45
LSW
LMFT
LPC
G0397
U4
U5
U2
$47.68
$52.45
PSY assistant
SW-T
MFT-T
C-T
G0397
U1
U9
UA
U7
$47.68
$52.45
Unit Value
G0396: Encounter from 15 to 30 minutes
G0397: Encounter over 30 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 31, 32, 53
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.

75 | P a g e
Table 3-13: Community Psychiatric Supportive Treatment (CPST)
MH
Service
Provider Type
Code
Practitioner
Modifier
Procedure
Modifier
Rate through
December 31,
2023
Rate effective
January 1,
2024
Community
Psychiatric
Supportive
Treatment –
Individual
MD/DO
H0036
-
-
$19.54
$22.03
CNS
CNP
PA
PSY
H0036
-
-
$19.54
$22.03
LISW
LIMFT
LPCC
Lic school PSY
H0036
-
-
$19.54
$22.03
LSW
LMFT
LPC
H0036
U4
U5
U2
-
$19.54
$22.03
PSY assistant
SW-T
SW-A
MFT-T
C-T
H0036
U1
U9
U8
UA
U7
-
$19.54
$22.03
QMHS (3 yrs+
Exp.)
QMHS (high
school)
QMHS
(Associate’s)
QMHS
(Bachelor’s)
QMHS
(Master’s)
H0036
UK
HM
HM
HN
HO
-
$19.54
$22.03
Community
Psychiatric
Supportive
Treatment –
Group
MD/DO
H0036
-
HQ
$8.99
$10.14
CNS
CNP
PA
PSY
H0036
-
HQ
$8.99
$10.14

76 | P a g e
MH
Service
Provider Type
Code
Practitioner
Modifier
Procedure
Modifier
Rate through
December 31,
2023
Rate effective
January 1,
2024
Community
Psychiatric
Supportive
Treatment –
Group
(continued)
LISW
LIMFT
LPCC
Lic school PSY
H0036
-
HQ
$8.99
$10.14
LSW
LMFT
LPC
H0036
U4
U5
U2
HQ
$8.99
$10.14
PSY assistant
SW-T
SW-A
MFT-T
C-T
H0036
U1
U9
U8
UA
U7
HQ
$8.99
$10.14
QMHS (3 yrs+
Exp.)
QMHS (high
school)
QMHS
(Associate’s)
QMHS
(Bachelor’s)
QMHS
(Master’s)
H0036
UK
HM
HM
HN
HO
HQ
$8.99
$10.14
Unit Value
15 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 23, 31, 32,
33, 34, 53, 99
If more than six (6) units are delivered on
the same date of service by the same
agency, subsequent units will be
adjudicated at 50% of the above rates.
Telehealth allowed with GT modifier. GT modifier is
required when service rendered via telehealth.

77 | P a g e
Assertive Community Treatment (ACT)
Table 3-14: Assertive Community Treatment (ACT)
MH
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Assertive
Community
Treatment
MD/DO
H0040
AM
$615.64
$694.13
CNP
CNS
PA
H0040
UC
SA
SA
$352.75
$397.73
Licensed
practitioner
*
H0040
HO
$251.91
$284.03
Unlicensed
practitioner
H0040
HN
$199.70
$225.16
Peer recovery
supporter
H0040
HM
$159.24
$179.54
Unit Value
1 representing a per diem
Permitted POS
03, 04, 11, 12, 13, 14, 16, 17, 18, 20, 53, 99
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.
*Please refer to Ohio Administrative Code 5160-27-04(L) (2) for information on which practitioners are
included in this level.

78 | P a g e
Intensive Home Based Treatment (IHBT)
For information on billing IHBT, refer to the OhioRISE Provider Enrollment and Billing Guidance.
SECTION 4
Substance Use Disorder (SUD) Coverage
OAC rule 5160-27-09 establishes the American Society of Addiction Medicine (ASAM) placement
criteria as the standard for Ohio Medicaid coverage of substance use disorder treatment services. The
SUD services described in this section are covered when provided by eligible providers as defined in
5160-27-01.
Table 4-1: SUD Assessment
SUD
Service
Provider
Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
SUD Assessment
PSY assistant
H0001
U1
$77.22
$87.07
SW-T
H0001
U9
$77.22
$87.07
MFT-T
H0001
UA
$77.22
$87.07
CDC-A
H0001
U6
$77.22
$87.07
C-T
H0001
U7
$77.22
$87.07
Unit Value
Encounter
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 23, 31, 32, 34,
57, 99
Telehealth allowed with GT modifier. GT
modifier is required when service rendered via
telehealth.

79 | P a g e
Table 4-2: SUD Peer Recovery Support
SUD
Service
Provider
Type
Code
Practitioner
Modifier
Procedure
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
SUD
Individual
Peer
Recovery
Support
PRS
H0038
HM, HN, HO
-
$15.51
$17.49
SUD Group
Peer
Recovery
Support
PRS
H0038
HM, HN, HO
HQ
$1.94
$2.19
Unit Value
15 minutes
Permitted
POS
03, 04, 11, 12, 13,
14, 16, 18, 23, 31,
32, 33, 34, 53, 57,
99
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via telehealth.
Table 4-3: Individual Counseling
SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31,
2023
Rate effective
January 1,
2024
Individual
Counseling
PSY assistant
H0004
U1
$19.31
$25.10 (KX)
$21.77
$28.30 (KX)
SW-T
H0004
U9
$19.31
$25.10 (KX)
$21.77
$28.30 (KX)
MFT-T
H0004
UA
$19.31
$25.10 (KX)
$21.77
$28.30 (KX)
CDC-A
H0004
U6
$19.31
$25.10 (KX)
$21.77
$28.30 (KX)
C-T
H0004
U7
$19.31
$25.10 (KX)
$21.77
$28.30 (KX)
Unit Value
15 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 31, 32, 34,
57, 99
H0004 KX - POS 23 also available
Telehealth allowed with GT modifier. GT
modifier is required when service rendered via
telehealth.
Individual
counseling to
address a crisis
Add KX modifier to indicate behavioral health counseling provided when a patient is
experiencing a crisis, as allowable within the practitioner’s scope of practice.

80 | P a g e
Table 4-4: Group Counseling
SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Group
Counseling
MD/ DO
H0005
AF
$11.02
$12.43
CNS
CNP
PA
PSY
LISW
LIMFT
LPCC
LICDC
H0005
HK
$9.37
$10.56
LSW
LMFT
LPC
LCDC III, LCDC II
H0005
U4 and HK
U5 and HK
U2 and HK
U3 and HK
$9.37
$10.56
PSY assistant
H0005
U1
$8.37
$9.44
SW-T
H0005
U9
$8.37
$9.44
MFT-T
H0005
UA
$8.37
$9.44
CDC-A
H0005
U6
$8.37
$9.44
C-T
H0005
U7
$8.37
$9.44
Unit Value
15 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 31, 32, 34, 57
and
99
Telehealth allowed with GT modifier. GT modifier
is required when service rendered via telehealth.

81 | P a g e
Table 4-5: SUD Case Management
SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
SUD Case
Management
MD/DO
H0006
-
$19.54
$22.03
CNS
CNP
PA
PSY
H0006
-
$19.54
$22.03
LISW
LIMFT
LPCC
LICDC
Lic school PSY
H0006
-
$19.54
$22.03
LSW
LMFT
LPC
LCDC II or LCDC
III
H0006
U4
U5
U2
U3
$19.54
$22.03
PSY assistant
H0006
U1
$19.54
$22.03
SW-T
H0006
U9
$19.54
$22.03
SW-A
H0006
U8
$19.54
$22.03
MFT-T
H0006
UA
$19.54
$22.03
CDC-A
H0006
U6
$19.54
$22.03
C-T
H0006
U7
$19.54
$22.03
CMS high school
CMS Associate’s
CMS Bachelor’s
CMS Master’s
H0006
HM
HM
HN
HO
$19.54
$22.03
Unit Value
15 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 18, 23, 31, 32, 33, 34, 57, 99
If more than six (6) units are delivered on the same date
of service by the same agency, subsequent units will be
adjudicated at 50% of the above rates.
Telehealth allowed with GT
modifier. GT modifier is required
when service rendered via telehealth.

82 | P a g e
Table 4-6: SUD Drug Screening
SUD
Service
Provider Type
Code
Practitioner
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Non-blood
specimen collection
for alcohol/other
drug testing
MD/DO
CNS
CNP
PA
RN, LPN
PSY
LISW
LIMFT
LPCC
LICDC
Lic school PSY
H0048
-
$14.48
$16.33
LSW
LMFT
LPC
LCDC III, LCDC II
H0048
U4
U5
U2
U3
$14.48
$16.33
PSY assistant
SW-T
SW-A
MFT-T
CDC-A
C-T
CMS high school
CMS Associate’s
CMS Bachelor’s
CMS Master’s
H0048
U1
U9
U8
UA
U6
U7
HM
HM
HN
HO
$14.48
$16.33
Unit Value
Encounter
Permitted POS
11, 57

83 | P a g e
Table 4-7: SUD RN and LPN Nursing Services
SUD
Service
Provider
Type
Code
Modifier
Rate through
December 31, 2023
Rate effective January
1, 2024
Nursing
Services –
Individual
RN
T1002
-
$31.92 –in office
$41.00 –in community
$35.99 - in office
$46.23 - in community
LPN
T1003
-
$22.54
$29.13
$25.41
$32.84
Nursing
Services –
Group
RN
T1002
HQ
$10.37
$11.69
Unit Value
15 minutes
Permitted
POS
Individual RN/LPN nursing services - 03,
04, 11, 12, 13, 14, 16, 18, 31, 32, 33, 34,
57, 99
Group RN nursing services – 11 and 57
For T1002 KX – POS 23 is also available
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.
RN nursing
service to
address a
crisis
Add KX modifier to indicate RN nursing service provided when a patient is experiencing a crisis, as
allowable within the practitioner’s scope of practice. KX is not allowable with group RN nursing
services (HQ modifier).

84 | P a g e
Table 4-8: Intensive Outpatient Level of Care Group Counseling
SUD
Service
Provider Type
Code
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Group
Counseling IOP
Level of Care*
MD/DO
CNS
CNP
PA
PSY
H0015
HK
$149.88
$168.99
LISW
LIMFT
LPCC
LICDC
H0015
HK
$149.88
$168.99
LSW
LMFT
LPC
LCDC III, LCDC II
H0015
U4, HK
U5, HK
U2, HK
U3, HK
$149.88
$168.99
PSY assistant
SW-T
MFT-T
CDC-A
C-T
H0015
U1
U9
UA
U6
U7
$103.04
$116.18
Unit Value
Per diem. For IOP group counseling when provided to a client for a minimum length of 2 hours.
and 1 minute.
Permitted POS
03, 04, 11, 14, 16, 57
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.
* When practitioners are co-facilitating an IOP group counseling service, it is up to the agency to determine under which
practitioner to bill, to ensure billing for this per diem service is not duplicative, and to ensure the practitioner to patient
ratio of no more than 1:12 is maintained.

85 | P a g e
Table 4-9: Partial Hospitalization (PH) Level of Care Group Counseling
*When practitioners are co-facilitating a PH group counseling service, it is up to the agency to determine
under which practitioner to bill, to ensure billing for this per diem service is not duplicative, and to ensure
the practitioner to patient ratio of no more than 1:12 is maintained.
SUD
Service
Provider
Type
Code
Practitioner
Modifier
Procedure
Modifier
Rate through
December 31,
2023
Rate effective
January 1,
2024
Group
Counseling
PH Level of
Care*
MD/DO
CNS
CNP
PA
PSY
H0015
HK
TG
$224.82
$253.48
LISW
LIMFT
LPCC
LICDC
H0015
HK
TG
$224.82
$253.48
LSW
LMFT
LPC
LCDC III
LCDC II
H0015
U4, HK
U5, HK
U2, HK
U3, HK
U3, HK
TG
$224.82
$253.48
PSY assistant
SW-T
MFT-T
CDC-A
C-T
H0015
U1
U9
UA
U6
U7
TG
$154.56
$174.27
Unit Value
Per diem. For PH group counseling when provided to a client for a minimum length of 3 hours and 1
minute.
Permitted
POS
03, 04, 11, 14, 16, 57
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via telehealth.

86 | P a g e
Table 4-10: SUD Withdrawal Management with Extended On Site Monitoring
SUD
Service
Provider Type
Code
Procedure
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Withdrawal
Management
Hourly ASAM 2
WM
RN
H0014
-
$127.68
$143.96
RN
H0014
AT
$338.35
$381.49
LPN
H0014
-
$90.16
$101.66
LPN
H0014
AT
$238.92
$269.38
Withdrawal
Management Per
Diem ASAM 2
WM
MD/DO
CNS
CNP
PA
H0012
-
$360.36
$406.31
Unit Value
H0012: Per diem
H0014: 1 hour
H0014 AT: 2-3 hours
Permitted POS
11, 55, 57
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.
SECTION 5
SUD Residential Treatment
Providers must be certified by OhioMHAS for residential and withdrawal management substance use
disorder services to bill for SUD residential treatment. Providers must have the ODM provider specialty
“954 – SUD RESIDENTIAL FACILITY” for provider type “95 – OMHAS CERTIFIED/LICENSED
TREATMENT PROGRAM” to bill using the SUD residential treatment benefit package.
In order to bill a SUD residential per diem at least one documented face-to-face service must be provided
by one of the clinical/treatment team members to the patient at the SUD residential treatment program
site. Per diem payments do not include room and board.
SUD Withdrawal Management with Extended On Site Monitoring
For information on billing Withdrawal Management Per Diem ASAM 2 WM, refer to Table 4-10 (SUD
Withdrawal Management with Extended On Site Monitoring)

87 | P a g e
Table 5-1: Clinically Managed Low-Intensity Residential Treatment
SUD
Service
Provider Type
Code
Rate through December
31, 2023
Rate effective January 1,
2024
Clinically
Managed Low-
Intensity
Residential
Treatment ASAM
3.1
Any
independently
licensed
practitioner with
an SUD scope of
practice
H2034
$152.57
$172.02
Unit Value
Per diem
Permitted POS
55
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via telehealth.
Table 5-2: Clinically Managed Residential Withdrawal Management
SUD
Service
Provider Type
Code
Rate through
December 31, 2023
Rate effective January 1,
2024
Clinically
Managed
Withdrawal
Management
ASAM 3.2 WM
Any
independently
licensed
practitioner with
an SUD scope of
practice
H0010
$256.33
$289.01
Unit Value
Per diem
Permitted POS
55
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via telehealth.

88 | P a g e
Table 5-3: Clinically Managed Population-Specific High Intensity Residential Treatment
(Adults)
SUD
Service
Provider Type
Code
Procedure
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Clinically Managed
Population-Specific
High Intensity
Residential
Treatment ASAM
3.3 (Adults)
Any
independently
licensed
practitioner with
an SUD scope of
practice
H2036
HI
$213.70
$240.95
Unit Value
Per diem
Permitted POS
55
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.
Table 5-4: Clinically Managed High Intensity Residential Treatment
SUD
Service
Provider
Type
Code
Rate through December
31, 2023
Rate effective January 1,
2024
Clinically Managed
High Intensity
Residential
Treatment ASAM
3.5
Any
independently
licensed
practitioner with
an SUD scope
of practice
H2036
$213.70
$240.95
Unit Value
Per diem
Permitted POS
55
Telehealth allowed with GT modifier.
GT modifier is required when service
rendered via telehealth.

89 | P a g e
Table 5-5: Medically Monitored Intensive Inpatient Treatment (Adults) and Medically
Monitored High-Intensity Inpatient Services (Adolescent)
SUD
Service
Provider Type
Code
Procedure
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Medically
Monitored
Intensive Inpatient
Treatment (Adults)
and Medically
Monitored High-
Intensity Inpatient
Services
(Adolescent)
ASAM 3.7
Any
independently
licensed
practitioner with
an SUD scope of
practice
H2036
TG
$303.49
$342.18
Unit Value
Per diem
Permitted POS
55
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.
Table 5-6: Medically Monitored Inpatient Withdrawal Management
SUD
Service
Provider
Type
Code
Rate through December 31,
2023
Rate effective January 1,
2024
Medically
Monitored
Inpatient
Withdrawal
Management
ASAM 3.7
WM
Any
independently
licensed
practitioner with
an SUD scope
of practice
H0011
$392.86
$442.95
Unit Value
Per diem
Permitted
POS
55
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.

90 | P a g e
SECTION 6
Opioid Treatment Programs
This section includes services provided by Opioid Treatment Programs (OTPs) licensed by OhioMHAS
as a methadone administration program and/or certified by the Substance Abuse and Mental Health
Services Administration (SAMHSA) as an OTP.
Provider Network Management (PNM) Enrollment for Opioid Treatment Programs
OTP providers must be enrolled with Ohio Medicaid as provider type 95, community substance use
disorder treatment provider, with the 950 provider specialty. Additionally, to bill Medicaid for OTP
specialty services, the provider agency must be licensed as an OTP by OhioMHAS and certified by the
Substance Abuse and Mental Health Services Administration (SAMHSA). Medicaid OTP provider
specialties differ by type:
• Providers of Methadone enroll as Medicaid provider specialty 951.
• Providers of Buprenorphine enroll as Medicaid provider specialty 953.
• Providers of both Methadone and Buprenorphine enroll with both specialties 951 and 953.
These specialties can be added by request through the ODM Provider Network Management (PNM)
system. OTPs will need to upload their documentation of OhioMHAS licensure and SAMHSA
Certification. Once submitted, the request for a new provider specialty and the supporting
documentation will be reviewed by ODM Provider Enrollment and the provider will be notified when
the specialty is added or if additional information is needed.
Buprenorphine Administration for SUD Treatment Programs
For information on billing Buprenorphine, refer to Table 2-9: Provider Administered Pharmaceuticals
OTP Billing Guidance
1. Daily Administration. H0020 with the HF modifier is used for daily methadone
administration, including single take-home doses provided in accordance with Ohio
Administrative Code 5122-40-06. T1502 is used for daily buprenorphine administration,
including single take home doses provided in accordance with Ohio Administrative Code
5122-40-06.
a. If patient is seen every day in order to receive methadone or buprenorphine,
modifier HF must be used with H0020 and T1502 respectively.
b. The date of service for H0020 or T1502 with modifier HF is the date of
administration of the medication or in the case of a daily take-home dose, the
date the patient will take the dose.
2. Weekly Administration. H0020 or T1502 with a modifier representing 1, 2, 3 or 4 weeks
(see Table 6-1) is used for weekly medication administration that includes take-home doses
provided in accordance with 42 Ohio Administrative Code 5122-40-06. The OTP must
maintain documentation in the patient record that supports the number of take-home doses
administered.
a. If any weekly administration modifier has been billed, the OTP cannot bill H0020
or T1502 again during that time period (1, 2, 3, or 4 weeks).
b. Date of service on the claim must be the date the patient was seen in the office
by the OTP in order to receive their take-home medication.

91 | P a g e
3. OTPs administering buprenorphine must bill the appropriate J code (see chart below) for
the medication that was administered. OTPs may bill for take-home doses using S5000
or S5001.
4. 99211 may be used for the nasal administration of naloxone (J2310). This coding
combination is only used when the naloxone is administered nasally on site.
5. 96372 may be used for the injectable administration of naloxone (J2310). This coding
combination is only used when the naloxone is administered by injection on site.
6. J2310 is used for injectable/nasal naloxone administered in accordance with the Ohio
Board of Pharmacy requirements.
7. OTPs may bill for the cost of oral naltrexone (J8499) under their Ohio Board of Pharmacy
license.
8. OTPs may bill for the collection of blood using venipuncture (36415), per draw when the
sample is sent to an outside laboratory for testing.
9. All of the OTP services must be performed by one of the following medical professionals
within their scope of practice: physician, clinical nurse specialist, certified nurse
practitioner, physician assistant, registered nurse, or a licensed practical nurse.
10. Please reference Table 6-1 for additional information on service coding, rates and
modifiers.

92 | P a g e
Table 6-1: Opioid Treatment Programs
Provider Type 95/951 – State Licensed Methadone Program
Service
Description
Provider
Type
Code
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Methadone
Administration
Daily
MD/DO,
CNS, NP,
PA, RN, LPN
H0020
HF
$16.38
$18.47
Weekly (2 – 7 days)
MD/DO,
CNS, NP,
PA, RN, LPN
H0020
TV
$114.66
$129.28
Two Weeks (8 – 14
days)
UB
$229.32
$258.56
Three Weeks (15 – 21
days)
TS
$343.98
$387.84
Four Weeks (22 – 28
days)
HG
$458.64
$517.12
Medications
Oral Naltrexone, per
50 mg tablet
-
J8499
HG
$1.20
$1.35
Injection/Nasal,
naloxone (Narcan),
1mg
-
J2310
-
See Medicaid fee
schedule in effect for date of service.
Laboratory
Services
Collection of venous
blood by venipuncture
Per CPT
guidelines 1
36415
-
See Medicaid fee schedule in effect
for date of service.
Unit Value
CPT or HCPCS designation

93 | P a g e
Table 6-2: Opioid Treatment Programs
Provider Type 95/953 –
SAMHSA Certified Opioid Treatment Program
Service
Description
Provider
Type
Code
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Buprenorphine/
Naloxone
Administration
Daily
MD/DO,
CNS,
CNP, PA,
RN, LPN
T1502
HF
$16.38
$18.47
Weekly (2 – 7
days)
TV
$114.66
$129.28
Two Weeks (8 – 14
days)
UB
$229.32
$258.56
Three Weeks (15 –
21 days)
TS
$343.98
$387.84
Four Weeks (22 –
28 days)
HG
$458.64
$517.12
Medications
Buprenorphine,
oral, 1 mg.
-
J0571
-
See Medicaid fee schedule in effect for date
of service.
Buprenorphine/nal
oxone, oral, less
than or equal to 3
mg.
-
J0572
-
See Medicaid fee schedule in effect for date
of service.
Buprenorphine/nal
oxone, oral, greater
than 3 mg, but less
than or equal to 6
mg.
-
J0573
-
See Medicaid fee schedule in effect for date
of service.
Buprenorphine/nal
oxone, oral, greater
than 6 mg, but less
than or equal to 10
mg.
-
J0574
-
See Medicaid fee schedule in effect for date
of service.
Buprenorphine/nal
oxone, oral, greater
than 10 mg.
-
J0575
-
See Medicaid fee schedule in effect for date
of service.

94 | P a g e
Provider Type 95/953 –
SAMHSA Certified Opioid Treatment Program
Service
Description
Provider
Type
Code
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
Medications
(continued)
Buprenorphine/nal
oxone, generic, per
1mg
buprenorphine/0.25
mgnaloxone
-
S5000
-
$1.20
$1.35
Buprenorphine
generic, per 1 mg.
-
S5000
HD
$0.55
$0.62
Buprenorphine/nal
oxone,
brand, per 1mg
-
S5001
-
$2.30
$2.59
Buprenorphine/0.2
5mg
naloxone
-
-
-
$2.30
$2.59
Oral Naltrexone,
per 50mg tablet
-
J8499
HG
$1.20
$1.35
Injection/Nasal,
naloxone (Narcan),
1mg
-
J2310
-
See Medicaid fee schedule in effect for date
of service.
Laboratory
Services
Collection of
venous blood by
venipuncture
Per CPT
guidelines
1
36415
-
See Medicaid fee schedule in effect for date
of service.
Unit Value
CPT or HCPCS Designation
1
Separate billing for collection of venous blood is only allowable when a provider draws the blood and
sends it to a non-related outside facility without performing any testing.
Coordination of Benefits: Medicare Opioid Treatment Program Benefit
ODM is required by CMS to coordinate Medicaid payment for OTP services to individuals with Medicare
to ensure services and costs that are covered by the Medicare OTP are not being paid by Medicaid or a
Medicaid managed care entity. Based on the Medicare OTP benefit as of the date this manual was
published, Table 6-4 identifies OTP services covered by Medicaid that are included in the Medicare
bundled payment, as well as those that are not part of the Medicare bundled payment. Medicaid claims for
dually eligible recipients will need to show proof of Medicare denial and valid reason for non-payment
prior to Medicaid making any payment for the OTP services that are designated as included in the
Medicare bundled payment. The Medicare OTP benefit is subject to change; therefore, Table 6-4 should
be used as reference. OTP providers are responsible for billing Medicare prior to Medicaid payers for
services that are included in the Medicare OTP bundle.

95 | P a g e
Table 6-3: Medicare Opioid Treatment “Bundle” Billing Codes
Medicaid procedure codes covered under Medicare OTP payment
ASAM Level 1
ASAM Level 2
ASAM Level 3
Ohio Medicaid Codes
Covered by Medicare
H0020/T1502 – med admin
90791-92, H0001 –
assessment
99201-05, 99211-15,
99341-50
H0004 – individual
counseling
H0005 – group counseling
H0048 –non-blood
specimen collection for
alcohol/other drug testing
90832-38 – individual
counseling
90853 – group counseling
96372 – injection admin
H0020/T1502
90791-92, H0001
99201-05, 99211-15,
99341-50
H0004
H0005
H0048
90832-38
90853
96372
H0020/T1502
Ohio Medicaid
Medication codes
Covered by Medicare
S5000-01, J0571-75, J2310, J8499
Ohio Medicaid Lab Drug
Testing Codes Covered
by Medicare
80305-07, 80320-36, 80338-77, 83992, G0480-83
Medicaid procedure codes not covered under Medicare OTP payment
Ohio Medicaid Codes
NOT Covered by
Medicare
H0006 – care management
H0038 - peer recovery
T1002 – RN services
T1003 – LPN services
H0015 – IOP
H0015 TG – PH
H0012 – detox
H0014 – detox
H0006
H0038
T1002
T1003
H2034 – residential
H2036 – residential
H0010 – detox
H0011 – detox

96 | P a g e
SECTION 7
Specialized Recovery Services (SRS) Program [1915(i)]
The SRS program is available to individuals who meet certain financial criteria and have been diagnosed
with a serious and persistent mental illness (SPMI) or a diagnosed chronic condition listed in
Administrative Code rule 5160-43-02 (A) (3). SRS individual eligibility and program enrollment criteria
are detailed in Administrative Code rule 5160-43-02. In addition to full Medicaid coverage, individuals
enrolled in the SRS program have access to these additional services: Recovery Management,
Individualized Placement and Support-Supported Employment (IPS-SE) and Peer Recovery Support
(PRS). To deliver and submit claims for payment for Recovery Management, Peer Recovery Support
and Individualized Placement and Support- Supported Employment providers must meet all the
requirements listed in Administrative Code rule 5160-43-04 in addition to having the following Provider
Type and Specialty:
• Recovery Management
• Provider Type 45
• Provider Specialty 845
• Individualized Placement and Support-Supported Employment (IPS-SE)
• Provider Type 84
• Provider Specialty 851
• Peer Recovery Support
• Provider Type 84
• Provider Specialty 852
For behavioral health agencies to provide and submit for IPS-SE services they must comply with the rules
set forth in 5160-43-04 and 5160-27 of the Administrative Code.
SRS program services are covered when rendered via telehealth. For details on the requirements to render
SRS program services, refer to Administrative Code rule 5160-43-04.

97 | P a g e
Table 7-1: SRS Supported Employment
MH
Service
Provider Type
Code
Rate through
December 31, 2023
Rate effective
January 1, 2024
SRS Supported
Employment,
Initial
Any unlicensed practitioners
per OAC 5160-27-01, except
PRS and “supervised trainees”
under general supervision.
H2023
$19.53
$22.02
SRS Supported
Employment,
Subsequent
Any unlicensed practitioners
per OAC 5160-27-01, except
PRS and “supervised trainees”
under general supervision.
H2025
$19.53
$22.02
Unit Value
15 minutes
Permitted POS
03, 04, 11, 12, 13, 14, 16, 17, 18, 19, 20, 23,
53, 55, 56, 57
*POS 56 not allowable for initial service
Telehealth allowed with GT modifier.
GT modifier is required when service rendered
via telehealth.
Table 7-2: SRS Peer Recovery Support
MH
Service
Provider
Type
Code
Procedure
Modifier
Rate through
December 31, 2023
Rate effective
January 1, 2024
SRS Peer
Recovery Support,
Individual
PRS
H0038
-
$15.51
$17.49
SRS Peer
Recovery Support,
Group
PRS
H0038
HQ
$1.94
$2.19
Unit Value
15 minutes
Permitted POS
Not allowed in 02, 05, 06, 07, 08, 41, 42,
55
Telehealth allowed with GT modifier.
GT modifier is required when service rendered via
telehealth.

98 | P a g e
SECTION 8
OhioRISE
The Ohio Department of Medicaid (ODM) supported by the Governor’s Family and Children First
Cabinet Council, and in partnership with state sister agencies, stakeholders, and providers, developed
Ohio’s first-ever integrated program to help children who have complex and serious behavioral health
needs. OhioRISE (Resilience through Integrated Systems and Excellence), launched on July 1, 2022, aims
to improve care and outcomes for these children and their families or caregivers by:
• Creating a seamless delivery system for children and youth, families/caregivers, and system
partners.
• Providing a “locus of accountability” by offering community-driven comprehensive care
coordination through local Care Management Entities (CMEs).
• Expanding access to critical behavioral health treatment services and supports needed for this
population such as Intensive and Moderate Care Coordination, Mobile Response and
Stabilization, Behavioral Health Respite, Intensive Home-Based Treatment, and Flexible
Funds.
• Assisting youth, families, state, and local child serving agencies, and other health providers to
locate and use these services.
The OhioRISE program covers a range of behavioral health (BH) services for youth that are comprised of
existing, enhanced, and new behavioral health and care coordination services. For more information about
billing for the new and enhanced services for youth enrolled in OhioRISE, please refer to the OhioRISE
Provider Enrollment and Billing Guidance. For youth enrolled in OhioRISE, existing behavioral health
services will be covered in accordance with the OhioRISE Mixed Services Protocol and will be billed
consistent with the billing policies outlined in the appropriate provider type billing guidelines.

99 | P a g e
Appendix: Ohio Medicaid List of Place of Service Codes
Listed below are places of service that are included in the above tables. For a complete list of place of service codes,
please see CMS Place of Service Code Set.
For services delivered via telehealth, providers may use either the place of service code that reflects the location of
the practitioner or the location of the patient. The appendix to OAC 5160-27-03 includes a list of allowable places of
service codes for each procedure code. Please note, place of service code 02 is not allowed. Providers should use the
GT modifier to identify telehealth services.
Code(s)
Place of Service Name
Place of Service Description
01
Pharmacy
A facility or location where drugs and other medically related items and services
are sold, dispensed, or otherwise provided directly to patients.
03
School
A facility whose primary purpose is education.
04
Homeless Shelter
A facility or location whose primary purpose is to provide temporary housing to
homeless individuals (e.g., emergency shelters, individual or family shelters).
11
Office
Location, other than a hospital, skilled nursing facility (SNF), military treatment
facility, community health center, State or local public health clinic, or
intermediate care facility (ICF), where the health professional routinely provides
health examinations, diagnosis, and treatment of illness or injury on an
ambulatory basis.
12
Home
Location, other than a hospital or other facility, where the patient receives care
in a private residence.
13
Assisted Living Facility
Congregate residential facility with self-contained living units providing
assessment of each resident's needs and on-site support 24 hours a day, 7 days a
week, with the capacity to deliver or arrange for services including some health
care and other services.
14
Group Home
A residence, with shared living areas, where clients receive supervision and
other services such as social and/or behavioral services, custodial service, and
minimal services (e.g., medication administration).
16
Temporary Lodging
A short-term accommodation such as a hotel, campground, hostel, cruise ship or
resort where the patient receives care, and which is not identified by any other
POS code.
17
Walk-in Retail Health
Clinic
A walk-in health clinic, other than an office, urgent care facility, pharmacy or
independent clinic and not described by any other Place of Service code, that is
located within a retail operation and provides, on an ambulatory basis,
preventive and primary care services.
18
Place of
Employment/Worksite
A location, not described by any other POS code, owned or operated by a public
or private entity where the patient is employed, and where a health professional
provides on-going or episodic occupational medical, therapeutic or rehabilitative
services to the individual.

100 | P a g e
Code(s)
Place of Service Name
Place of Service Description
20
Urgent Care Facility
Location, distinct from a hospital emergency room, an office, or a clinic, whose
purpose is to diagnose and treat illness or injury for unscheduled, ambulatory
patients seeking immediate medical attention.
22
On Campus-Outpatient
Hospital
A portion of a hospital which provides diagnostic, therapeutic (both surgical and
nonsurgical), and rehabilitation services to sick or injured persons who do not
require hospitalization or institutionalization.
23
Emergency Room -
Hospital
A portion of a hospital where emergency diagnosis and treatment of illness or
injury is provided.
24
Ambulatory Surgical
Center
A freestanding facility, other than a physician's office, where surgical and
diagnostic services are provided on an ambulatory basis.
25
Birthing Center
A facility, other than a hospital's maternity facilities or a physician's office,
which provides a setting for labor, delivery, and immediate postpartum care as
well as immediate care of newborn infants.
31
Skilled Nursing Facility
A facility which primarily provides inpatient skilled nursing care and related
services to patients who require medical, nursing, or rehabilitative services but
does not provide the level of care or treatment available in a hospital.
32
Nursing Facility
A facility which primarily provides to residents skilled nursing care and related
services for the rehabilitation of injured, disabled, or sick persons, or, on a
regular basis, health-related care services above the level of custodial care to
other than individuals with intellectual disabilities.
33
Custodial Care Facility
A facility which provides room, board and other personal assistance services,
generally on a long-term basis, and which does not include a medical
component.
34
Hospice
A facility, other than a patient's home, in which palliative and supportive care
for terminally ill patients and their families are provided.
41
Ambulance - Land
A land vehicle specifically designed, equipped and staffed for lifesaving and
transporting the sick or injured.
42
Ambulance - Air or Water
An air or water vehicle specifically designed, equipped and staffed for lifesaving
and transporting the sick or injured.
53
Community Mental Health
Center
A facility that provides the following services: outpatient services, including
specialized outpatient services for children, the elderly, individuals who are
chronically ill, and residents of the CMHC's mental health services area who
have been discharged from inpatient treatment at a mental health facility; 24
hour a day emergency care services; day treatment, other partial hospitalization
services, or psychosocial rehabilitation services; screening for patients being
considered for admission to State mental health facilities to determine the
appropriateness of such admission; and consultation and education services. If
the facility is not certified by Medicare as a CMHC, POS should be 11,
indicating office.

101 | P a g e
Code(s)
Place of Service Name
Place of Service Description
55
Residential Substance
Abuse Treatment Facility
A facility which provides treatment for substance (alcohol and drug) abuse to
live-in residents who do not require acute medical care. Services include
individual and group therapy and counseling, family counseling, laboratory
tests, drugs and supplies, psychological testing, and room and board.
57
Non-residential Substance
Abuse Treatment Facility
A location which provides treatment for substance (alcohol and drug) abuse on
an ambulatory basis. Services include individual and group therapy and
counseling, family counseling, laboratory tests, drugs and supplies, and
psychological testing.
99
Other Place of Service
Other place of service not identified above. May be used when a more specific
place of service in not available, including community.

