i
MARYLAND DEPARTMENT OF HEALTH
COMAR 10.09.23.01-1
MEDICAL ASSISTANCE PROGRAM
Audiology, Physical
Therapy, and Early Periodic,
Screening, Diagnosis, and
Treatment (EPSDT)
Provider Manual
EFFECTIVE JANUARY 2019
ii
TABLE OF CONTENTS
EPSDT PROVIDER MANUAL OVERVIEW .............................................................................. 1
GENERAL INFORMATION……………………………………………………………………..5
Patient Eligibility & Eligibility Verification System (EVS) ....................................................... 5
Billing Medicare ......................................................................................................................... 2
MCO Billing ............................................................................................................................... 3
Fee for Service Billing………………………………………………………………………….6
Medical Assistance Payments ..................................................................................................... 4
The Health Insurance Portability & Accountability Act (HIPAA) ............................................... 5
National Provider Identifier (NPI) .............................................................................................. 5
Fraud and Abuse ......................................................................................................................... 5
Appeal Procedure ........................................................................................................................ 6
Regulations .................................................................................................................................. 6
Provider Requirements................................................................................................................ 6
EPSDT ACUPUNCTURE, CHIROPRACTIC, SPEECH LANGUAGE PATHOLOGY,
OCCUPATIONAL & NUTRITION THERAPY SERVICES & PHYSICAL THERAPY
SERVICES……………………………………………………………………………………….10
EPSDT Overview ....................................................................................................................... 7
Covered Services ....................................................................................................................... 8
EPSDT Acupuncture, Chiropractic, Speech Language Pathology, and Occupational Therapy
Services ................................................................................................................................... 8
Physical Therapy ..................................................................................................................... 9
EPSDT Nutrition Services .................................................................................................... 10
Preauthorization ...................................................................................................................... 10
Provider Enrollment ................................................................................................................ 10
EPSDT Population………………………………………………………………….………..15
Procedure Codes and Fee Schedules............................................................................................. 13
EPSDT Acupuncture Services .............................................................................................. 13
EPSDT Chiropractic Services ............................................................................................... 13
Physical Therapy ................................................................................................................... 14
iii
EPSDT Occupational Therapy .............................................................................................. 15
EPSDT Speech Language Pathology .................................................................................... 16
EPSDT Nutrition Services .................................................................................................... 17
AUDIOLOGY SERVICES ........................................................................................................... 18
Overview ................................................................................................................................... 18
Covered Services ...................................................................................................................... 18
Limitations ................................................................................................................................ 19
Preauthorization Requirements ................................................................................................. 21
Payment Procedures .................................................................................................................. 23
Audiology Services Fee Schedule ............................................................................................ 25
Audiology Services ............................................................................................................... 27
Hearing Aid, Cochlear Implant, Auditory Osseointegrated Devices and Accessories &
Supplies ................................................................................................................................. 29
VISION CARE SERVICES ......................................................................................................... 31
Overview ................................................................................................................................... 31
Covered Services ...................................................................................................................... 31
Service Limitations ................................................................................................................... 32
Preauthorization Requirements ................................................................................................. 35
Provider Enrollment .................................................................................................................. 38
Payment Procedures .................................................................................................................. 38
Preauthorization Required Prior To Treatment......................................................................... 41
Professional Services Fee Schedule - Provider Type 12 (Non-facility & Facility Included)…. .. 42
Professional Services Fee Schedule - Provider Type 12 – (Facility Only)................................... 45
ATTACHMENT A: MARYLAND MEDICAL ASSISTANCE PROGRAM FREQUENTLY
REQUESTED TELEPHONE NUMBERS ................................................................................... 48
ATTACMENT B: HEALTH INSURANCE CLAIM FORM ...................................................... 50
ATTACHMENT C: MARYLAND DEPARTMENT OF HEALTH PREAUTHORIZATION
REQUEST FORM - VISION CARE SERVICES ........................................................................ 52

1
PROVIDER MANUAL OVERVIEW
In this manual, you will find billing and reimbursement information for the following Medicaid
services: Acupuncture, Chiropractic, Speech Language Pathology, Occupational Therapy,
Nutrition Therapy, Physical Therapy, Audiology, and Vision Services. The information
provided is related to services provided to Medicaid participants who are 20 years of age or
younger, except for audiology and physical therapy services which are covered for Medicaid
participants of all ages. Please refer to the table of contents to find information specific to each
of the covered services.
Occupational therapy, speech language pathology, and physical therapy services are “carved-
out” from the HealthChoice Managed Care Organization (MCO) benefits package for
participants who are 20 years of age and younger and must be billed Fee-for-Service (FFS)
directly to the Medicaid Program.
Acupuncture, chiropractic, nutrition, and vision services are covered by the HealthChoice
Managed Care Organization (MCO) benefits package for participants who are 20 years of age
and younger.
Effective July 1, 2018, audiology services are covered by the HealthChoice MCO benefits
package for participants of all ages.
EPSDT refers to Early Periodic Screening, Diagnosis, and Treatment services for participants
under the age of 21.
Some services described in this manual are both EPSDT services (covered under age 21) and
are also covered services for adults. Some services for adults described in this manual are only
covered in certain settings. Most Medical Assistance participants are enrolled in MCOs.
Certain services for children are not part of the MCO benefit package; instead, they are carved
out and must be billed to Medicaid FFS as described in this manual.
EPSDT services covered by the MCO are described in COMAR 10.09.67.20. When a
participant under age 21 is enrolled in an MCO, contact the MCO unless the service is carved
out.
When a participant age 21 and older is enrolled in an MCO, the services described in this
manual that are covered for adults are the responsibility of the MCO. These services are
described in COMAR 10.09.67. Providers must contact the MCO for further details.
When a participant is not enrolled in an MCO, providers must follow the guidance in this
manual.

2
General Information
Patient Eligibility & Eligibility Verification System (EVS)
The EVS is a telephone inquiry system that enables health care providers to verify quickly and
efficiently a Medical Assistance participant‟s current eligibility status. Medical Assistance
eligibility should be verified on EACH DATE OF SERVICE prior to rendering services.
Although Medical Assistance eligibility validation via the Program‟s EVS system is not
required, it is to your advantage to do so to prevent the rejection of claims for services rendered
to a canceled/non-eligible participant. Before rendering a Medical Assistance service, verify
the participant’s eligibility on the date of service via the Program’s Eligibility Verification
System (EVS) 1-866-710-1447.
If you need additional EVS information, please call the Provider Relations Unit at 410-767-
5503 or 800-445-1159. EVS is an invaluable tool that is fast and easy to use.
For providers enrolled in eMedicaid, Web EVS, a new web-based eligibility application, is now
available at www.emdhealthchoice.org. The provider must be enrolled in eMedicaid in order to
access the web EVS system. For additional information view the website or contact 410-767-
5340 for provider support.
Billing Medicare
The Program will authorize payment on Medicare claims if:
• The provider accepts Medicare assignments;
• Medicare makes direct payment to the provider;
• Medicare has determined that services were medically justified;
• The services are covered by the Program; and
• Initial billing is made directly to Medicare according to Medicare guidelines.
If the participant has insurance or other coverage such as Medicare, or if any other person is
obligated, either legally or contractually, to pay for, or to reimburse the participant for the
services in these guidelines, the provider should seek payment from that source first. If an
insurance carrier rejects the claim or pays less than the amount allowed by the Medical
Assistance Program, the provider should submit a claim to the Program. A copy of the
insurance carrier‟s notice or remittance advice should be kept on file and available upon request
by the Program. In this instance, the CMS-1500 must reflect the letter K (services not covered)
in box 11 of the claim form.
Specifically, when a provider bills Medicare Part B for services rendered to a Medicaid
participant and the provider accepts assignment on the claim, the payments should be made

3
automatically. However, if payment is not received within 30 days, the claim may not have
successfully crossed over and the claim should be submitted to the Program on a CMS-1500
along with the Medicare Explanation of Benefits (EOB). Note: When dropping claims to paper,
the CMS-1500 and EOB should match Medicare claim line for line.
Providers should only submit claims to Medicare for services rendered to patients who are
dually eligible for both Medicare and Medicaid. The Program must receive Medicare/Medicaid
crossover claims within 120 days of the Medicare payment date. This is the date on Medicare's
EOB form. The Program recognizes the billing time limitations of Medicare and will not make
payment when Medicare has rejected a claim due to late billing. In general, the Program does
not pay Medicare Part B coinsurance or copayments on claims where Medicare payment
exceeds the Medicaid fee schedule.
Contact Medical Assistance‟s Provider Relations Office if you have questions about
completing claim forms or Medicare crossover claims.
MCO Billing
Other than the carve-out services of PT, OT, and speech therapy for children under the age of
21, claims for participants who are enrolled in an MCO must be submitted to the MCO for
payment. Contact the MCO for information regarding their billing and preauthorization
procedures.
Acupuncture, nutrition, and chiropractic services are a covered benefit through the MCO system
for participants who are 20 years old and younger. Audiology services are a covered benefit
through the MCO system for participants of all ages. Contact the MCO for information
regarding their billing and preauthorization procedures.
Fee-for-Service (FFS) Billing
Providers shall bill the Maryland Medical Assistance Program for reimbursement on the CMS-
1500 and attach any requested documentation. Maryland Medical Assistance specific procedure
codes are required for billing purposes. Please refer to the procedure code and fee schedule that
is included in this manual.
The Program reserves the right to return to the provider, before payment, all invoices not
properly signed, completed, and accompanied by properly completed forms required by the
Department.
The provider shall charge the Program their usual and customary charge to the general public
for similar services. The Program will pay for covered services, based upon the lower of the
following:
• The provider‟s customary charge to the general public; or
• The Department‟s fee schedule.

4
The Provider may not bill the Program or participants for:
• Services rendered by mail or telephone;
• Completion of forms and reports;
• Broken or missed appointments; or
• Services which are provided at no charge to the general public.
To ensure payment by the Maryland Medical Assistance Program, check Maryland Medical
Assistance‟s Eligibility Verification System (EVS) for every Medical Assistance patient on the
date of service.
Under Medical Assistance‟s Fee-for-Service system, services are reimbursed on a per visit basis
under the procedure code that is listed on Maryland Medical Assistance‟s established
procedure code and fee schedule. The schedule will indicate the maximum units allowed for the
service and the reimbursement amount for each unit of service. The maximum units are the
total number of units that can be billed on the same day of service. Maryland Medical
Assistance will reject claims that exceed the maximum units of service.
PLEASE NOTE: All submitted claims must include the MA number and NPI for the rendering
provider.
Medical Assistance Payments
You must accept payment from Medical Assistance as payment in full for a covered service.
You cannot bill a Medical Assistance participant under the following circumstances:
• For a covered service for which you have billed Medical Assistance;
• When you bill Medical Assistance for a covered service and Medical Assistance denies
your claims because of billing errors you made, such as: wrong procedure codes, lack of
preauthorization, invalid consent forms, unattached necessary documentation,
incorrectly completed forms, filing after the time limitations, or other provider errors;
• When Medical Assistance denies your claim because Medicare or another third party has
paid up to or exceeded what Medical Assistance would have paid;
• For the difference in your charges and the amount Medical Assistance has paid;
• For transferring the participant‟s medical records to another health care provider; and/or
• When services were determined to not be medically necessary.
You can bill the participant under the following circumstances:
• If the service provided is not covered by Medical Assistance and you have notified the
participant prior to providing the service that the service is not covered; or
• If the participant is not eligible for Medical Assistance on the date you provided the
service.

5
The Health Insurance Portability & Accountability Act (HIPAA)
HIPAA of 1996 requires that standard electronic health transactions be used by health plans,
including private, commercial, Medical Assistance and Medicare, health care clearinghouses,
and health care providers.
More information on HIPAA may be obtained from:
http://dhmh.maryland.gov/hipaa/Pages/Home.aspx.
National Provider Identifier (NPI)
Effective July 30, 2007, all health care providers that perform medical services must have an
NPI. The NPI is a unique, 10-digit, numeric identifier that does not expire or change. NPI‟s are
assigned to improve the efficiency and effectiveness of the electronic transmission of health
information. Implementation of the NPI impacts all practice, office, or institutional functions,
including billing, reporting, and payment.
The NPI is administered by the Centers of Medicare and Medicaid Services (CMS) and is
required by HIPAA. Providers must use the legacy MA number as well as the NPI number when
billing on paper.
Apply for an NPI by using the web-based application process via the National Plan and Provider
Enumeration System (NPPES) at https://nppes.cms.hhs.gov/NPPES/Welcome.do.
Fraud and Abuse
It is illegal to submit reimbursement requests for:
• Amounts greater than your usual and customary charge for the service. If you have more
than one charge for a service, the amount billed to the Maryland Medical Assistance
Program should be the lowest amount billed to any person, insurer, health alliance or
other payer;
• Services which are either not provided or not provided in the manner described on the
request for reimbursement. In other words, you must accurately describe the service
performed, correctly define the time and place where the service was provided and
identify the professional status of the person providing the service;
• Any procedures other than the ones you actually provide;
• Multiple, individually described or coded procedures if there is a comprehensive
procedure which could be used to describe the group of services provided;
• Unnecessary, inappropriate, non-covered or harmful services, whether or not you
actually provided the service; or
• Services for which you have received full payment by another insurer or party.
You are required to refund all overpayments received from the Medical Assistance Program

6
within 30 days. Providers must not rely on Department requests for any repayment of such
overpayments. Retention of any overpayments is also illegal.
A provider who is suspended or removed from the Medical Assistance Program or who
voluntarily withdraws from the Program must inform participants before rendering services that
he/she is no longer a Medical Assistance provider and the participant is therefore financially
responsible for the services.
Appeal Procedure
Appeals related to Medical Assistance are conducted under the authorization of COMAR
10.09.36.09 and in accordance with COMAR 10.01.03. To initiate an appeal, the appeal must
be filed within 30 days of the date of a notice of administrative decisions in accordance with
COMAR 10.01.03.06.
Regulations
Visit the following website to review the regulations that pertain to this manual:
http://www.dsd.state.md.us/COMAR/ComarHome.html.
Select option #3; choose select by title number; select title number 10 – Maryland Department
of Health; Select Subtitle 09 - Medical Care Programs; to view individual regulations select:
1) COMAR 10.09.23 for EPSDT;
2) COMAR 10.09.23 for acupuncture, nutrition, chiropractic, occupational therapy, or
speech language pathology services;
3) COMAR 10.09.17 for physical therapy services;
4) COMAR 10.09.51 for audiology services;
5) COMAR 10.09.14 for vision services; and
6) COMAR 10.09.36 for general Medical Assistance provider participation criteria.
Provider Requirements
The provider must meet requirements as set forth in COMAR 10.09.36, General Medical
Assistance Provider Participation Criteria, including:
1. Be licensed and legally authorized to practice in the state in which the service is
provided;
2. Verify a Medical Assistance participant‟s eligibility prior to rendering services;
3. Maintain adequate records for a minimum of 6 years and make them available, upon
request, to the Department or its designee;

7
4. Provide service without regard to race, creed, color, age, sex, national origin, marital
status, or physical or mental handicap;
5. Not knowingly employ a provider to render services to Medical Assistance patients
after that provider has been disqualified from the Program, unless prior approval has
been received from the Department;
6. Accept payment by the Department as payment in full for services rendered and make
no additional charge to any person for covered services;
7. Place no restrictions on participants‟ right to select providers of their choice; and
8. Agree that if the Program denies payment or requests repayment on the basis that an
otherwise covered service was not medically necessary, the provider may not seek
payment for that service from the participant or family members.
EPSDT ACUPUNCTURE, CHIROPRACTIC, SPEECH
LANGUAGE PATHOLOGY, OCCUPATIONAL & NUTRITION
THERAPY SERVICES & PHYSICAL THERAPY SERVICES
EPSDT Overview
This section of the manual addresses occupational therapy, speech language pathology and
physical therapy services for children when the services are not part of home health services or
an inpatient hospital stay. These services are “carved-out” from the HealthChoice Managed
Care Organization (MCO) benefits package for participants who are 20 years of age and
younger and must be billed Fee-for-Service directly to the Medicaid Program. Services
provided by pediatricians, internists, family practitioners, general practitioners, nurse
practitioners, neurologists, and/or other physicians to determine whether a child has a need
for occupational therapy, physical therapy or speech language pathology services are the
responsibility of the MCO and must be billed to the MCO. When therapy services are
provided to participants under age 21 as part of home health or an inpatient hospital stay they
become the responsibility of the MCO. In addition, MCOs reimburse for community-based
rehabilitation, including physical and occupational therapy and speech language pathology
services for adult enrollees. Contact the MCO for their preauthorization and billing
policy/procedures for participants 21 years of age and older.
Acupuncture, chiropractic, and nutrition services addressed in this manual are limited to
Maryland Medical Assistance‟s Early Periodic Screening, Diagnosis and Treatment (EPSDT)
population (services for participants who are 20 years of age and younger). These services are
not generally covered for adults. When a participant under age 21 is enrolled in HealthChoice
the MCO is responsible for covering these services.

8
The following chart outlines the payer for these services when the participant is enrolled in an
MCO:
Service
Bill the MCO
Bill Fee-for-Service (FFS)
Medical Assistance
Occupational Therapy
21 + older
0-20
Physical Therapy
21 + older
0-20
Speech Language
21 + older
0-20
Acupuncture
0-20
------
Chiropractic
0-20
------
Nutrition
0-20
------
Home Health Therapy
0-99
------
Inpatient Therapy
0-99
------
Therapy services provided by a hospital, home health agency, inpatient facility, nursing home,
RTC, local lead agency, school or in accordance with an IEP/IFSP, model waiver, etc., are not
specifically addressed in this manual.
Covered Services
EPSDT Acupuncture, Occupational Therapy, Speech Language Pathology &
Chiropractic Services
For occupational therapy and speech language pathology services bill Fee-for-Service for
participants under 21 years of age. Contact the MCO for preauthorization for participants 21
years of age and older. Acupuncture and chiropractic services for participants under age 21 are
covered through the MCO.
Services are covered for participants who are 20 years of age and younger when the services
are:
• Necessary to correct or ameliorate defects and physical illnesses and/or
conditions discovered in the course of an EPSDT screen;
• Provided upon the referral order of a screening provider;
• Rendered in accordance with accepted professional standards and when the condition of
a participant requires the judgment, knowledge, and skills of a licensed acupuncturist,
licensed occupational therapist, licensed speech pathologist or licensed chiropractor;
• Delivered in accordance with the plan of treatment;
• Limited to one initial evaluation per condition; and
• Delivered by a licensed acupuncturist, licensed chiropractor, licensed occupational
therapist, or a licensed speech pathologist.
In order to participate as an EPSDT-referred services provider, the provider shall:

9
• Gain approval by the screening provider every six (6) months or as authorized by the
Department for continued treatment of a participant. Approval must be documented by
the screening provider and the therapist, acupuncturist, or chiropractor in the
participant‟s medical record;
• Have experience with rendering services to individuals from birth through 20 years of
age;
• Submit a quarterly progress report to the participant‟s primary care provider; and
• Maintain medical documentation for each visit.
PLEASE NOTE: Services provided in a facility or by a group where reimbursement is covered
by another segment of the Medical Assistance Program are not covered.
Physical Therapy
PLEASE NOTE: Bill Fee-for-Service Medical Assistance for participants under 21 years of
age. Contact the MCO for preauthorization for participants 21 years of age and older.
Medically necessary physical therapy services ordered in writing by a physician, nurse
practitioner, physician assistant, nurse midwife, doctor of dental surgery or of dental medicine
or podiatrist are covered when:
• Provided by a licensed physical therapist or by a licensed physical therapist assistant
under direct supervision of the licensed physical therapist;
• Rendered in the provider‟s office, the participant‟s home, or a domiciliary level
facility;
• Diagnostic, rehabilitative, or therapeutic and directly related to the written treatment
order;
• Of sufficient complexity and sophistication, or the condition of the patient is such,
that the services of a physical therapist are required;
• Rendered pursuant to a written treatment order that is signed and dated by the
prescriber;
• The treatment order is kept on file by the physical therapist as part of the participant‟s
permanent record;
• Not altered in type, amount, frequency, or duration by the therapist unless medically
indicated. The physical therapist shall make necessary changes and sign the treatment
order, advising the prescriber of the change and noting it in the patient‟s record;
• Limited to one initial evaluation per condition; and
• A new order is requested from the prescriber, for continued therapy, if the order exceeds 30
days.
Services are to be recorded in the patient‟s permanent record which shall include:
• The treatment order of the prescriber;

10
• The initial evaluation by the therapist and significant past history;
• All pertinent diagnoses and prognoses;
• Contraindications, if any; and
• Progress notes documented in accordance with the requirements listed in COMAR
10.38.03.02-1A(2), C, and D.
The following physical therapy services are not covered:
• Services provided in a facility or by a group where reimbursement for physical
therapy is covered by another segment of the Medical Assistance Program;
• Services performed by licensed physical therapy assistants when not under the direct
supervision of a licensed physical therapist;
• Services performed by physical therapy aides;
• Experimental treatment; and/or
• More than one initial evaluation per condition.
EPSDT Nutrition Services
Medically necessary nutrition services provided by a licensed dietician nutritionist;
Rendered in accordance with accepted professional standards and when the condition of
a participant requires the judgment, knowledge, and skills of a licensed dietician
nutritionist.
PLEASE NOTE: Nutrition services are covered through the MCO; contact the MCO for
preauthorization information if serving an MCO enrollee.
Preauthorization
Contact the MCO for information regarding their billing and preauthorization procedures for
acupuncture, chiropractic, nutrition, and therapy services for participants who are under 21, or
who are receiving home health and inpatient services.
Preauthorization is not required under the Fee-for-Service system; however, it is expected that a
quarterly care plan be shared with the participant's primary care provider.
Provider Enrollment
PLEASE NOTE: Under the Maryland Medical Assistance program, acupuncturists, therapists
and chiropractors who are part of a physician‟s group are not considered physician extenders.
Services rendered by these providers cannot be billed under the supervising physician‟s
rendering number. These providers must complete an enrollment application and obtain a

11
Maryland Medical Assistance provider number that has been specifically assigned to them under
their name. The number will be used when billing directly to Maryland Medical Assistance.
Therapists, acupuncturists, nutrition dieticians, and chiropractors must be licensed to practice
their specialties in the jurisdictions where they practice. (Chiropractors must be licensed and
enrolled as a physical therapist in order to bill for physical therapy services.)
When a Maryland Medical Assistance Program provider application has been approved for
participation in the Program a nine digit provider identification number will be issued. This
number will permit the provider to bill the Program‟s computerized payment processing system
for services that are covered under the Fee-for-Service system. Applicants enrolling as a
renderer in a group practice must be associated with a Maryland Medical Assistance existing or
new group practice of the same provider type (i.e. a PT can enroll as a renderer in a PT group
practice but not in a physician group practice).
PLEASE NOTE: All submitted claims must include the MA number and NPI for the rendering
provider.
Changes to the practice must be brought to the attention of the Program.
Provider Type
Type of Practice
Specialty Codes
AC - Acupuncture
35 (group) or 30 (individual
or renderer in a group
practice)
18 - Occupational Therapist
35 (group) or 30 (individual or
renderer in a group practice)
EPSDT –
Occupational
Therapy (173)
17 - Speech Language Pathologist
35 (group) or 30 (individual or
renderer in a group practice)
EPSDT – Speech
/Language Pathology
(209)
13 - Chiropractor
35 (group) or 30 (individual
or renderer in a group
practice)
EPSDT – Chiropractor (106)
16 - Physical Therapist
35 (group) or 30 (individual
or renderer in a group
practice)
Physical Therapy (189)
28 - Therapy Group
35 (group) or 30 (individual or
renderer in a group practice)
Must be comprised of at
least two different
specialties: OT (173), PT
(189), SP (209)

12
Provider Type
Type of Practice
Specialty Codes
85 - Nutritionist
35 (group) or 30 (individual or
renderer in a group practice)
EPSDT Nutrition Counseling
(124)
Healthy Start Nutrition (141)
EPSDT Population
Under 21 years of age – EPSDT Population
Speech language pathology, occupational therapy and physical therapy services provided to
participants who are 20 years of age or younger are part of Maryland Medical Assistance‟s Fee-
for-Service system when not provided as a home health or inpatient service. Home health and
inpatient care are coverable by the MCO. Therapy providers who are enrolled as a Maryland
Medical Assistance provider may render the prescribed therapy services and bill the Program
directly on the CMS-1500 form under his/her Maryland Medical Assistance assigned provider
identification number.
Acupuncture, nutrition, and chiropractic services continue as a covered benefit under the MCO
system; these services must be billed to the MCO for MCO enrollees. Contact the MCO for
preauthorization/treatment procedures for acupuncture, nutrition, and chiropractic services.
21 years of age and older
The majority of Maryland Medical Assistance participants are enrolled in an MCO. It is
customary for the MCO to refer their enrollees to therapists in their own provider network for
this age group. If a participant is 21 or older and is enrolled in an MCO, preauthorization may
be required by the MCO before treating the patient. Contact the participant‟s MCO for their
authorization/treatment procedures.
Under Medical Assistance‟s Fee-for-Service system, coverage for community-based therapy
services for the 21 and over age population is limited to physical therapy services unless
coverable under a different Maryland Medical Assistance Program that is not specifically
addressed in this manual (i.e. hospital services, home health services, etc.)

13
Procedure Codes and Fee Schedules Effective July 1, 2018
EPSDT Acupuncture Services
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
97810
Acupuncture, 1 or more
needles; without electrical
stimulation, initial 15-minutes
of personal one-on-one
contact with the patient
N
1
$28.37
97811
Acupuncture without
electrical stimulation, each
additional 15-minutes of
personal one-on-one contact
with the patient, with re-
insertion of needle(s)
N
1
$21.11
97813
Acupuncture with electrical
stimulation, initial 15-
minutes of personal one-on-
one contact with the patient
N
1
$30.27
97814
Acupuncture with electrical
stimulation, initial 15-
minutes of personal one-on-
one contact with the patient,
with re-insertion of needle(s)
N
1
$23.86
EPSDT Chiropractic Services
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
98940
Chiropractic Manipulative
Treatment Spinal, 1 to 2
regions
N
1
$22.00
98941
Chiropractic Manipulative
Treatment Spinal, 3 to 4
regions
N
1
$31.51
98942
Chiropractic Manipulative
Treatment Spinal, 5
regions
N
1
$41.04
98943
Chiropractic Manipulative
Treatment Extra spinal, 1
or more regions
N
1
$21.18

14
Physical Therapy
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
97161
Physical Therapy Evaluation,
Low complexity, 20 minutes
N
1
$69.20
97162
Physical Therapy Evaluation,
Moderate complexity, 30 minutes
N
1
$69.20
97163
Physical Therapy Evaluation,
High complexity, 45 minutes
N
1
$69.20
97164
Physical Therapy Re-Evaluation,
Established plan of care
N
1
$47.19
97010
Application of modality to
1 or more Areas; hot or
cold packs (supervised)
N
10
$4.77
97012
Mechanical Traction (supervised)
N
10
$12.67
97014
Electrical Stimulation
(unattended)
N
1
$12.52
97016
Vasopneumatic Devices
N
2
$15.37
97018
Paraffin Bath
N
10
$8.76
97022
Whirlpool
N
10
$18.81
97024
Diathermy (e.g. microwave)
N
10
$5.34
97026
Infrared
N
10
$4.77
97028
Ultraviolet Light
N
10
$5.87
97032
Attended Electrical
Stimulation, each 15 minutes
N
4
$14.96
97033
Iontophoresis, each 15 minutes
N
4
$17.48
97034
Contrast Bath, each 15-minutes
N
4
$14.17
97035
Ultrasound, each 15-minutes
N
4
$9.90
97036
Hubbard Tanks, each 15-minutes
N
4
$26.01
97110
Therapeutic Procedure, each 15-
minutes
N
4
$29.03
97112
Neuromuscular Reeducation
N
4
$26.58
97113
Aquatic Therapy
N
4
$33.98
97116
Gait Training
N
4
$22.08
97124
Therapeutic Massage
N
4
$20.46

15
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
97140
Manual Therapy
Techniques, each 15
minutes
N
4
$23.45
97597
Selective Debridement (for
wounds ≤ 20 sq. cm.)
N
1
$59.82
97598
Selective Debridement
(for each additional 20
sq. cm wound)
N
1
$25.68
97605
Negative pressure wound therapy
N
1
$32.38
97606
Total wound surface area ≥ 50
sq.cm.
N
1
$38.27
97607
Negative pressure wound therapy
≤ 50 sp. cm
N
1
$37.79
97608
Negative pressure wound therapy
> 50 sq. cm.
N
1
$44.97
97750
Physical performance
test or measurement,
each 15 minutes
N
3
$25.72
97755
Assistive Technology
Assessment each 15 minutes
N
2
$27.68
EPSDT Occupational Therapy
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number
of Units
Maximum
Payment
97165
Occupational Therapy
Evaluation, Low complexity,
30 minutes
N
1
$ 67.01
97166
Occupational Therapy
Evaluation, Moderate
complexity, 45 minutes
N
1
$67.01
97167
Occupational Therapy
Evaluation, High Complexity,
60 minutes
N
1
$67.01
97168
Occupational Therapy
Re-Evaluation, Established
plan of care
N
1
$ 44.34

16
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number
of Units
Maximum
Payment
97530
Therapeutic Activities, each 15
minutes
N
4
$ 30.56
EPSDT Speech Language Pathology
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
92507
Individual
N
1
$ 63.99
92508
Group
N
1
$ 30.47
92521
Evaluation of speech fluency
N
1
$ 91.35
92522
Evaluation of speech sound
production
N
1
$74.00
92523
Evaluation of speech sound
production with evaluation
of language comprehension
and expression
N
1
$153.97
92524
Behavioral and qualitative
analysis of voice and
resonance
N
1
$77.40
92526
Treatment of swallowing
dysfunction and/or oral
function for feeding
N
1
$80.85
92607
Evaluation for prescription for
speech-generating
augmentative and alternative
communication device, face-
to-face with patient, first hour
N
1
$121.74
92608
Evaluation for prescription for
speech-generating
augmentative and alternative
communication device, face-
to-face with patient, each
additional 30 minutes
N
4
$41.53
92609
Therapeutic services for the
use of speech-generating
device, including
programming and
modification
N
1
$86.26

17
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
92610
Evaluation of oral and
pharyngeal swallowing
function
N
1
$81.43
92626
Evaluation of auditory
rehabilitation status
N
1
$70.21
92627
Evaluation of auditory
rehabilitation
N
3
$17.37
92630
Auditory rehabilitation; pre-
lingual hearing loss
N
1
$63.99
92633
Auditory rehabilitation; post-
lingual hearing loss
N
1
$63.99
EPSDT Nutrition Services
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Number of
Units
Maximum
Payment
97802
Nutrition Assessment
and intervention
N
4
$30.03
97803
Nutrition Re-
assessment and
intervention
N
4
$26.35
97804
Group Nutrition
Service
N
1
$13.55
PLEASE NOTE: Services are reimbursed up to the maximum units as indicated on this
schedule. Providers enrolled as a Therapy Group (Provider Type 28) may bill the per visit
charge for each enrolled discipline participating in the group. Please refer to the fee schedule for
maximum reimbursement.
Claims must reflect the above referenced procedure codes for proper reimbursement. These codes
are specific to services outlined in the Provider Manual for EPSDT acupuncture, nutrition,
chiropractic, speech language pathology, and occupational therapies, as well as physical therapy
services, and they are specific to the Maryland Medical Assistance Fee-for-Service system of
payment.

18
AUDIOLOGY SERVICES
Overview
As of July 1, 2018, audiology services for the EPSDT population will be provided through the
enrollee‟s managed care organization (MCO). These services were placed back into the MCO
system of payment. Effective July 1, 2018, audiology services are a covered Medicaid benefit
for all Medicaid participants when determined to be medically necessary. The participant may
have to receive a preauthorization or referral from the MCO before visiting an audiologist for
evaluation and/or treatment. Maryland Medical Assistance FFS requires preauthorization on
certain services. In order to determine which service requires preauthorization, review the
attached fee schedule for audiology services.
Covered Services
All services for which reimbursement is sought must be provided in accordance with the
regulations for Maryland Medical Assistance Audiology Services (COMAR 10.09.51).
The Program covers the following medically necessary audiology services:
1. Audiology services, as follows:
a. Audiology assessments using procedures appropriate for the participant‟s
developmental age and abilities; and
b. Hearing-aid evaluations and routine follow-up for participants with an identified
hearing impairment, who currently use or are being considered for hearing aids;
2. Hearing amplification services, as follows:
a. Unilateral or bilateral hearing aids which are:
1. Not used or rebuilt, and which meet the current standards set forth in 21
CFR §§801.420 and 801.421, which are incorporated by reference;
2. Recommended and fitted by an audiologist when in conjunction with
written medical clearance from a physician who has performed a medical
examination within the past 6 months;
3. Sold on a 30-day trial basis; and
4. Fully covered by a manufacturer‟s warranty for a minimum of 2 years at
no cost to the Program;

19
b. Hearing aid accessories and services, as listed below:
1. Ear molds;
2. Batteries;
3. Routine follow-ups and adjustments;
4. Repairs after all warranties have expired;
5. Replacement of unilateral or bilateral hearing aids every 5 years when
determined to be medically necessary; and
6. Other hearing aid accessories determined to be medically necessary;
c. Cochlear implants and related services, as listed below:
1. Unilateral or bilateral implantation of cochlear implant or implants which
are medically necessary including the cost of the device;
2. Post-operative evaluation and programming of the cochlear implant or
implants;
3. Aural rehabilitation services; and
4. Repair or replacement of cochlear implant device components subject to
the limitations in COMAR 10.09.51.05;
d. Auditory osseointegrated device or devices and related services, as listed below:
1. Unilateral or bilateral implantation of auditory osseointegrated devices
which are medically necessary including the cost of the device;
2. Non-implantable or softband device or devices;
3. Evaluation and programming of the auditory osseointegrated device or
devices; and
4. Repair or replacement, or both of auditory osseointegrated device
components subject to the limitations in COMAR 10.09.51.05.
Limitations
A. Covered audiology services including hearing aids, cochlear implants and auditory
osseointegrated devices are limited to:
1. Unless the time limitation is waived by the Department, one audiology assessment per
year;
20
2. The initial coverage of unilateral or bilateral hearing aids, cochlear implants, or
auditory osseointegrated devices when the Department‟s medical necessity criteria have
been met;
3. Replacement of unilateral or bilateral hearing aids once every 5 years unless the
Program approves more frequent replacement;
4. Replacement of hearing aids, cochlear implants and auditory osseointegrated device
components that have been lost, stolen, or damaged beyond repair, after all warranties
policies have expired;
5. Repairs and replacements that take place after all warranties have expired;
6. A maximum of 76 batteries per participant per 12-month period for a unilateral hearing
aid or osseointegrated devices, or 152 batteries per participant per 12-month period for
a bilateral hearing aid or osseointegrated devices purchased from the Department not
more frequently than every 6 months, and in quantities of 38 or fewer for a unilateral
hearing aid or osseointegrated, or 76 or fewer for a bilateral hearing aid or
osseointegrated device;
7. A maximum of 238 disposable batteries for a unilateral cochlear implant per
participant per 12-month period or 476 disposable batteries per 12-month period for a
bilateral cochlear implant purchased not more frequently than every 6 months, and in
quantities of 119 or fewer for a unilateral cochlear implant, or 238 or fewer for a
bilateral cochlear implant;
8. Four replacement cochlear implant component rechargeable batteries per 12-month
period for bilateral cochlear implants, and a maximum of two replacement
rechargeable batteries per 12-month period for a unilateral cochlear implant;
9. Two cochlear implant replacement transmitter cables per 12-month period for bilateral
cochlear implants, and a maximum of one replacement transmitter cable per 12-month
period for a unilateral cochlear implant;
10. Two cochlear implant replacement headset cables per 12-month period for bilateral
cochlear implants, and a maximum of one replacement headset cable per 12- month
period for a unilateral cochlear implant;
11. Two cochlear implant replacement transmitting coils per 12-month period for bilateral
cochlear implants, and a maximum of one replacement transmitting coil per 12-month
period for a unilateral cochlear implant;
12. Charges for routine follow-ups and adjustments which occur more than 60 days after
the dispensing of a new hearing aid; and
13. A maximum of two unilateral earmolds or four bilateral earmolds per 12-month period
unless a larger amount are determined to be medically necessary.

21
B. Services which are not covered are:
1. Services not medically necessary;
2. Hearing aids and accessories not medically necessary;
3. Cochlear implant services and external components not medically necessary;
4. Cochlear implant services and external components provided less than 90 days after the
surgery which are covered through the initial reimbursement,
5. Spare or backup cochlear implant components;
6. Spare or backup auditory osseointegrated device components;
7. Replacement of hearing aids, equipment, cochlear implant components, and auditory
osseointegrated device components if the existing devices are functional, repairable, and
appropriately correct or ameliorate the problem or condition;
8. Spare or backup hearing aids, equipment, or supplies;
9. Repairs to spare or backup hearing aids, cochlear implants, auditory osseointegrated
devices, equipment, or supplies;
10. Investigational or ineffective services or devices, or both;
11. Replacement of improperly fitted ear mold or ear molds unless the:
a. Replacement service is administered by someone other than the original
provider; and
b. Replacement service has not been claimed before;
12. Additional professional fees and overhead charges for a new hearing aid when a
dispensing fee claim has been made to the Program; and
13. Loaner hearing aids.
Preauthorization Requirements
The following information details the preauthorization requirements by the Department for those
billing under Medicaid FFS. The Department‟s clinical criteria for medical necessity can be
found at this link.
https://mmcp.health.maryland.gov/Pages/Provider-Information.aspx

22
Please note that MCOs may have different requirements and criteria. Contact the MCOs directly
for more information about their policies. MCO contact information can be found at:
https://mmcp.health.maryland.gov/Pages/Provider-Information.aspx.
A. The Department requires preauthorization for the following services:
1. All hearing aids;
2. Certain hearing aid accessories;
3. All cochlear implant devices and replacement components except microphone,
transmitter cables and transmitting coils;
4. All auditory osseointegrated devices; and
5. Repairs for hearing aids, cochlear implants, and auditory osseointegrated components
exceeding $500.
B. Preauthorization is valid:
1. For services rendered or initiated within 6 months from the date the preauthorization
was issued; and
2. If the patient is an eligible participant at the time the service is rendered.
C. Effective July 1, 2018, Telligen will be responsible for preauthorizing all hearing aids,
certain hearing aid accessories, all cochlear implant devices, all auditory osseointegrated
devices, repairs exceeding $500, and other cochlear implant and auditory osseointegrated
components exceeding $500.
D. From July 1, 2018 forward, providers are required to submit preauthorization requests
electronically through Telligen‟s web-based provider portal, Qualitrac. Qualitrac is a web
application that allows healthcare providers to submit review requests for consideration. All
of the audiology items on the fee schedule with an asterisk (*) after the reimbursement
amount, will require preauthorization. At this time, the Department requires that all
providers who will submit requests for hearing aids, cochlear implant devices and
components, and auditory osseointegrated devices and components complete a security
registration for Telligen‟s Qualitrac provider portal. Please visit Telligen‟s website at:
http://www.telligenmd.qualitrac.com/document-library.
Once in Qualitrac, download the Security Administrator Registration Form and view the
guide for completion. All providers must complete the security registration prior to prior to
submitting a preauthorization request for audiology services. Sections 3, 4, and 5 of the
packet will need to be completed and sent to Telligen for processing. Section 5 needs to be

23
notarized. If notarization cannot be completed in a timeframe to meet the deadline, the
forms can be faxed to Telligen and the notarized form may be mailed within 30 days. Once
completed documentation is received by Telligen, please allow 3-5 days for processing.
Additionally, Telligen has offered trainings on how to submit preauthorization requests. To
view the training information please visit: http://www.telligenmd.qualitrac.com/education-
training.
E. The following written documentation shall be submitted by the provider to Telligen, the
Department „s designee with each request for preauthorization of hearing aids, cochlear
implants, or auditory osseointegrated devices:
1. Audiology report documenting medical necessity of the hearing aids, cochlear implants
or auditory osseointegrated devices;
2. Interpretation of the audiogram;
3. Medical evaluation by a physician supporting the medical necessity of the initial hearing
aids, cochlear implants or auditory osseointegrated devices within 6 months of the
preauthorization request. (only required for the initial request of the hearing aids,
cochlear implants, or auditory osseointegrated device); and
4. Invoice for the cost of service, minus any discounts, for services reimbursed at
acquisition cost (A/C).
A preauthorization request for hearing aids, cochlear implants, and auditory osseointegrated
device components must be submitted through Telligen‟s web-based provider portal, Qualitrac.
The provider must complete, sign (signature from the audiologist or hearing aid dispenser is
required) and submit the request electronically prior to rendering the service to the participant
to ensure coverage. It is imperative that correct procedure codes be entered with the request.
Omitted information will result in a rejected request.
Determination of authorization is issued via a letter from Telligen after the receipt and review
of the request has been completed. A copy of the notification letter is sent to the provider as
well as to the participant.
Payment Procedures
A. To obtain compensation from the Department for covered services, the provider shall
submit a request for payment on the form designated by the Department.
B. Audiology services are reimbursed in accordance with COMAR 10.09.23.01-1.
C. The provider shall be paid the lesser of:
1. The provider‟s customary charge to the general public, unless the service is free to
24
individuals not covered by Medicaid; or
2. The rate in accordance with the Department‟s fee schedule.
D. The provider may not bill the Department or participant for:
1. Completion of forms and reports;
2. Broken or missed appointments;
3. Professional services rendered by mail or telephone; and
4. Services provided at no charge to the general public.
E. Audiology centers licensed as a part of a hospital may charge for and be reimbursed
according to rates approved by the Health Services Cost Review Commission (HSCRC), set
forth in COMAR 10.37.03.
F. The provider shall refund to the Department payment for hearing aids, supplies, or both, that
have been returned to the manufacturer within the 30-day trial period.
G. The provider shall give the Department the full advantage of any and all manufacturer's
warranties and trade-ins offered on hearing aids, equipment, or both.
H. Unless preauthorization has been granted by the Department or its designee, the Department
is not responsible for any reimbursement to a provider for any service which requires
preauthorization.
I. For audiology services reimbursed at acquisition cost (A/C), the provider must complete and
submit a preauthorization request to Telligen, and include an invoice for their cost for the
service, minus any discount offered to them (if applicable).
J. For services covered by Medicare and when Medicare is the primary payer, the provider
must submit a Medicare Explanation of Benefits (EOB) to the Department with their claim.
An EOB is not required if the service is not covered by Medicare.
K. The Department may not make direct payment to participants.

25
Audiology Procedure Codes & Fee Schedule Effective July 1, 2018
Audiology Services Fee Schedule
Procedure
Code
Description
Maximum
Fee
92550
Tympanometry and reflex threshold measurements (do not
report 92550 in conjunction with 92567, 92568)
$35.00
92551
Screening test, pure tone, air only
$9.72
92552
Pure tone audiometry (threshold); air only
$25.40
92553
Pure tone audiometry (threshold); air and bone
$30.25
92555
Speech audiometry threshold
$18.85
92556
Speech audiometry threshold; with speech recognition
$30.53
92557
Comprehensive audiometry-pure tone, air and bone, and speech
threshold and discrimination - annual audiology assessment
(annual limitation may be waived if medically necessary and
appropriate)
$36.60
92560
Bekesy audiometry; screening
$5.50
92561
Bekesy audiometry; diagnostic
$31.14
92562
Loudness balance test; alternate binaural or monaural
$37.37
92563
Tone decay test
$24.83
92564
Short increment sensitivity index (SISI)
$21.98
92565
Stenger test, pure tone
$13.22
92567
Typanometry (impedance testing) (do not report 92550 or 92568
in addition to 92567)
$20.00
92568
Acoustic reflex testing; threshold (do not report 92550 or 92567
in addition to 92568)
$16.22
92570
Acoustic immittance testing (includes tympanometry,
acoustic reflex threshold, and acoustic reflex decay
testing)
$50.00
92571
Filtered speech test
$21.98
92572
Staggered spondaic word test
$25.44
92575
Sensorineural acuity level test
$47.10

26
Procedure
Code
Description
Maximum
Fee
92576
Synthetic sentence identification test
$29.39
92577
Stenger test, speech
$15.26
92579
Visual reinforcement audiometry
$35.55
92582
Conditioning play audiometry
$53.94
92583
Select picture audiometry
$40.51
92584
Electrocochleography
$70.26
92585
Auditory evoked potentials for evoked response
audiometry
(ABR) comprehensive
$140.00
92586
Auditory evoked potentials for evoked response audiometry
(ABR) - limited
$70.00
92587
Distortion product evoked otoacoustic emissions; limited
evaluation (single stimulus level, either transient or distortion
products)
$50.00
92588
Evoked otoacoustic emissions; comprehensive (comparison of
transient and/or distortion product
otoacoustic emissions at
multiple levels and
frequencies)
$75.00
92590
Hearing aid examination and selection; monaural
$78.00
92591
Hearing aid examination and selection; binaural
$78.00
92592
Hearing aid check; monaural
$42.00
92593
Hearing aid check; binaural
$42.00
92594
Electroacoustic evaluation for hearing aid; monaural
$11.00
92595
Electroacoustic evaluation for hearing aid; binaural
$13.00
92596
Ear protector attenuation measurements
$33.42
92601
Diagnostic analysis of cochlear implant, patient
under 7 years of age; with programming
$140.40
92602
Subsequent reprogramming (do not report 92602 in addition to
92601)
$ 96.30
92603
Diagnostic analysis of cochlear implant, age 7 years or older,
with programming
$118.62

27
Procedure
Code
Description
Maximum
Fee
92604
Subsequent reprogramming (do not report 92604 in addition to
92603)
$70.49
92620
Evaluation of central auditory function, with report; initial 60
minutes
$73.76
92621
Evaluation of central auditory function, with report; each
additional 15 minutes
$17.33
92626
Evaluation of auditory rehabilitation status; first hour (can be
used pre-op and post-op)
$70.21
92627
Evaluation of auditory rehabilitation status; each additional 15
minutes
$17.37
92630
Auditory rehabilitation; pre-lingual hearing loss
$63.99
92633
Auditory rehabilitation; post-lingual hearing loss
$63.99
V5299
Hearing service, miscellaneous (procedure not listed; service not
typically covered, request for consideration. Documentation
demonstrating medical necessity required – to be submitted with
preauthorization request.)
A/C*
Hearing Aid, Cochlear Implant, Auditory Osseointegrated Devices and
Accessories & Supplies Fee Schedule
Procedure
Code
Description
Maximum
Fee
L7510
Repair of prosthetic device/repair or replace minor parts
A/C*
L7520
Repair prosthetic device, labor component
$24.57 per unit,
maximum 12
units
L8614
Cochlear device, includes all internal and external components
$18,853.31*
L8615
Cochlear implant device headset/headpiece, replacement
$428.08
L8616
Cochlear implant device microphone, replacement
$99.71
L8617
Cochlear implant device transmitting coil, replacement
$87.09
L8618
Cochlear implant or auditory osseointegrated device transmitter
cable, replacement
$24.89

28
Procedure
Code
Description
Maximum
Fee
L8619
Cochlear implant external speech processor and controller, integrated
system, replacement
$8,093.59*
L8621
Zinc air battery for use with cochlear implant device and auditory
osseointegrated sound processors, replacement, each
$0.59
L8622
Alkaline battery for use with cochlear implant device, any size,
replacement, each; maximum 180 for unilateral or 360 per 12 month
period for bilateral
$0.30
L8623
Lithium ion battery for use with cochlear implant device speech
processor, other than ear level, replacement, each
$61.39
L8624
Lithium ion battery for use with cochlear implant or auditory
osseointegrated device speech processor, ear level, replacement, each
$153.07
L8625
External recharging system for battery for use with cochlear implant
or auditory osseointegrated device, replacement only, each
$179.25
L8627
Cochlear implant, external speech processor, component,
replacement
$6,914.53*
L8628
Cochlear implant, external controller component, replacement
$1,179.04*
L8629
Transmitting coil and cable, integrated, for use with cochlear implant
device, replacement
$169.95
L8690
Auditory osseointegrated device, includes all internal and external
components
$4,515.27*
L8691
Auditory osseointegrated device, external sound processor, excludes
transducer/actuator, replacement only, each
$1,634.56*
L8692
Auditory osseointegrated device, external sound processor, used
without osseointegration, body worn, includes headband or other
means of external attachment
$2,503.41*
L8693
Auditory osseointegrated device, abutment, any length, replacement
only
$1,439.22*
L8694
Auditory osseointegrated device, transducer/actuator, replacement
only, each
$896.34*

29
Procedure
Code
Description
Maximum
Fee
V5014
Repair/Modification of Hearing Aid
$250.00
V5160
Dispensing fee, binaural
$175.00
V5171
Hearing aid, contralateral routing device, monaural. ITE
$1,190.00*
V5172
Hearing aid, contralateral routing device, monaural. ITC
$1,190.00*
V5181
Hearing aid, contralateral routing device, monaural. BTE
$1,190.00*
V5211
Hearing aid, contralateral routing device, binaural. ITE/ITE
$1,190.00*
V5212
Hearing aid, contralateral routing device, binaural. ITE/ITC
$1,190.00*
V5213
Hearing aid, contralateral routing device, binaural. ITE/BTE
$1,190.00*
V5214
Hearing aid, contralateral routing device, binaural. ITC/ITC
$1,190.00*
V5215
Hearing aid, contralateral routing device, binaural. ITC/BTE
$1,190.00*
V5221
Hearing aid, contralateral routing device, binaural. BTE/BTE
$1,190.00*
V5200
Dispensing fee, contralateral, monaural
$106.00
V5240
Dispensing fee, contralateral routing system, binaural
$175.00
V5254
Digital, monaural, CIC
$950.00*
V5255
Digital, monaural, ITC
$950.00*
V5256
Digital, monaural, ITE
$950.00*
V5257
Digital, monaural, BTE
$950.00*
V5258
Digital, binaural, CIC
$1,900.00*
V5259
Digital, binaural, ITC
$1,900.00*
V5260
Digital, binaural, ITE
$1,900.00*
V5261
Digital, binaural, BTE
$1,900.00*
V5241
Dispensing fee, monaural
$106.00

30
Procedure
Code
Description
Maximum
Fee
V5264
Ear mold, not disposable, (limitation = up to 2 per monaural/4 per
binaural per 12 month period)
$27.00
V5266
Replacement battery for use in hearing device maximum 76 per
year for monaural maximum 152 per 12 month period for binaural
$0.58
V5267
Hearing aid supplies /accessories (medically necessary and
effective services. Note: prophylactic ear protection - a copy of the
signed prescription from the primary care doctor, and a
documented history of tympanostomy tube must be on file.)
A/C*
99002
Handling/conveyance service for devices
$15.00
KEY:
* Requires preauthorization for all participants
A/C Acquisition cost

31
VISION CARE SERVICES
Overview
Vision screening and treatment services are included in the comprehensive Early and Periodic
Screening, Diagnosis, and Treatment (EPSDT) program for children and adolescents under 21
years of age. At a minimum, EPSDT must include age-appropriate vision assessments and
services to correct or ameliorate vision problems, including eyeglasses.
Covered Services
All services for which reimbursement is sought must be provided in accordance with the
Maryland Medical Assistance Vision Care Services (COMAR 10.09.14).
The Medical Assistance Program covers the following vision care services:
1. A maximum of one optometric examination to determine the extent of visual
impairment or the correction required to improve visual acuity, every two years for
participants 21 years and older, and a maximum of one optometric examination a year
for participants younger than 21 years old, unless the time limitations are waived by the
Program, based upon medical necessity;
2. A maximum of one pair of eyeglasses a year for participants younger than 21 years old
(unless the time limitations are waived by the Program, based on medical necessity)
which have first quality, impact resistant lenses (except in cases where prescription
requirements cannot be met with impact resistant lenses) and frames which are made of
fire-resistant, first quality material, when at least one of the following conditions are
met:
a. The participant requires a diopter change of at least 0.50;
b. The participant requires a diopter correction of less than 0.50 based on medical
necessity and preauthorization has been obtained from the Program;
c. The participant‟s present eyeglasses have been damaged to the extent that they
affect visual performance and cannot be repaired to effective performance standards,
or are no longer usable due to a change in head size or anatomy; or
d. The participant‟s present eyeglasses have been lost or stolen;
3. Examination and eyeglasses for a participant with a medical condition, other than
normal physiological change necessitating a change in eyeglasses (before the normal
time limits have been met) when a preauthorization has been obtained from the
program;
4. Visually necessary optometric care rendered by an optometrist when these services are:

32
a. Provided by the optometrist or his/her licensed employee;
b. Related to the patient‟s health needs as diagnostic, preventative, curative, palliative,
or rehabilitative services; and
c. Adequately described in the patient‟s record; and
5. Optician services when they are:
a. Provided by the optician or optometrist, or by an employee under their supervision
and control;
b. Adequately described in the patient‟s record; and
c. Ordered or prescribed by an ophthalmologist or optometrist.
Service Limitations
A. The Vision Care Program does not cover the following services:
1. Services not medically necessary;
2. Investigational or experimental drugs or procedures;
3. Services prohibited by the State Board of Examiners in Optometry;
4. Services denied by Medicare as not medically justified;
5. Eyeglasses, ophthalmic lenses, optical aids, and optician services rendered to participants
21 years or older;
6. Eyeglasses, ophthalmic lenses, optical aids, and optician services rendered to participants
younger than 21 years old which were not ordered as a result of a full or partial EPSDT
screen;
7. Repairs, except when repairs to eyeglasses are cost effective compared to the cost of
replacing with new glasses;
8. Repairs for participants 21 or older;
9. Combination or metal frames except when required for proper fit;
10. Cost of travel by the provider;
11. A general screening of the Medical Assistance population;
12. Visual training sessions which do not include orthoptic treatment; and
33
13. Routine adjustments.
B. The optometrist may not bill the Program or the participant for:
1. Completion of forms and reports;
2. Broken or missed appointments;
3. Professional services rendered by mail or telephone;
4. Services which are provided at no charge to the general public; and
5. Providing a copy of a participant‟s record when requested by another licensed provider
on behalf of the participant.
C. An optometrist certified by the Board as qualified to administer diagnostic pharmaceutical
agents may use the following agents in strengths not greater than the strengths indicated:
1. Agents directly or indirectly affecting the pupil of the eye including the mydriatics and
cycloplegics listed below:
a. Phenylephrine hydrochloride (2.5%);
b. Hydroxyamphetamine hydrobromide (1.0%);
c. Cyclopentolate hydrochloride (0.5 - 2.0%);
d. Tropicamide (0.5 and 1.0%);
e. Cyclopentolate hydrochloride (0.2%) with Phenylephrine hydrochloride (1.0%);
f. Dapiprazole hydrochloride (0.5%); and
g. Hydroxyamphetamine hydrobromide (1.0%) and Tropicamide (0.25%);
2. Agents directly or indirectly affecting the sensitivity of the cornea including the topical
anesthetics listed below:
a. Proparacaine hydrochloride (0.5%); and
b. Tetracaine hydrochloride (0.5%);
3. Diagnostic topical anesthetic and dye combinations listed below:
a. Benoxinate hydrochloride (0.4%) - Fluorescein sodium (0.25%); and
b. Proparacaine hydrochloride (0.5%) - Fluorescein sodium (0.25%).
34
D. An optometrist certified by the Board as qualified to administer and prescribe topical
therapeutic pharmaceutical agents is limited to:
1. Ocular antihistamines, decongestants, and combinations thereof, excluding steroids;
2. Ocular antiallergy pharmaceutical agents;
3. Ocular antibiotics and combinations of ocular antibiotics, excluding specially
formulated or fortified antibiotics;
4. Anti-inflammatory agents, excluding steroids;
5. Ocular lubricants and artificial tears;
6. Tropicamide;
7. Homatropine;
8. Nonprescription drugs that are commercially available; and
9. Primary open-angle glaucoma medications, in accordance with a written treatment plan
developed jointly between the optometrist and an ophthalmologist.
E. The Program will only pay for lenses to be used in frames purchased by the Program or to
replace lenses in the participant‟s existing frames, which are defined as those which have
been fitted with lenses and previously worn by the participant for the purpose of correcting
that patient‟s vision.
F. Providers may not sell a frame to a participant as a private patient and bill the Program for
the lenses only.
G. Providers may not bill the Program for lenses when the participant presents new, unfitted
frames which were purchased from another source.
H. Providers may not bill the Program for the maximum allowed fee for frames and collect
supplemental payment from the participant to enable that participant to purchase a desired
frame that exceeds Program limits.
I. If after the provider has fully explained the extent of Program coverage, the participant
knowingly elects to purchase the desired frames and lenses, the provider may sell a
complete pair of eyeglasses (frames and lenses) to a participant as a private patient without
billing the Program.

35
Preauthorization Requirements
A. The following services require written preauthorization:
1. Optometric examinations to determine the extent of visual impairment or the correction
required to improve visual acuity before expiration of the normal time limitations;
2. Replacement of eyeglasses due to medical necessity or because they were lost, stolen or
damaged before expiration of the normal time limitations;
3. Contact lenses;
4. Subnormal vision aid examination and fitting;
5. Orthoptic treatment sessions;
6. Plastic lenses costing more than equivalent glass lenses unless there are six or more
diopters of spherical correction or three or more diopters of astigmatic correction;
7. Absorptive lenses, except cataract; and
8. Ophthalmic lenses or optical aids when the diopter correction is less than:
a. 0.50 D. sphere for myopia in the weakest meridian;
b. + 0.75 D. sphere for hyperopia in the weakest meridian;
c. + 0.75 additional for presbyopia;
d. + 0.75 D. cylinder for astigmatism;
e. A change in axis of 5 degrees for cylinders of 1.00 diopter or more; and
f. A total of 4 prism diopters lateral or a total of 1 prism diopter vertical.
B. Preauthorization is issued when the provider submits to the Program adequate
documentation demonstrating that the service to be preauthorized is medically necessary.
"Medically necessary means that the service or benefit is directly related to diagnostic,
preventive, curative, palliative, rehabilitative or ameliorative treatment of an illness, injury,
disability, or health condition; consistent with current accepted standards of good medical
practice; the most cost efficient service that can be provided without sacrificing
effectiveness or access to care; and not primarily for the convenience of the consumer, their
family or the provider.
C. Preauthorization is valid only for services rendered or initiated within 60 days of the date
the preauthorization is issued.
36
D. Preauthorization must be requested in writing. A Preauthorization Request Form for Vision
Care Services (DHMH 4526) must be completed and submitted to:
Medical Care Operations Administration
Division of Claims Processing
P.O. Box 17058
Baltimore, MD 21203
E. Documentation substantiating medical necessity must be attached to the preauthorization
request. A copy of the patient record report and/or notes describing the service must be
included with the request. If available, include a copy of the laboratory invoice at this time.
Otherwise, a copy of the invoice must be attached to the claim for proper pricing of the item
after the service has been authorized by the Program.
F. Procedure codes followed by a “P” in this manual require written preauthorization.
G. The Program will cover medically justified contact lenses for participants younger than 21
years old. The following criteria are used when reviewing written preauthorization requests
for contact lenses:
1. Monocular Aphakia:
a. When visual acuity of the two eyes is equalized within two lines (standard Snellen
designation);
b. When no secondary condition or disease exists that could adversely alter the acuity of
either eye or contra-indicate such usage; and
c. When tests conclude that disrupted binocular function will be restored and enhanced
when compared to alternative treatment;
2. Anisometropia:
a. When the prescriptive difference between the two eyes exceeds 4.00 diopters (S.E.)
and visual acuity of the two eyes is equalized within two lines;
b. When no secondary condition or disease exists that could adversely alter the acuity of
either eye or contra-indicate such usage; and
c. When tests conclude that disrupted binocular function will be restored and enhanced
when compared to alternative treatment; and
3. Keratoconus/Corneal Dyscrasies:
a. When contact lenses are accepted as the treatment of choice relative to the phase of a
particular condition;
37
b. When the best spectacle correction in the best eye is worse than 20/60 and when the
contact lens is capable of improving visual acuity to better than 20/40 or four lines
better than the best spectacle acuity; and
c. When no secondary condition or disease exists that could adversely alter the acuity of
either eye or contra-indicate such usage.

38
Provider Enrollment
PLEASE NOTE: Under the Maryland Medical Assistance program, optometrists and optical
centers that are part of a physician‟s group cannot bill under the physician‟s provider number.
Services rendered by the optometrist or optical center cannot be billed under the physician‟s
provider number. These providers must complete an enrollment application and be assigned a
Medical Assistance provider number that has been specifically assigned to them. The number
will be used when billing directly to Maryland Medical Assistance for optometric or optical
center services.
Contact the ePREP Call Center at 1-844-463-7768 for assistance with enrolling as a Medicaid
provider for vision services (Provider Type 12). Ophthalmologists are enrolled under Medical
Assistance‟s Physician Program (Provider Type 20), and should follow the regulations and
manual specific to that particular provider type.
Payment Procedures
The provider shall submit requests for payment for vision services as stated in COMAR
10.09.36.
The request for payment must include any required documentation, such as, preauthorization
number, need for combination or metal frame, patient record notes, and laboratory invoices,
when applicable.
The Medical Assistance Program has established a fee schedule for covered vision care
services provided by optometrists and optical centers (MD MA Provider Type 12). The fee
schedule lists all covered services by CPT and national HCPCS codes and the maximum fee
allowed for each service. Vision care providers must bill their usual and customary charge to
the general public for similar professional services.
The provider shall submit a request for payment on the CMS-1500 billing form. The request for
payment must include any required documentation, such as preauthorization number, need for
combination or metal frame, patient record notes, and laboratory invoices, when applicable.
Maryland Medical Assistance Billing Instructions for the CMS-1500 can be obtained from
Provider Relations at (410) 767-5503 or (800) 445-1159 or at the following link
https://mmcp.health.maryland.gov/Pages/Provider-Information.aspx.
The Program will pay professional fees for covered services at the lower of the provider‟s usual
and customary charge or the Program‟s fee schedule. For professional services, providers must
bill their usual and customary charges. The Program will pay for materials at acquisition costs
not to exceed the maximum established by the Program. For materials, providers must bill their
acquisition costs.
39
Where a “By Report” (B/R) status is indicated on the schedule, attach a copy of the lab
invoice to the claim for pricing purposes as well as the records to substantiate medical necessity
(record report/notes describing the service).
When the fee for a vision care procedure is listed as “Acquisition Cost” (A/C) in this manual,
the value of the procedure is based on acquisition cost. Bill the Program the acquisition cost for
the item. The lab invoice substantiating the charge as well as other records must remain on file
for a 6 year period and made available upon request by the Program.
Procedures with a preauthorization requirement (P) must be authorized prior to treating the
patient. If the procedure is authorized, the preauthorization number must appear on the claim.
The provider must select the procedure code that most accurately identifies the service
performed. Any service rendered must be adequately documented in the patient record. The
records must be retained for 6 years. Lack of acceptable documentation may cause the Program
to deny payment or if payment has already been made, to request repayment, or to impose
sanctions, which may include withholding of payment or suspension or removal from the
Program. Payment for services is based upon the procedure(s) selected by the provider.
Although some providers delegate the task of assigning codes, the accuracy of the claim is
solely the provider‟s responsibility and is subject to audit.
The NFAC (Non-Facility) fee is paid for place of service 11, 12, and 62.
The FAC (facility) fee is paid for all other places of service.
Payments for lenses, frames, and the fitting and dispensing of spectacles include any routine
follow-up and adjustments for 60 days. No additional fees will be paid. Providers must bill and
will be paid for the supply of materials at acquisition costs not to exceed the maximum
established by the Program. If a maximum has not been established, the provider must attach
laboratory documentation to the invoice.
Fitting includes facial measurements, frame selection, prescription evaluation and verification
and subsequent adjustments. The maximum fee for lenses includes the cost for FDA hardening,
testing, edging, assembling and surfacing. The maximum fee for frames includes the cost of a
case.
1. Use the following procedure codes for the billing of frames:
a. V2020 for a child/adult ZYL frame;
b. V2025 for a metal or combination frame when required for a proper fit; and
c. V2799 (preauthorization required) for a special or custom frame when necessary
and appropriate.
2. Use procedure codes 92340 - 92342 for the fitting of spectacles.

40
3. Use procedure code 92370 and attach a copy of the lab invoice to the claim when billing
for a repair. PLEASE NOTE: Repair charges not traditionally billed to the general
public cannot be billed to Maryland Medical Assistance. (Review the regulations for
coverage of eyeglass repairs.)
Contact lens services require preauthorization and include the prescription of contact lenses
(specification of optical and physical characteristics), the proper fitting of contact lenses
(including the instruction and training of the wearer, incidental revision of the lens and
adaptation), the supply of contact lenses, and the follow-up of successfully fitted extended wear
lenses. Use the following procedure codes for the billing of these services:
1. 92310-26 for the professional services of prescription, fitting, training, and adaptation;
2. V2500 - V2599, S0500 for contact lenses;
3. V2784 for polycarbonate lenses; and
4. 92012 for follow-up subsequent to a proper fitting.
Vision care claims must be received within 12 months of the date that services were rendered.
If a claim is received within the 12 month limit but rejected due to erroneous or missing data,
re-submittal will be accepted within 60 days of rejection or within 12 months of the date that
the service was rendered, whichever is later. If a claim is rejected because of late receipt, the
participant may not be billed for that claim.
Medicare/Medical Assistance crossover claims must be received within 120 days of the date
that payment was made by Medicare. This is the date of Medicare‟s Explanation of Benefits
form. The Program recognizes the billing time limitations of Medicare and will not make
payment when Medicare has rejected a claim due to late billing.
The Medical Assistance Program is always the payer of last resort. Whenever a Medical
Assistance participant is known to be enrolled in Medicare, Medicare must be billed first.
Claims for Medicare/Medical Assistance participants must be submitted on the CMS-1500
directly to the Medicare Intermediary.
For additional information about the MD Medical Assistance Program, go to the following link:
https://mmcp.dhmh.maryland.gov/Pages/Provider-Information.aspx.
A copy of the regulations can be viewed at:
http://www.dsd.state.md.us/COMAR/subtitle_chapters/Titles.aspx (title 10) (subtitle 09)
10.09.14.

41
Preauthorization Required Prior To Treatment
When the fee for a vision care procedure is listed as “By Report” (B/R) on this schedule a
copy of the optometrist‟s patient record report and/or notes which describe the services
rendered and the lab invoice must be submitted with the claim.
When the fee for a vision care procedure is listed as “Acquisition Cost” (A/C) on this
schedule, the value of the procedure is to be determined from a copy of a current laboratory or
other invoice which clearly specifies the unit cost of the item.
When the fee for a vision care procedure is listed with a "P", a request for
preauthorization must be submitted on form DHMH 4526. A copy of the patient record
report and/or notes describing the services must be submitted to the Program prior to
rendering the service.
The maximum fee for lenses includes the cost for FDA hardening, testing, edging, assembling
and surfacing. The maximum fee for frames includes the cost of a case
Services provided must be medically necessary.
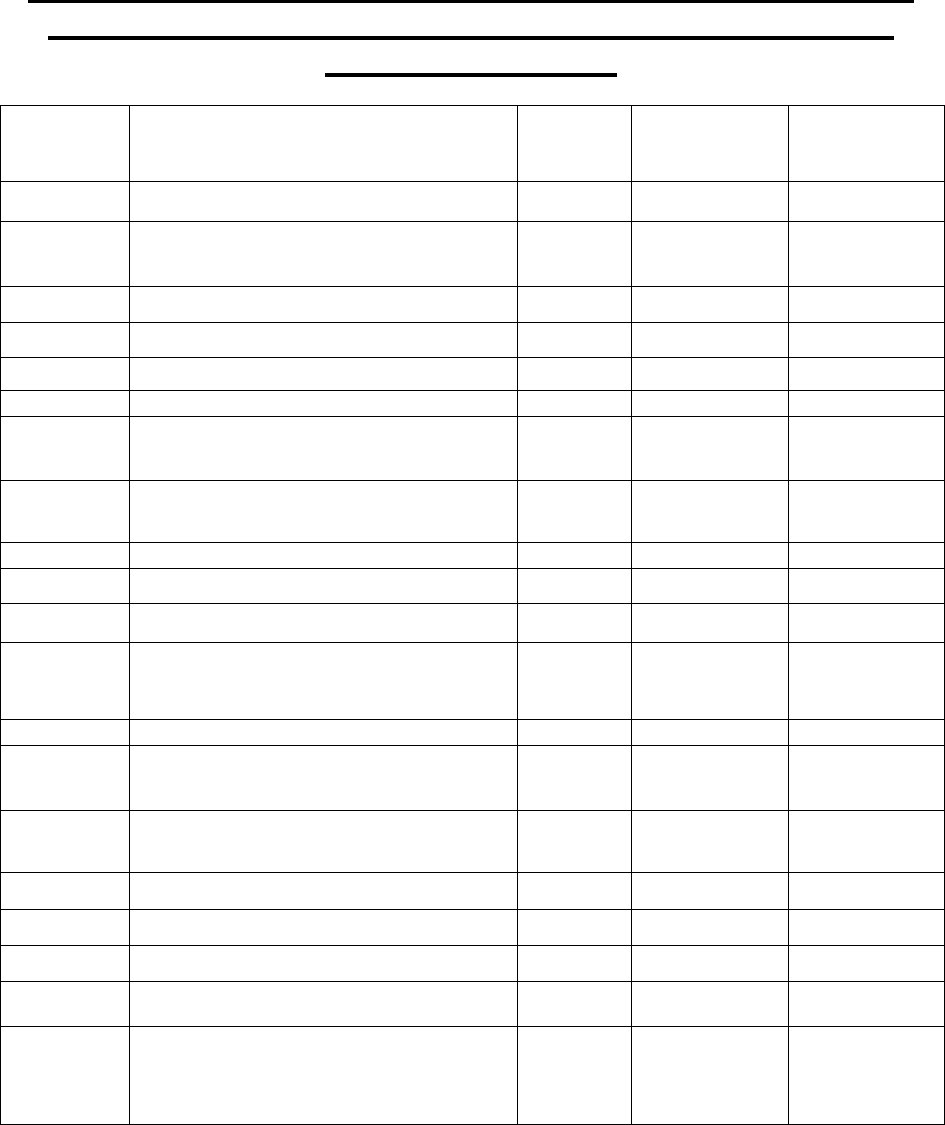
42
Professional Services/Materials Reimbursements for Vision Care
Providers (Provider Type 12 Non-facility & Facility Included)
Effective July 1, 2018
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Payment
NFAC
Maximum
Payment
FAC
65205
Removal of foreign body from eye
$ 44.11
$ 34.43
65210
Removal of foreign body embedded in
eye
$ 53.88
$ 41.63
65220
Removal of foreign body w/o lamp
$ 45.98
$ 33.43
65222
Removal of foreign body w/ lamp
$ 52.46
$ 40.77
92002
Eye exam w/new patient
$ 63.71
$ 37.20
92004
Eye exam w/new patient comprehensive
$ 116.51
$ 77.46
92012
Eye exam and treatment of established
patients
$ 67.09
$41.15
92014
Eye Exam and treatment of establish
patients, comprehensive
$ 96.99
$62.22
92015
Determination of Refractive state
$ 19.02
$15.03
92020
Special Eye Evaluation - Gonioscopy
$ 21.00
$16.43
92025
Computerized Corneal Topography
$ 29.90
$ 29.90
92060
Sensorimotor exam with multiply
measure
Ocular deviation
$ 51.21
$ 51.21
92065
Orthoptic/pleoptic training
P
$ 42.98
$ 42.98
92071
Fitting contact lens for treatment of
ocular surface disease
$ 31.59
$28.03
92072
Fitting contact lens for management of
keratoconus initial fitting
$ 104.54
$80.01
92081
Visual field exam(s) limited
$ 33.37
$ 33.37
92082
Visual field exam(s) Intermediate
$ 49.38
$ 49.38
92083
Visual field exam(s) extended
$ 56.74
$ 56.74
92100
Serial Tonometry exam(s)
$ 63.33
$34.29
92132
Scanning Computerized ophthalmic
diagnostic imaging anterior segment,
with interpretation and report
$ 30.41
$ 30.41
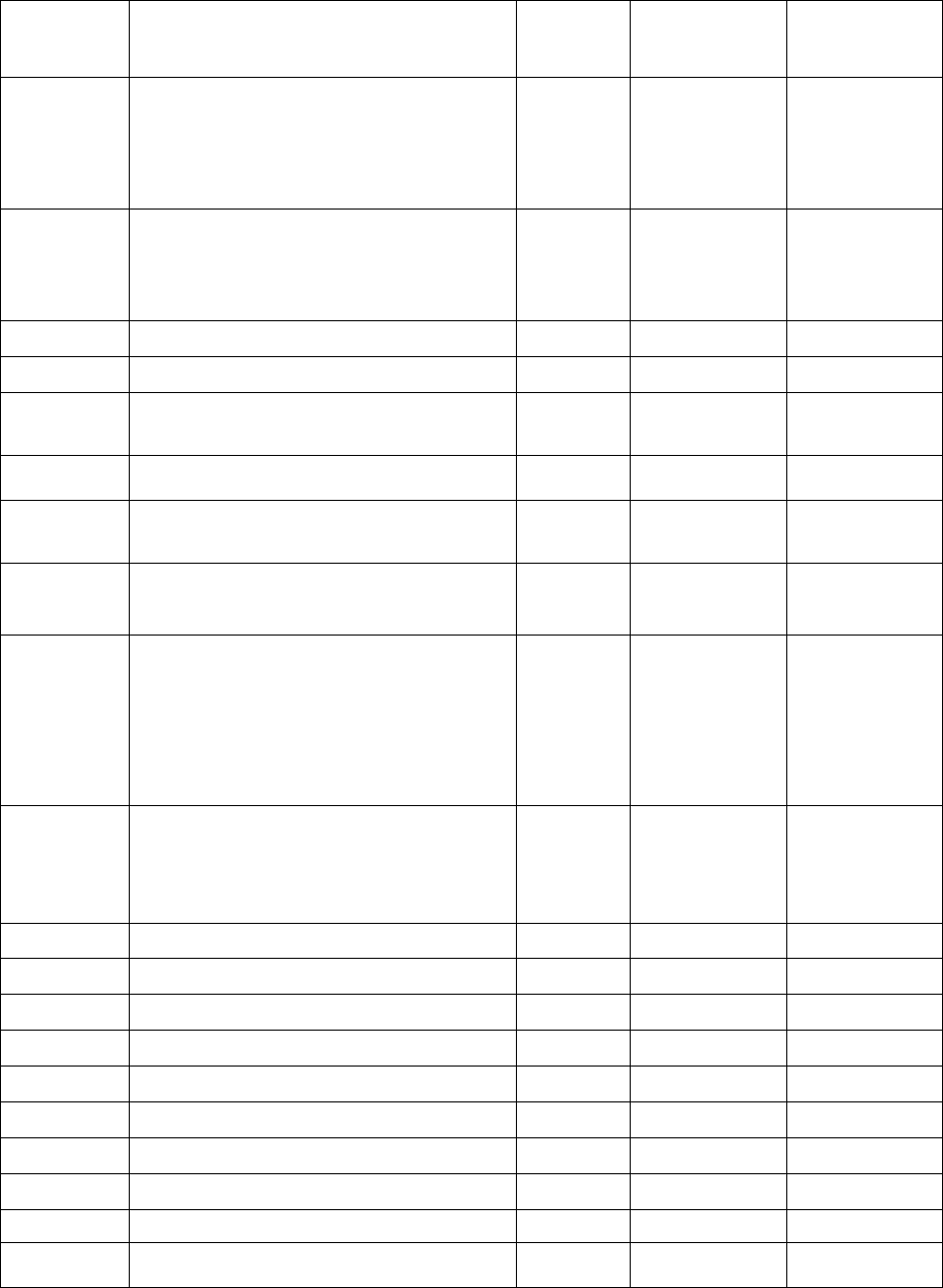
43
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Payment
NFAC
Maximum
Payment
FAC
92133
Scanning Computerized ophthalmic
diagnostic imaging posterior segment,
with interpretation and report unilateral
or bilateral; optic nerve
$ 37.09
$ 37.09
92134
Scanning Computerized ophthalmic
diagnostic imaging posterior segment,
with interpretation and report unilateral
or bilateral; retina
$ 37.09
$ 37.09
92225
Ophthalmoscopy, initial
$ 20.98
$16.70
92226
Ophthalmoscopy, subsequent
$ 19.36
$14.80
92250
Fundus photography w/ interpretation
and report
$ 53.55
$ 53.55
92260
Ophthalmodynamometry
$ 14.48
$8.49
92283
Color vision examination extended, e.g.,
anomaloscope or equivalent
$ 44.78
$ 44.78
92284
Dark adaptation examination w/
interpretation and report
$ 51.16
$ 51.16
92285
External ocular photography w/
interpretation and report for
documentation of medical progress (e.g.,
close-up photography, slit lamp
photography, goniophotography, stereo-
photography)
$ 30.13
$ 30.13
92286
Special anterior segment photography
w/interpretation and report; with specular
endothelial microscopy and cell count.
$ 93.71
$ 93.71
92310
Contact lenses fitting
P
$ 75.28
$ 46.21
92311
Contact lens fitting - 1/aphakia
P
$ 79.33
$ 43.13
92312
Contact lens fitting - 1/aphakia
P
$ 92.38
$ 49.91
92313
Contact lens fitting - 1/aphakia
P
$ 75.89
$ 36.56
92314
Fitting Special Contact lens
$ 62.97
$ 27.34
92325
Modification of contact lens
P
$ 33.95
$ 33.95
92326
Replacement of contact lens
P
$ 36.82
$ 36.82
92340
Fitting of spectacles, monofocal
$ 27.88
$ 14.48
92341
Fitting of spectacles, bifocal
$ 31.71
$ 18.60
92342
Fitting of spectacles, multifocal
$ 34.16
$ 20.77

44
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Payment
NFAC
Maximum
Payment
FAC
92354
Fitting of spectacle mounted low vision
aid; single element system
P
$ 61.53
$ 61.53
92355
Fitting of spectacle mounted low vision
aid; telescopic or other compound lens
system
P
$ 43.11
$ 43.11
92370
Repair & refitting spectacles
$ 24.26
$12.58

45
Professional Services/Materials Reimbursements for Vision Care
Providers (Provider Type 12 –Facility Only)
Effective July 1, 2018
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Payment
FAC
92499
Unlisted eye service or procedure
B.R.
S0500
Disposable contact lens, per lens
P
A.C.
V2020
Adult/child ZYL frames w /case
$ 20.00
V2025
Metal or combination frame
$ 25.00
V2100
Lens sphere single plano 4.00, per lens
$ 12.00
V2101
Single vision sphere 4.12 - 7.00, per lens
$ 7.20
V2102
Single vision sphere 7.12 - 20.00, per lens
$ 22.15
V2103
Spherocylinder, SV, 4.00d/.12-2.00, per lens
$ 15.00
V2104
Spherocylinder, SV, 4.00d/2.12-4d, per lens
$ 15.00
V2105
Spherocylinder, SV,4.00d/4.25-6d, per lens
$ 7.30
V2106
Spherocylinder, SV,4.00d/over6.00d, per lens
A.C.
V2107
Spherocylinder, SV,+-4.25d/.12-2d, per lens
$ 15.00
V2108
Spherocylinder, SV,+-4.25d/2.12-4d, per lens
$ 15.00
V2109
Spherocylinder, SV,+-4.25d/4.25-6d, per lens
$ 9.20
V2110
Spherocylinder, SV,+-4.25d/over 6d, per lens
B.R.
V2111
Spherocylinder, SV,+-7.25d/.25-2.25d, per lens
$ 22.15
V2112
Spherocylinder, SV,+-7.25d/2.25-4d, per lens
$ 19.00
V2113
Spherocylinder, SV,+-7.25d/4.25-6d, per lens
A.C.
V2114
Spherocylinder, SV, over +-12.00d, per lens
$ 36.00
V2115
Lenticular (myodisc), SV, per lens
B.R.
V2118
Aniseikonic lens, SV
P
A.C.
V2121
Lenticular lens, Per Lens, Single, per lens
A.C.
V2199
Not otherwise classified, SV lens
P
A.C.
V2200
Sphere, bifcl, plano +-4.00d, per lens
$ 21.00
V2201
Sphere, bifcl,+-4.12/+-7.00d, per lens
$ 13.00
V2202
Sphere ,bifcl,+-7.12/+-20d, per lens
A.C.
V2203
Spherocylinder, BF, 4.00d/.12-2.00d, per lens
$ 21.00
V2204
Spherocylinder, BF, 4.00d/2.12-4, per lens
$ 14.50
V2205
Spherocylinder, BF, 4.00d/4.25-6, per lens
$ 16.50
V2206
Spherocylinder, BF, 4.00d/over 6, per lens
B.R.
V2207
Spherocylinder, BF, 4.25-7/.12 to 2, per lens
$ 14.50
V2208
Spherocylinder, BF, 4.25+-7/2.12 to 4, per lens
$ 15.50
V2209
Spherocylinder, BF, 4.25+-7/4.25-6, per lens
$ 17.50
V2210
Spherocylinder, BF, 4.25+-7/over 6, per lens
A.C.
V2211
Spherocylinder, BF, 7.25+-12/.25-2.25, per lens
A.C.
V2212
Spherocylinder, BF, 7.25+-12/2.25-4, per lens
A.C.
V2213
Spherocylinder, BF, 7.25+-12/4.25-6, per lens
A.C.
V2214
Spherocylinder, BF, sphere over +-12.00d, per
lens
A.C.
V2215
Lenticular (myodisc) bifocal, per lens
B.R.

46
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Payment
FAC
V2218
Aniseikonic, bifocal, per lens
P
A.C.
V2219
Bifocal seg width over 28 mm
P
A.C.
V2220
Bifocal add over 3.25d
P
A.C.
V2221
Lenticular lens, bifocal, per lens
$ 24.00
V2299
Specialty bifocal
P
A.C.
V2300
Sphere, trifcl, pl+-4.00d, per lens
$ 16.50
V2301
Sphere, trifcl +-4.12/-7.00d, per lens
$ 19.00
V2302
Sphere, trifcl +-7.12/+-20.00, per lens
A.C.
V2303
Spherocylinder, trifcl, pl+-4/.12-2, per lens
$ 18.00
V2304
Spherocylinder, trifcl, p+-4/2.25-4, per lens
$ 20.50
V2305
Spherocylinder, trifcl, p+-4/4.25-6, per lens
$ 24.00
V2306
Spherocylinder, trifcl, p+-4/over 6, per lens
A.C.
V2307
Spherocylinder, trifcl, +-4.25/…2d, per lens
$ 20.50
V2308
Spherocylinder, trifcl, +-4.25/…4d, per lens
$ 22.00
V2309
Spherocylinder, trifcl, +-4.25/…6d, per lens
$ 25.00
V2310
Spherocylinder, trifcl, +-4.25/over 6d, per lens
A.C.
V2311
Spherocylinder, trifcl, +-7.25/…2.25d, per lens
A.C.
V2312
Spherocylinder, trifcl ,+-7.25/…4.00d, per lens
A.C.
V2313
Spherocylinder, trifcl, +-7.25/…6.00d, per lens
A.C.
V2314
Spherocylinder, trifcl, over p-12.00d, per lens
A.C.
V2315
Lenticular (myodisc), trifocal, per lens
A.C.
V2318
Aniseikonic lens, trifocal
P
A.C.
V2319
Trifocal seg width over 28 mm
P
A.C.
V2320
Trifocal add over 3.25d
P
A.C.
V2321
Lenticular lens, trifocal, per lens
A.C.
V2399
Specialty trifocal (by report)
P
A.C.
V2410
Variable asph, SV, full fld,gl/pl
P
A.C.
V2430
Variable asph, bifcl, full fld,gl/pl
P
A.C.
V2499
Variable sphericity, other type
P
A.C.
V2500
Contact lens, PMMA spherical
P
A.C.
V2501
Contact lens PMMA toric/prism
P
A.C.
V2502
Contact lens PMMA bifocal
P
A.C.
V2503
Contact lens PMMA color vision def
P
A.C.
V2510
Contact lens, gas permeable, spherical, per lens
P
A.C.
V2511
Contact lens, gas permeable, toric, prism ballast,
per lens
P
A.C.
V2512
Contact lens, gas permeable, bifocal, per lens
P
A.C.
V2513
Contact lens, gas permeable, extended wear, per
lens
P
A.C.
V2520
Contact lens, hydrophilic, spherical, per lens
P
A.C.
V2521
Contact lens, hydrophilic, toric, or prism ballast,
per lens
P
A.C.
V2522
Contact lens, hydrophilic, bifocal, per lens
P
A.C.
V2523
Contact lens, hydrophilic, extended wear, per
lens
P
A.C.
V2530
Contact lens, scleral, gas imperm, per lens
P
A.C.

47
Procedure
Code
Description
Requires
Pre-Auth
Maximum
Payment
FAC
V2599
Contact lens, other type
P
A.C.
V2600
Hand held low vision aids
P
A.C.
V2610
Single lens spectacle mount low vision aids
P
A.C.
V2615
Telescopic & other compound lens
P
A.C.
V2700
Balance lens
A.C.
V2715
Prism lens
P
A.C.
V2718
Press-on lens, Fresnel prism
P
A.C.
V2745
Add. tint, any color/solid/grad
B.R.
V2784
Polycarbonate lens, any index (Greater than 6
Diopters or other medically necessary
condition)
$6.50
V2799
Vision service, miscellaneous
P
A.C.

48
ATTACHMENT A: MARYLAND MEDICAL ASSISTANCE
PROGRAM FREQUENTLY REQUESTED TELEPHONE
NUMBERS
Audiology Policy/Coverage Issues
(410) 767-3998
Vision Policy/Coverage Issues
(410) 767-3998
Healthy Start/Family Planning Coverage
(800) 456-8900
Maryland Medical Assistance Children’s Services
(410) 767-3998
Rare and Expensive Case Management Program (REM)
(800) 565-8190
Eligibility Verification System (EVS)
(866) 710-1447
Board of Audiologists/Hearing Aid
Dispensers/Speech Language Pathologists
(410) 764-4725
Maryland Board of Acupuncture
(410) 764-4766
Maryland Board of Examiners in Optometry
(410) 764-4710
Maryland Board of Audiologists, Hearing Aid
Dispensers, and Speech-Language Pathologists
(410) 764-4725
Maryland Board of Chiropractic Examiners
(410) 764-4738
Maryland Board of Dietetic Practice
(410) 764-4733
Maryland Board of Occupational Therapy Practice
(410) 402-8556
Maryland Board of Physical Therapy Examiners
(410) 764-4718
Provider Enrollment
(410) 767-5340
Electronic Provider Revalidation and Enrollment Portal
(ePREP)
(844) 463-7768
Provider Relations
P.O. Box 22811
Baltimore, MD 21203
(410) 767-5503
(800) 445-1159

49
Missing Payment Voucher/Lost or Stolen Check
(410) 767-5503
Third Party Liability/Other Insurance
(410) 767-1771
Recoveries
(410) 767-1783
50
ATTACMENT B: HEALTH INSURANCE CLAIM FORM
(SEE NEXT PAGE)

51
PLEASE PRINT OR TYPE
APPROVED OMB-0938-1197
FORM 1500 (02-12)

52
ATTACHMENT C: MARYLAND DEPARTMENT OF HEALTH
PREAUTHORIZATION REQUEST FORM - VISION CARE
SERVICES
SECTION I - Patient Information
Medicaid Number
Last Name First Name MI
DOB Sex Telephone
Address
SECTION II - Preauthorization General Information
Pay to Provider Number
Name Date Service
Address Requested by
Contact Provider
Provider’s Signature Telephone ( )
SECTION III – Additional Preauthorization Information
Give Reason(s) for Requested Service
SECTION IV – Preauthorization Line Item Information
DESCRIPTION
OF SERVICE
PROCEDURE
CODE
REQUESTED
AUTHORIZED
UNITS
AMOUNT
UNITS
AMOUNT
$
$
$
$
$
$
$
$
$
$

53
PREAUTHORIZATION NUMBER
DOCUMENT CONTROL NUMBER SUBMIT TO: Program Systems and Operations Administration
(STAMP HERE) Division of Claims Processing
P.O. Box 17058
Baltimore, Maryland 21203
SECTION V – Specific Preauthorization Information
New Prescription: O.D. Best Visual Activity
O.D. Best Visual Activity
CONTACT LENS REQUESTS:
Health Condition of each eye: O.D. O.S.
Date of Surgery: O.D. O.S.
Best visual acuity with contact lenses: O.D. O.S.
Advantage of contact lenses over glasses:
SECTION VI (DHMH Only)
Approved Denied Returned
Reason(s)
Medical Consultant’s Signature Date
