
1
MID-STATE HEALTH NETWORK
SUBSTANCE USE DISORDER SERVICES
PROVIDER MANUAL
Effective Date: October 1, 2022
Revised: September 1, 2022
Approved by: CEO, July 2022
Deputy Director, July 2022
SUD Medical Director, 2022

2
Table of Contents
Introduction 5
Governing Authorities and Prepaid Inpatient Health Plan (PIHP) Requirements 5
Definitions 8
CUSTOMER SERVICE AND RECIPIENT RIGHTS 15
Customer Service 15
Recipients Rights for Substance Use Disorder Services 16
COMPLIANCE 17
Confidentiality, Privacy & Release of Information 17
Breach Notification 18
Documentation & Records 19
Reporting Requirements & Delinquency Procedure 19
QUALITY IMPROVEMENT 21
Annual Consumer Satisfaction Surveys 21
Michigan Mission Based Performance Indicator System (MMBPIS) 21
Sentinel Events 22
PROVIDER NETWORK MANAGEMENT 23
Organizational Credentialing and Recredentialing 23
Delegation of Rendering Provider Credentialing and Recredentialing 23
Quality Assurance and Performance Improvement 24
Capacity 24
Notification of Termination/Closure 24
Employee Confidentiality 25
REMI Provider Portal 25
Training and Continuing Education 26
Contract Non-Compliance 27
TREATMENT SERVICES 28
Annual Plans 28
Auricular Acupuncture 28
Biopsychosocial Assessment 28
Co-Occurring Mental Health and Substance Use Disorders 29
Cultural Competency 29
Discharge Planning 30

3
Documentation Standards 30
Evidence-Based Practices 31
Gambling Disorder Protocol 31
Group Therapy 32
Individualized Treatment Planning 33
Integrated Coordination of Care 33
Jail-Based Services 34
MDOC Priority Population Technical Requirements 35
Medication Assisted Treatment (MAT) 36
Opioid Health Home 37
Performance Enhancement Plan (PEP) 38
Prohibition on Provision of Hypodermic Needles 39
Project ASSERT & SBIRT Programs 39
Recovery Oriented Systems of Care 40
Telemedicine 40
Transfer 41
Trauma Informed Care 41
Trauma-Specific Services 42
Veteran Services 43
Warm Transfer 44
FINANCE AND CLAIMS 46
General Business Requirements 46
Medicaid Verification/Reimbursement 46
Healthy Michigan Plan (HMP) 46
Provider Authorizations & Claims 47
Medicaid Recipients with other Primary Insurance 47
Reimbursable Diagnoses 49
Service Codes & Rates 49
Specialty Grant Funding 49
UTILIZATION MANAGEMENT 51
Access to Services 51
Eligibility Determination & Medical Necessity 51

4
Block Grant Funding 52
Out of Region & Out of Network Services 53
Types of Utilization Review 53
SUD Benefit Plans 55
Authorizations 55
REMI Admissions, Discharges, Transfers 56
Provider Appeal Process 58
PREVENTION PROVIDERS 60
Prevention Services 60
Coordination of Services 62
Program Evaluation 62
Charging for Prevention Services 63
Prevention Activity Reporting 63
Designated Youth Tobacco Use Representatives (DYTURs) 64
DYTUR Reporting 65
Early Intervention-Prevention 65
Community Coalitions 66
SELECTED REFERENCES 67
Appendix A: MSHN MAT Protocol 69
Appendix B: Recovery Housing Technical Requirement 82
Appendix C: Technical requirement for SUD Transportation Services 87
Appendix D: MSHN Informed Consent Related to MAT 89
Appendix E: Informational Grid on Recovery Pathways for Opioid Use Disorder (OUD)
90

5
MID-STATE HEALTH NETWORK
SUBSTANCE USE DISORDER SERVICES
PROVIDER MANUAL
Introduction
Welcome to the Mid-State Health Network (MSHN) substance use disorder (SUD) services
provider manual. MSHN is pleased to be partnering with SUD prevention, treatment, and
recovery support services providers that offer an array of services throughout MSHN’s 21-
county region. The purpose of this manual is to offer information and technical assistance
regarding the requirements associated with provider contracted role(s). This manual is a
referenced attachment to your contract for MSHN services and may be revised accordingly in
response to changes in contract requirements and/or MSHN policies and procedures. MSHN will
notify providers of effective changes. The most current version of the manual, along with a
change log will be posted to the MSHN Website: Provider Network→Substance Use
Disorder→Provider Manuals.
For the most current listing of MSHN staff, including contact information, visit the MSHN
Website: Stakeholders → Contact.
MSHN utilizes a 2-Year Strategic Plan, inclusive of the SUD Prevention, Treatment & Recovery
provider system. The FY22-23 was approved by the MSHN Board of Directors in 2021 and it
identifies current priorities for behavioral health services, including SUD within the region. In
FY22-23 MSHN expanded from the quadruple aim—Better Health, Better Care, Better Value,
and Better Provider Systems—to include a 5
th
strategic priority, Better Equity, to reflect MSHN’s
commitment to overcoming longstanding health disparities between different sub-populations
across Michigan and the U.S. MSHN also has an SUD-specific Strategic Plan for FY21-23 for SUD
prevention, treatment, and recovery efforts for the region. Prevention efforts are focused on
reducing underage drinking, marijuana use, opioid prescription use, youth tobacco and nicotine
use, and substance use in older adults. Treatment efforts are focused on increasing accessibility
of services (MAT, stimulant use treatment, WSS, jail-based services, and trauma-informed
care), expanding penetration rates for adolescents, older adults and veterans/military families,
increasing cultural competence and reducing health disparities.
During the COVID-19 State of Emergency; Federal and/or State policy or Executive Orders
issued and in effect beginning on March 10, 2020, including any modifications of such Executive
Orders or policies in relation to COVID-19, issued after that date, that provide different
guidance or requirements than are currently identified and stated within the provider
agreement and/or this manual and/or MSHN’s policies, procedures, or regional guidance the
PROVIDER shall follow the federal and/or state direction and guidance as it relates to the
COVID-19 State of Emergency. Please refer to the MSHN Coronavirus Disease webpage found
HERE for further information.
Governing Authorities and Prepaid Inpatient Health Plan (PIHP)
Requirements
MSHN is under contract with the Michigan Department of Health and Human Services (MDHHS),
with all the associated obligations and requirements for the use of public funds. As one of the
10 PIHPs in Michigan, MSHN has provider network management obligations including but not

6
limited to, assurance of overall federal, state, and other compliance mandates, regional service
array adequacy, and ensuring provider competency expectations are met in both professional
enhancement and service delivery areas.
Key references for SUD services are on the MSHN website: Provider Network→Provider
Requiremenst→Substance Use Disorder and include:
• MSHN SUD Prevention Provider contract
• MSHN SUD Treatment Provider contract
• MSHN SUD Recovery Housing Provider contract
• MSHN & MDHHS Contract, Substance Use Disorder Policy Manual
• MDHHS Office of Recovery Oriented Systems of Care (OROSC) policies & advisories
• LARA Licensing, Certification, Training
• Medicaid Provider Manual, Chapter: Behavioral Health and Intellectual and
Developmental Disability Supports and Services
• SAMHSA mental and substance use disorders
• MDHHS Provider Qualifications Chart
• Medicaid Services Administration (MSA) Bulletins
Providers are expected to adhere to all standards, requirements, and legal obligations contained
in these referenced MDHHS guidance and requirement documents applicable to the specific
services being purchased and provided. For efficiency, MSHN will highlight but will not
duplicate, in entirety, the information found in the above-mentioned references. Providers are
responsible for understanding, demonstrated through service delivery, the content pertinent
to the scope of work identified in contract. MSHN will make every effort to inform SUD providers
about policy, procedure, or other requirement change(s).
For convenience, MSHN has policies and procedures posted on the MSHN website: Provider
Network→Provider Requirements→Policies and Procedures: Applicable MSHN policies and
procedures for SUD providers include, but are not limited to:
• Advance Directives
• Behavioral Health Recovery Oriented Systems of Care
• Background Checks
• Breach Notification
• Compliance and Program Integrity
• Compliance Reporting and Investigation
• Confidentiality and Notice of Privacy
• Conflict of Interest Policy
• Consent to Share Information
• Consumer Satisfaction
• Credentialing and Re-Credentialing Policy
• Credentialing and Recredentialing - Licensed Independent Practitioners
• Critical Incidents
• Cultural Competency
• Customer Service (Policy and Procedure)
• Disclosure of Ownership, Control, and Criminal Convictions.
• Disqualified Individuals
• Evidence-Based Practices

7
• Income Eligibility for Non-Medicaid Services (Policy & Procedure)
• Medicaid Enrollee Appeals/Grievances
• Medicaid Event Verification (Policy and Procedure)
• Medicaid Information Management
• Michigan Mission Based Performance Indicator System
• Monitoring and Oversight
• Non-Licensed Provider Qualifications
• Performance Improvement Policy
• Provider Appeal Procedure
• Provider Contract Non-Compliance Procedure
• Provider Network Management
• Quality Management
• Recipient Rights for Substance Use Disorder Recipients
• Record Retention
• Service Philosophy, Access System
• Service Provider Reciprocity
• Sentinel Events
• SUD Services – Women’s Specialty Services (Policy & Procedure)
• Use of Public Act 2 Dollars
• Trauma Informed Systems of Care
MSHN’s governing Board of Directors (BOD) includes representation from each of the 12
Community Mental Health Service Programs (CMHSP) in the region. The BOD has policy and
fiduciary responsibilities for all contracts with MDHHS including SUD administration and
services. Additionally, and as required by statute, the MSHN PIHP region has an SUD Oversight
Policy Board (OPB), whose members represent each of the 21 counties in the region. The OPB
is an advisory to the BOD and serves as the authority for approving use of Public Act 2 funds.
The list of these board members can be found on the MSHN website: Stakeholders→Boards &
Councils, along with a calendar of regional meetings.
MSHN welcomes the opportunity to enhance SUD partnerships and appreciates feedback
regarding SUD services. Please contact MSHN staff to share knowledge, concerns and/or
expertise.

8
Definitions
Abuse includes practices that are inconsistent with sound fiscal, business or medical practices
and result in an unnecessary cost to the payor, or in reimbursement for services that are not
medically necessary or fail to meet professionally recognized standards for healthcare.
Admission is that point in a consumer’s relationship with an organized treatment service when
the intake process has been completed and the consumer is determined eligible to receive
services of the treatment program.
Amount refers to the number of units (e.g., 25 15-minute units of community living supports)
of service identified in the individual plan of service or treatment plan to be provided.
AMS refers to the Access Management System which is required by the Michigan Department
of Health and Human Services (MDHHS) to screen, authorize, refer and provide follow-up
services.
Appeal is a review at the local level by a PIHP of an Adverse Benefit Determination, as defined
above. 42 CFR 438.400.
ASAM refers to the American Society for Addiction Medicine. It is the medical association
for Addictionists. The members developed the patient placement criteria, the most recent of
which is
The ASAM Patient Placement Criteria
,
3
rd
Edition
.
Assessment includes those procedures by which a qualified clinician evaluates an individual’s
strengths, areas identified for growth, problems, and needs to establish a SUD diagnosis and
determine priorities so that a treatment plan can be developed.
Breach is an impermissible use or disclosure under the HIPAA Privacy Rule that compromises
the security or privacy of the protected health information.
Care Coordination means a set of activities designed to ensure needed, appropriate and cost-
effective care for consumers. As a component of overall care management, care coordination
activities focus on ensuring timely information, communication, and collaboration across a care
team and between Responsible Plans. Major priorities for care coordination in the context of a
care management plan include:
• Outreach and contacts/communication to support patient engagement,
• Conducting screening, record review, and documentation as part of Evaluation and
Assessment,
• Tracking and facilitating follow-up on lab tests and referrals,
• Care Planning,
• Managing transitions of care activities to support continuity of care,
• Address social supports and making linkages to services addressing housing, food, etc.,
and
• Monitoring, Reporting and Documentation.

9
Case Management refers to a substance use disorder case management program that
coordinates, plans, provides, evaluates and monitors services or recovery from a variety of
resources on behalf of and in collaboration with a consumer who has a substance use disorder.
A substance use disorder case management program offers these services through designated
staff working in collaboration with the substance use disorder treatment team and as guided by
medical necessity and the individualized treatment planning process.
CMHSP Participant refers to one of the twelve-member Community Mental Health Services
Program (CMHSP) participant in the Mid-State Health Network.
Continued Service Criteria is when, in the process of consumer assessment, certain
problems and priorities are identified as justifying admission to a particular level of
care. Continued Service Criteria describe the degree of resolution of those problems and
priorities and indicate the intensity of services needed. The level of function and clinical
severity of a consumer’s status in each of the six assessment dimensions of ASAM is considered
in determining the need for continued service.
Continuum of Care refers to an integrated network of treatment services and modalities,
designed so that a consumer’s changing needs will be met as that consumer moves through the
treatment and recovery process.
Co-Occurring Disorders are concurrent substance-related and mental health disorders. Use
of the term carries no implication as to which disorder is primary and which secondary, which
disorder occurred first, or whether one disorder caused the other.
Cultural Competency is defined as a set of values, behaviors, attitudes, and practices within
a system, organization, and program or among individuals and which enables them to work
effectively cross culturally. It refers to the ability to honor and respect the beliefs (religious or
otherwise), language, interpersonal styles and behaviors of individuals and families receiving
services, as well as staff who are providing such services. Cultural competence is a dynamic,
ongoing, developmental process that requires a long-term commitment and is achieved over
time.
Discharge Summary is the written summary of the consumer’s treatment episode. The
elements of a discharge summary include description of the treatment received, its duration, a
rating scale of the clinician’s perception of investment by the consumer, a consumer self-rating
score, description of the treatment and non-treatment goals attained while the consumer was in
treatment, and detail those goals not accomplished with a brief statement as to why.
Discharge/Transfer Criteria is when, in the process of treatment, certain problems and
priorities indicate a different level of care, a different provider, or discharge from treatment may
be necessary. The level of functioning and clinical severity of a consumer’s status in each of the
six ASAM dimensions is considered in determining the need for discharge or transfer.
DSM-V refers to the
Diagnostic and Statistical Manual of Mental Disorders (5
th
Edition
),
developed by the American Psychiatric Association (APA). It is the standard classification of
mental health disorders used by mental health professionals in the United States. It is intended
to be used in SUD clinical settings by clinicians for determining behavioral health diagnoses that

10
are part of the assessment and inform development of an individualized treatment plan with the
medically necessary level of care.
Duration refers to the length of time (e.g., three weeks, six months) it is expected that a
service identified in the individual plan of service or treatment plan will be provided.
Early Intervention is a specifically focused treatment program including stage-based
intervention for individuals with substance use disorders as identified through a screening or
assessment process including individuals who may not meet the threshold of abuse or
dependence. (The ASAM Criteria, 3
rd
Edition Level .05 Early Intervention)
Encounter is used for billing purposes related to treatment services, recovery support, and
early intervention services to indicate a measure of time spent providing a service with a
consumer.
Episode of Care is the period of service between the beginning of a treatment service for a
drug or alcohol problem and the termination of services for the prescribed treatment plan. The
first event in this episode is an admission and the last event is a discharge. Any change in
service and/or provider during a treatment episode should be reported as a discharge, with
transfer given as the reason for termination. For reporting purposes, “completion of treatment”
is defined as completion of all planned treatment for the current treatment episode.
Fraud refers to an intentional deception or misrepresentation by a person with the knowledge
the deception could result in unauthorized benefit to him/herself or some other person.
Includes any act that constitutes fraud under applicable Federal or State law.
Grievances are a consumer’s expression of dissatisfaction about service issues, other than an
Adverse Benefit Determination. Possible subjects for grievances include, but are not limited to,
quality of care or services provided, aspects of interpersonal relationships between a service
provider and the consumer, failure to respect the Consumer’s rights regardless of whether
remedial action is requested, or a Consumer’s dispute regarding an extension of time proposed
by the PIHP to make a service authorized decision. 42 CFR 438.400.
Grievance and Appeal System is the processes implemented to handle Appeals of Adverse
Benefit Determinations and Grievances, as well as the processes to collect and track information
about them. 42 CFR 438.400.
Health Care Eligibility/Benefit Inquiry (270) is used to inquire about the health care
eligibility and benefits associated with a subscriber or dependent.
Health Care Eligibility/Benefit Response (271) is used to respond to a request inquiry
about the health care eligibility and benefits associated with a subscriber or dependent.
HMP refers to Healthy Michigan Plan, Michigan’s Medicaid expansion program which became
effective on April 1, 2014, to serve newly enrolled persons. HMP expanded the array of services
available for persons with substance use disorders in need of treatment.

11
Individualized Treatment is treatment designed to meet a particular consumer’s needs,
guided by an individualized treatment plan that is informed by the individual consumer’s
assessment and his/her particular strengths, needs, wishes, and diagnostic areas.
Intensity of Service is the scope, type, and frequency of staff interventions and other
services (such as consultation, referral or support services) provided during treatment at a
particular level of care.
Interim Service(s) are provisional service(s) provided while consumer is waiting for an
appropriate level of care. Please see the specific procedure for priority populations for additional
information.
Length of Service is the number of days (for residential care) or units/visits/encounters (for
outpatient care) of service provided to a consumer, from admission to discharge, at a particular
level of care.
Level of Care, as part of the ASAM, refers to a discrete intensity of clinical and environmental
support services bundled or linked together and available in a variety of settings.
Level of Function is an individual’s relative degree of health and freedom from specific signs
and symptoms of a mental or substance-related disorder, which determine whether the
individual requires treatment.
Level of Service, as part of the ASAM, this term refers to broad categories of patient
placement, which encompass a range of clinical services from early intervention to high-
intensity residential services.
MAPS is the acronym for Michigan’s Automated Prescription System. It is a web-based service
to monitor prescriptions for consumers in Michigan. The website is MAPS.
MDHHS refers to the Michigan Department of Health and Human Services (MDHHS).
Medicaid Health Plans (MHPs) are insurance companies who contract with the State to
provide coverage for the physical health care and mild-moderate behavioral health care benefits
of Medicaid enrollees.
Medicaid Abuse refers to practices that are inconsistent with sound fiscal, business or medical
practices and result in an unnecessary cost to the payor, or in reimbursement for services that
are not medically necessary or fail to meet professionally recognized standards for healthcare.
Medical Necessity means determination that a specific service is medically (clinically)
appropriate and necessary to meet a consumer’s treatment needs, consistent with the
consumer’s diagnosis, symptoms and functional impairments and consistent with clinical
Standards of Care.
Michigan Prevention Data System (MPDS) is the State’s web-based data system that
captures all direct funded prevention services and specific recovery-based services and
community out-reach services.

12
Michigan Mission Based Performance Indicator System (MMBPIS) includes domains for
access to care, adequacy and appropriateness of services provided, efficiency, and outcomes as
required by MDHHS.
Non-urgent cases are those consumers screened for substance use disorder services but who
do not require urgent (immediate) services.
Office Based Opioid Treatment (OBOT) providers offer outpatient treatment that includes
buprenorphine. OBOT providers are usually physician offices/private practice settings.
Opioid Treatment Provider (OTP) providers offer outpatient treatment that includes
methadone.
Peer Support/Recovery Supports are programs designed to support and promote recovery
and prevent relapse through supportive services that result in the knowledge and skills
necessary for an individual’s recovery. Peer Recovery programs are designed and delivered
primarily by individuals in recovery and offer social, emotional, and/or educational supportive
services to help prevent relapse and promote recovery.
Program is a generalized term for an organized system of services designed to address the
treatment needs of consumers.
Readiness to Change refers to an individual’s emotional and cognitive awareness of the need
to change, coupled with a commitment to change. Dimension 4 of the ASAM-PPC, “Readiness
to Change”, describes the individual’s degree of awareness of the relationship between his or
her substance use and/or mental health problems and the adverse consequences, as well as the
presence of specific readiness to change personal patterns.
Recognize, Understand, and Apply is the distinction that the criteria made between an
individual’s ability to
recognize
an addiction problem,
understand
the implications of alcohol and
other drug use on the individual’s life, and
apply
coping and other recovery skills in his/her life
to limit or prevent further alcohol or other drug use. The distinction is in the difference
between an intellectual awareness and more superficial acknowledgement of a problem
(recognition) and a more productive awareness of the ramifications of the problems for one’s
life (understanding); and the ability to achieve behavior change through the integration of
coping and other relapse prevention skills (application).
Recovery means a process of change through which individuals improve their health and
wellness, live self-directed lives, and strive to reach their full potential. SAMHSA states
Recovery is built on access to evidence-based clinical treatment and recovery support services
for all populations.
Reporting Requirements allow the PIHP to collect required reports as identified in provider
contracts. Refer to the contract for a list of report due dates and point of contact. Reporting
requirements are subject to changes based on state and federal requirements.

13
REMI stands for the Regional Electronic Medical Information (REMI) system. REMI is the web-
based managed care information system used by MSHN implemented on February 1, 2018.
REMI replaced CareNet for collection of state and federal data elements, PIHP performance
indicators, utilization management (authorization of services), and reimbursement.
RISC means Recovery and Integrated Services Collaborative, a regional effort to embed
recovery-oriented systems of care (principles and practices) throughout the service provider
network. Collaborative efforts of substance use and mental health providers and comprised of
prevention providers, treatment providers, community members, and individuals in recovery.
ROSC refers to Recovery Oriented System of Care which describes a paradigm shift from an
acute model of treatment to a care model that views SUD as a chronic illness. A ROSC is a
coordinated network of community-based services and supports that is person-centered and
builds over a period of months and/or years on the strengths and resilience of individuals,
families, and communities to achieve abstinence and improved health, wellness, and quality of
life for those with or at risk of alcohol and drug problems.
Root Cause Analysis (RCA) is a process that includes but is not limited to identifying the
causal factors that underlie a significant event that results in (or
could have resulted in
) serious
injury or death, i.e., a Sentinel Event. The root cause analysis focuses primarily on systems and
processes, not individual mistakes or performance. It is a process intended to help understand a
serious and negative situation so as to avoid it in the future.
SAMHSA stands for Substance Abuse and Mental Health Services Administration. It is the
federal agency which oversees the funding to the states for substance use disorder and mental
health services. It is a department within the U. S. Department of Health and Human Services.
SAPT stands for Substance Abuse, Prevention, and Treatment grant sometimes called a “block”
grant. It is the community grant funding from SAMHSA for substance use disorder treatment
and prevention services in the 50 states.
Scope of service is the parameters within which the service will be provided, including Who
(e.g., professional, paraprofessional, aide supervised by a professional); how (e.g., face-to-face,
telephone, taxi or bus, group or individual); and where (e.g., community setting, office,
beneficiary’s home).
Sentinel Event An unexpected occurrence involving death or serious physical or psychological
injury, or the risk thereof. Serious injury specifically includes loss of limb or function. The
phrase or ‘risk thereof’ includes any process variation for which a reoccurrence would carry a
significant chance of serious adverse outcome.
Stages of Change means assessing an individual's readiness to act on new healthier behavior
while providing strategies or processes of change to guide the individual to action and
maintenance. Stages of Change include precontemplation, contemplation, preparation, action,
and maintenance.
State Fair Hearing: Impartial state level review of a Medicaid Consumer’s appeal of an
adverse benefit determination presided over by a MDHHS Administrative Law Judge. Also

14
referred to as "Administrative Hearing". The State Fair Hearing Process is set forth in detail in
Subpart E of 42 CFR Part 431.
Support Services are those readily available to the program through affiliation, contract or
because of their availability to the community at large (for example, 911 emergency response
services). They are used to provide services beyond the capacity of the staff of the program on
a routine basis or to augment the services provided by the staff.
Transfer is the movement of the consumer from one level of service to another or from one
provider to another within the continuum of care.
Treatment is the application of planned procedures to identify and change patterns of
behavior that are maladaptive, destructive and/or injurious to health; or to restore appropriate
levels of physical, psychological and/or social functioning.
Urgent cases are those consumers screened for substance use disorder services (i.e.,
pregnant women) and must be offered treatment within 24 hours.
Waste refers to overutilization of services, or other practices that result in unnecessary costs.
Generally, not considered caused by criminally negligent actions, but rather the misuse of
resources.

15
CUSTOMER SERVICE AND RECIPIENT RIGHTS
Customer Service
Customer Service is a function that operates to enhance the relationship between the consumer
and the provider. This includes orienting new consumers to the services and benefits available
including how to access them, helping consumers with all problems and questions regarding
benefits, handling consumer complaints and grievances in an effective and efficient manner,
and tracking and reporting patterns of problem areas for the organization. This requires a
system that will be available to assist at the time the individual has a need for help and being
able to help on the first contact in most situations. Customer Service is an important aspect of
assuring that persons needing SUD treatment have information about how to access and/or be
assessed for SUD treatment, as well as other relevant community resources to meet potential
consumer and other community representatives or citizens’ informational needs. Customer
Services is responsible to provide support and resources to meet consumer and provider needs,
including but not limited to resource information and referrals. MSHN will assist providers to
meet any special needs of any consumers, including but not limited to those who have hearing
or vision impairments, those who need written or oral interpreter services, those who have
limited English language proficiency, or consumers who need any other special accommodation
to receive needed SUD treatment.
Each provider is expected to designate a staff member to provide Customer Service for the
organization and Customer Service staffing should be sufficient to meet the needs of the
consumers engaged in services. Customer Service staff shall assist consumers with questions,
accessing the local resolution processes, filing grievances and appeals, Medicaid Fair Hearings
information, and coordinating, as appropriate, with the Recipient Rights Advisor. Providers
shall ensure the ways to contact Customer Service via phone and mail are sufficiently displayed
and provided to consumers. Telephone calls to Customer Service shall be answered by a live
voice during business hours, telephone menus are not acceptable. A variety of alternatives
may be employed to triage high volumes of calls as long as each call receives a response within
one business day. The hours which Customer Service operates and the process for accessing
information from Customer Service outside those hours shall be publicized. MSHN Customer
Services is available Monday – Friday, 8:00 am to 5:00 pm to assist consumers and providers
with questions, complaints/grievances assistance, local appeals requests, Medicaid Fair
Hearings information, and SUD Recipient Rights support. Calls should be directed to MSHN
Customer Service at (844) 405-3094.
Customer Service is required to ensure that consumers are offered a Customer Handbook when
they first enter services and the most current handbook version annually thereafter. Providers
are required to complete Adverse Benefit Determination notices and Grievance and Appeals
processes through MSHN’s REMI system. This will also allow providers to maintain records for
appeals and grievances which includes the required information of the name of the person for
whom the appeal or grievance was filed, a general description of the reason for the appeal or
grievance, date received, date of each review, date of resolution, resolution details of the
appeal or grievance. The recordkeeping must be accurately maintained in a manner accessible
to MSHN and available upon request.

16
Recipients Rights for Substance Use Disorder Services
MSHN adheres to the 1978 PA 368, as amended, Administrative Rules for Substance Use
Disorder Programs in Michigan, sections R325.1301 to R325.1399 regarding Recipient Rights.
Consumers have the right to know about the services they are receiving, to make a complaint
about a possible violation to those rights and expect a resolution. The recipient rights process
establishes a method which, if a consumer believes his or her rights have been violated, there is
a known procedure to follow to process the complaint. Each SUD program shall designate one
staff member to function as the program rights advisor by the program director. The rights
advisor shall:
• Complete the required Recipient Rights Advisor trainings.
• Receive and investigate all recipient rights complaints.
• Communicate directly with the MSHN Rights Consultant, when necessary.
The Licensing and Regulatory Affairs (LARA) Rights of Recipients poster must be displayed in a
public place and a copy provided to consumers upon admission. The Recipient Rights poster
should indicate the program’s designated rights advisor’s name and telephone number, along
with the MSHN Regional Rights Consultant’s information
.
Additional brochures, rights
information, and posters are available at the LARA Resources and the MDHHS Resources
websites.
The Regional Rights Consultant for MSHN is:
Dan Dedloff, Customer Service & Rights Manager
Office: 517-657-3011 | Fax: 517-253-7552 | Toll-Free 844-405-3094
Dan.Dedloff@midstatehealthnetwork.org

17
COMPLIANCE
Providers are required to report all suspected fraud and abuse to the MSHN Compliance Officer
prior to completing any investigation or taking any action. The report will be submitted using
the Office of Inspector General Fraud Referral Form which can be downloaded for use from the
MSHN website: Provider Network→Provider Requirements→ Substance Use Disorder→Forms.
Providers will cooperate fully with investigations involving MSHN, the Michigan Department of
Health and Human Services Office of Inspector General and/or the Department of Attorney
General.
Provider staff with firsthand knowledge of activities or omissions that may violate applicable
laws and regulations (not involving suspected fraud or abuse) are required to report such
wrongdoing to the MSHN Compliance Officer or to the Provider Compliance Officer. The
Provider Compliance Officer will review reported violations to determine the need to report to
the MSHN Compliance Officer. The review will be based on but not limited to external party
involvement, Medicaid recipient services, practices and/or system-wide process applicability.
The Provider (CEO)/Executive Director (ED) and/or designee, shall inform, in writing, the MSHN
Chief Executive Officer (CEO) upon learning of any material notice to, inquiry from, or
investigation by any Federal, State, or local human services, fiscal, regulatory, investigatory
(excluding Recipient Rights related to non-PIHP activities), prosecutory, judicial, or law
enforcement agency or protection and/or advocacy organization regarding the rights, safety, or
care of a recipient of Medicaid services. The Provider CEO/ED shall inform, in writing, the
MSHN CEO immediately of any subsequent findings, recommendations, and results of such
notices, inquiries, or investigations.
In addition, providers are expected to communicate any issues regarding non-compliance in a
timely manner so MSHN can assist with developing and/or supporting appropriate responses.
The Compliance Officer for MSHN is:
Kim Zimmerman, Chief Compliance & Quality Officer
Office: 517-657-3018 | Fax: 517-253-7552
kim.zimmerman@midstatehealthnetwork.org
Confidentiality, Privacy & Release of Information
MSHN contracted SUD treatment providers shall comply with the Federal Drug and Alcohol
Confidentiality Law (42 CFR, Part 2) and the Health Insurance Portability and Accountability Act
(HIPAA) of 1996 – Privacy Standards (45 CFR Parts 160 and 164). MSHN requires provider
compliance with all federal and state confidentiality and privacy laws.
42 CFR Part 2 – Federal Drug and Alcohol Confidentiality Law - 42 U.S.C. Section 290dd-3,
290ee-3 for Federal laws and 42 C.F.R. Part 2 for the Code of Federal Regulations is the law
that protects consumer records and status within the context of SUD treatment. Generally, the
program may not acknowledge to anyone outside the program that a consumer attends a
program, or disclose any information identifying a consumer as an alcohol or drug abuser
without a written signed release unless:
• The disclosure is allowed by a special court order; or

18
• The disclosure is made to medical personnel in a medical emergency;
• The disclosure is made to qualified personnel for research, audit, or program evaluation.
Violation of the Federal law and regulations by a program is a crime. Suspected violations may
be reported to the United States Attorney in the district where the violation occurs. SUD
Providers are mandated reporters of suspected child abuse or neglect and thus federal law and
regulations do
not
protect any information about suspected child abuse or neglect from being
reported under state law to appropriate state or local authorities. For additional information, see
here: Mandated Reporting of Abuse/Neglect.
45 CFR Parts 160 and 164 – HIPAA Privacy - In conjunction with the protections under 42
U.S.C. and 42 CFR, all consumers have all their personal health records protected under HIPAA,
45 CFR. The consumer record contains information that under HIPAA is called Protected Health
Information or PHI.
The Privacy Rule defines PHI as individually identifiable health information, held or maintained
by a covered entity or its business associates acting for the covered entity that is transmitted or
maintained in any form or medium (including the individually identifiable health information of
non-U.S. citizens). This includes identifiable demographic and other information relating to the
past, present, or future physical or mental health or condition of an individual, or the provision
or payment of health care to an individual that is created or received by a health care provider,
health plan, employer, or health care clearinghouse.
Some elements that are considered PHI include, but are not limited to: name, address
(including street address, city, county, zip code and equivalent geocodes), name of relatives,
name of employer, all dates (including birth, death, date of service, admission, discharge, etc.),
telephone numbers, fax number, social security number, health plan beneficiary number,
account numbers, certificate/license number, any vehicle or other device serial number, web
Universal Resource Locator (URL), Internet Protocol (IP) address number, finger or voice prints,
and photographic images.
Release of Information- Substance Use Disorder (SUD) Providers are required to obtain
consents to share information regarding alcohol and substance use services and treatment. The
consent form is to be utilized for all electronic and non-electronic Health Information Exchange
environments. Providers are required to utilize, accept and honor the MDHHS standard release
form that was created by MDHHS under Public Act 129 of 2014 (DCH-3927 Consent to Share
Behavioral Health Information for Care Coordination Purposes).
The Privacy Officer for MSHN is:
Kim Zimmerman, Chief Compliance & Quality Officer
Office: 517-657-3018 | Fax: 517-253-7552
kim.zimmerman@midstatehealthnetwork.org
Breach Notification
Mid-State Health Network contracted substance use disorder providers must provide notification
following the discovery of a breach of protected health information in accordance with 45 CFR
164.400-414 (notification in the case of breach of unsecured protected health information).

19
The notification shall be sent to the privacy officer and/or security officer at Mid-State Health
Network immediately following the discovery of a breach of unsecured protected health
information as outlined in the Business Associate’s Agreement and Breach Notification
Procedure.
Steve Grulke, Chief Information Officer, Security Officer
Office: 517-253-7671 | Fax: 517-253-7552
steve.grulke@midstatehealthnetwork.org
Documentation & Records
MSHN adheres to MDHHS’s General Schedule #20 – Community Mental Health Services
Programs’ Record Retention and Disposal Schedule, located at: MDHHS Records Disposal.
All services, such as, assessments, treatment planning, referrals, progress notes, discharge
planning and all other content relative to service delivery must be properly documented
in REMI as well as the provider’s SUD treatment/medical record by properly credentialed
clinicians and linked to an individualized treatment plan. All progress notes must be signed and
any clinicians under a professional development plan must have notes co-signed by a properly
credentialed and authorized supervisor.
All records are subject to audit by MDHHS and/or MSHN, including event verification as required
for federal Medicaid compliance. MSHN and providers could also be subject to federal audit
relative to the use of Medicaid funds. Secure storing of records must meet requirements for
privacy, security and retention, including any electronic records.
Destruction of records needs to follow the policy and retention and disposal schedule listed
above. Disposal must be properly executed with cross-cut shredding or other such proper
disposal under the supervision of an authorized person. Requests for consumer records from
legal contacts or other entities as well as Freedom of Information (FOIA) requests should be
coordinated with MSHN prior to release.
Reporting Requirements & Delinquency Procedure
Mid-State Health Network (MSHN) is required to submit Prevention and Treatment data and
financial reports to the Michigan Department of Health and Human Services (MDHHS) on a
monthly, quarterly and annual basis. MSHN also establishes region-specific deadlines for
operational reports like annual plans and program budgets. MSHN’s ability to meet the
deadlines required by MDHHS and regional deadlines for provider network oversight is
dependent upon all contracted prevention and treatment providers complying with report
submission due dates on a consistent basis.
All data and finance reports and budgets regarding prevention and treatment are due to MSHN
on the designated due dates. Annually, providers will be given the due dates for submission of
all required reports and budgets for the fiscal year. The document entitled, “Reporting
Requirements for MSHN SUD Providers”, is included as an attachment to the MSHN Provider
Contract and includes dates of submission and designated MSHN staff contact person(s) or
locations for submission of each report. Programs are responsible for timely submission of these
reports and budgets on or prior to these due dates.

20
Thirty (30) days prior to the report due date, MSHN staff will send SUD treatment and
prevention providers email reminders with the report title, the due date, and email address for
submission. A follow-up reminder email will be sent seven (7) days prior to the due date as
well. Treatment and prevention providers are expected to submit the required report(s) by the
deadline.
Please refer to the Delinquency Procedure for SUD Providers for details.

21
QUALITY IMPROVEMENT
Mid-State Health Network (MSHN) is responsible for ensuring the responsibilities of the Quality
Management Program are outlined in the Quality Assessment and Performance Improvement
Program (QAPIP) Plan as required by Michigan Department of Health and Human Services. The
QAPIP Plan can be found on the MSHN Website: Stakeholders→Quality & Compliance→Quality
Assessment Performance Improvement Program Plan. The purpose of the MSHN QAPIP is to
establish a system for monitoring, evaluating, and improving quality and safety for those we
serve. The scope of MSHN’s Quality Management Program is inclusive of all CMHSP Participants
and their respective provider networks, and the Substance Use Disorder Providers. Performance
monitoring covers all organizational functions and aspects of care and service delivery systems.
Performance monitoring is accomplished through a combination of well-organized and
documented activities. MSHN delegates to its providers the responsibility for timely access to
treatment, effectiveness of treatment, consumer safety, and consumer feedback, as outlined in
the QAPIP Plan.
Annual Consumer Satisfaction Surveys
MSHN treatment providers shall conduct consumer satisfaction surveys of persons receiving
MSHN funded treatment at least once a year. MSHN will provide the survey tool and compile
the findings and results of the consumer satisfaction surveys for all providers. The regional
findings and results are available to the public and can be found on the MSHN Website:
Consumers→Quality & Compliance→Satisfaction Surveys. Consumers may be active consumers
or having been discharged up to 12 months prior to their participation in the survey. Surveys
may be conducted by mail, telephone, or face-to-face. The information obtained through the
consumer satisfaction survey process should be used to address individual cases of
dissatisfaction, and the development of a Performance Improvement plan which incorporates
the evaluation of the outcomes, utilizing data to make program changes, and identifies how
services are impacted by the program’s goals and objectives.
Michigan Mission Based Performance Indicator System (MMBPIS)
MSHN Treatment Providers are contractually responsible to meet, and document in REMI, the
timeliness standards for Medicaid and Healthy Michigan Plan in accordance with the most
current Michigan Mission-Based Performance Indicator System PIHP Reporting Codebook, in
which there are two (2) timeliness performance indicators as listed below:
• Indicator 2: The percentage of new persons during the quarter receiving a face-to-face
service for treatment or supports within 14 calendar days of a non-emergency request
for service for persons with Substance Use Disorders. (Persons with Substance Use
Disorders). Baseline Data Collection. No Standard.
• Indicator 4b: The percentage of discharges from a sub-acute Detox unit during the
quarter that were seen for follow-up care within 7 days. Standard=95%.
Treatment providers who do not meet the timeliness standard set by MDHHS will be subject to
a quality improvement or performance enhancement plan. The quality improvement plan will
include causal factors or barriers for not meeting the performance standards, and interventions
to improve timeliness of access to treatment. MSHN will use the information obtained to
identify any regional trends that impact access to treatment.

22
Sentinel Events
MSHN Treatment Providers are contractually responsible for reviewing and reporting all critical
incidents as identified by MDHHS and MSHN to determine if a sentinel event has occurred. The
MSHN policies and procedures provide details related to the specific service providers in which
the reporting applies to. The following events should be reviewed to determine if the event
meets the criteria for a sentinel event:
• Death of a recipient
• Accidents requiring emergency room visits and/or admissions to a hospital
• Arrest or conviction of recipients
• Serious challenging behaviors
• Medication errors
• Administration of Narcan
A sentinel event must be identified within 3 business days of the incident occurring. A root
cause analysis must commence within 2 business days of the identification of a sentinel event.
All sentinel events require the completion of a root cause analysis to determine any contributing
factors and determine if actions are required to prevent recurrence of the sentinel event. Critical
Incidents and Sentinel events are to be reported as indicated in the reporting requirements
through the provider portal in REMI.
Deaths that occur as a result of suspected staff action or inaction, subject of a recipient rights,
licensing, or police investigation shall be reported to MSHN within 48 hours of the death. The
report should include the following:
a. Name of individual
b. Individual Medicaid ID
c. Individual PIHP ID if there is no Medicaid ID number
d. Date, time, and place of death (if a licensed foster care facility, include the license
number)
e. Preliminary cause of death
f. Contact person’s name and Email address
Technical assistance may be provided by contacting MSHN’s Quality Manager. Visit the MSHN
website: Provider Network→Provider Requirements→Substance Use Disorder for more
information about reporting requirements.
The Quality Manager for MSHN is:
Sandy Gettel, Quality Manager
Office: 517-220-2422 | Fax: 517-253-7552
Sandy.Gettel@midstatehealthnetwork.org

23
PROVIDER NETWORK MANAGEMENT
Organizational Credentialing and Recredentialing
Substance Use Disorder providers must complete the agency credentialing process in order to
join MSHN's provider panel. Recredentialing must be conducted at least every two years.
Providers seeking to join MSHN's provider panel must demonstrate the following minimum
qualifications:
• License: a current unrestricted, unconditional license to practice substance use disorder
treatment or prevention services in the State of Michigan, issued by LARA;
o NOTE: Governmental entities (i.e., a government, governmental subdivision, or agency,
or public corporation) cannot hold or be required to hold a substance use disorder
license.
MCL 333.6233, MCL 333.1106, MCL 333.1104
• Accreditation (treatment programs only): Current accreditation from a national body
approved by the State of Michigan;
• Certification (if applicable): Current certifications to provide specialized services as
required by the State of Michigan;
• ASAM Level of Care Designation (treatment programs only): Approved by the
State of Michigan;
• Insurance: Current malpractice insurance, cyber security liability and professional
liability insurance in the amount required by MSHN (minimum $1,000,000 per
occurrence and $2,000,000 aggregate);
• Willing to accept all Medicaid/Healthy Michigan consumers residing in MSHN's 21-
county region; and
• Provider staff must meet provider qualifications as defined by the State of
Michigan.
Delegation of Rendering Provider Credentialing and Recredentialing
MSHN requires organizational providers to credential and re-credential, and conduct primary
source verification, and monitor licensure/certification expiration dates of their direct employed
and contracted rendering providers in accordance with the MSHN's credentialing/recredentialing
policies and procedures, which conforms to the
MDHHS credentialing and recredentialing
processes
.
SUD treatment rendering providers must meet qualifications as outlined in the
PIHP/CMHSP
Provider Qualifications Chart
. Upon hire, and upon obtaining new or advanced credentials, the
staff member profile in REMI needs to be added/updated to show current and valid credentials.
Organizational Providers will not be paid for claims where provider qualifications are not met.
Refer to the REMI Help document titled
CPT Codes – NPI, Time, and Modifier Information
for a
complete listing of codes which require specific credentials or NPI. MSHN monitors compliance
with credentialing and recredentialing processes as part of the Quality Assurance and
Performance Improvement site reviews.
SUD treatment and prevention provider staff cannot provide services if they are not certified or
do not have a registered development plan with MCBAP. SUD treatment and prevention
providers may request temporary privileging for staff members who are not certified or have
not registered a development plan with MCBAP but are in the process of obtaining certification
or a registered development plan. If temporary privileging is granted, it shall expire 120 days

24
after the MSHN decision effective date. Master’s level interns will also need to complete a
Temporary Privileging Form. Billing for services of a non-certified (or non-qualified) staff
member will result in financial recoupments and potential contract non-compliance sanctions.
Once the temporary privileging has been approved by MSHN, the provider can add a new user
or new credential to the Staff members profile through the REMI Provider Portal function,
see
REMI Provider Portal page 25 of this document for reference to the Portal
. Once MCBAP
approves the certification or development plan, an update to the staff members profile can be
completed through the Provider Portal in REMI,
see REMI Provider Portal page 25
.
Visit the MSHN website: Provider Requirements→Substance Use Disorder-Provider Credentialing
for more information about credentialing and provider qualifications. Provider qualifications and
supervision requirements are also outlined in the Medicaid Managed Specialty Supports and
Services Program Manual available on the Provider Requirements section of the webpage.
Quality Assurance and Performance Improvement
The Quality Assurance and Performance Improvement team (QAPI) is responsible for
conducting periodic Quality Assurance reviews for activities related to provider performance and
compliance monitoring and ensuring successful monitoring processes are in place as well as
continued monitoring of corrective action plan implementation. Reviews include site and desk
reviews for purposes of evaluating providers in areas of administration and clinical performance
and compliance. MSHN supports reciprocity, and where appropriate, may accept the results of
an audit conducted by another qualified entity. Copies of standards are available on the MSHN
webpage: Provider Requirements→Substance Use Disorder→Quality Assurance and
Performance Improvement.
For more information or to contact the QAPI team email QAPI@midstatehealthnetwork.org.
Capacity
The treatment provider will notify MSHN in the event there are any capacity limitations and/or
any inability to accept new referrals or when planning to increase capacity in residential,
withdrawal management, or recovery residence programs. It is also the provider's responsibility
to notify MSHN of any change in occupancy or service capacity relevant to their MSHN contract
scope of work for SUD services. Providers should also notify MSHN for other changes to
programming/capacity including but not limited to addition of medication assisted treatment,
ability to service new populations, (i.e., men, women, adolescents, adults), etc. MSHN may
elect to seek or add providers to the regional panel to meet existing or new needs of consumers
at any time. All providers are required to submit the monthly Capacity Waitlist Report,
regardless of the status.
Providers may be interested in MSHN’s publication,
Assessment of Network Adequacy
.
Visit the MSHN website: Provider Network→Provider Requirements→Community Mental Health
Service Participants for more information.
Notification of Termination/Closure
If a provider is ending its service contract with MSHN, due to contract termination or provider
closure, the provider must notify MSHN of their intent to close as soon as possible but no less
than 30 days before the contract termination/closure of the program. Also, each provider must

25
make a good faith effort to give written notice of termination, by the later of 30 calendar days
prior to the effective date of the closure, or within 15 days from the provider’s notice to MSHN,
to each consumer who received his or her services from, or was seen on a regular basis by, the
provider. The written notification to each consumer, as coordinated with the responsible MSHN
contact, must contain:
• Date of closure.
• Directions regarding obtaining continued treatment.
• Process for transferring their records to a new provider.
• The need for a signed release of information prior to the transfer of records.
• In the event of provider closure:
o Where their records will be transferred.
o How to obtain information from their records after closure.
The terminating/closing provider will provide MSHN UM Department
(UM@midstatehealthnetwork.org) and MSHN Customer Services
(dan.dedloff@midstatehealthnetwork.org) a list which includes open consumers and consumers
who were recently closed within the past 60 days from the date of the notice of termination or
within 30 days from closure for the purpose of transfer/discharge planning. MSHN will work
closely with the terminating/closing provider through weekly reviews and/or REMI, to assist
each consumer with their transfer to another treatment provider or termination from
treatment. The MSHN Contract Specialist will provide additional instructions to assist the
provider during the termination/closure process.
Providers who offer SUD services must have a mechanism to notify consumers in a reasonable
manner regarding unexpected program or site closure, such as due to inclement weather,
building damage, etc.
Employee Confidentiality
MSHN will protect the confidentiality of the SUD treatment service consumers and their records
as provided by law. Every contracted/sub-contracted program staff member involved in MSHN
funded work is expected to read and abide by the provisions of the MSHN standards of conduct
for confidentiality and privacy.
• Every staff member will sign an employee confidentiality and/or privacy statement at
time of employment;
• A signed copy of the statement will be placed in the staff personnel file;
• A review of the confidentiality policy will be provided annually to the staff; and,
• A new, signed confidentiality/privacy form will be obtained from each staff member
annually.
REMI Provider Portal
Providers are expected to access, monitor, and manage functions via the provider portal. Portal
functions include but are not limited to staff user account setup and management, staff
credentials management, required reporting, and documentation submission. It is highly
recommended that at least two individuals have access to the provider portal. The provider
Portal allows users with the necessary permissions to do the following;
- Add new staff;
- De-activate staff no longer employed;

26
- Reset staff passwords;
- Update staff credentialing records;
- Update agency credentialing records
Agencies are requested to inform MSHN of the two individuals to be assigned the portal
permissions by sending the full names and e-mail addresses to MSHN Contract Manager Kyle
Jaskulka at kyle.jaskulka@midstatehealthnetwork.org.
The REMI “Help” menu contains the Provider Portal User’s Manual as well as a How-to video
describing in more details the functionality of the portal.
The MSHN website also has links to the training materials related to the Provider Portal.
- FAQ
- Presentation
MSHN will no longer process the “REMI User Request” forms previously used to add staff sent
to the inquiries@midstatehealthnetswork.org mailbox.
Training and Continuing Education
MSHN providers are expected to maintain and stay up to date on all trainings required by their
licensure and/or accreditation. All contracted/subcontracted providers are responsible to ensure
that staff members involved in direct service delivery meet and maintain all training and
continuing education requirements as outlined in the MSHN Regional Minimum Training
Requirements. Refer to MSHN Contract for regional training requirements for treatment and
prevention provider staff or the MSHN website: Provider Resources→Provider Trainings for a
complete listing of required trainings and frequency.
Communicable Disease: MSHN adheres to requirements for communicable disease as described
in the OROSC Prevention
Policy #2: Addressing Communicable Disease Issues in the Substance
Abuse Service Network.
All MSHN funded treatment programs must have a procedure in place
for all consumers entering their programs for treatment stating individuals will be appropriately
screened for risk of Tuberculosis, Hepatitis B and C, Sexually Transmitted Infections (STIs and
HIV).
All funded programs will meet state reporting requirements while adhering to federal and state
confidentiality requirements, including 42 CFR Part 2 and Confidentiality of HIV/AIDS
Information. Health education and risk reduction education for at-risk consumers must be
provided at the treatment provider’s site or referred to the local public health

27
department. Follow-up must be monitored and documented in the consumer’s record. TB Tine
Tests may be read by trained staff. Such training is to be documented and readily available for
review.
It is important for all staff working in a substance use disorder program to have at least a
minimum knowledge of communicable disease. Knowledge standards are expected to be
consistent with the roles and responsibilities of program and clinical staff. Minimum standards
are listed in the OROSC Policy under Minimum Knowledge Standards for Substance Abuse
Professionals – Communicable Disease Related.
All trainings required for treatment and prevention providers are available through Improving
Mi Practices, a free training platform. In addition, there are a variety of other trainings that may
benefit your agency and staff. Agencies may create agency accounts and associate staff
members to the agency for easy documentation and tracking of completion of initial training
and annual refreshers. Staff members are able to access their training transcript as well.
MSHN will monitor compliance with MSHN Regional Training Requirement with review of
employee training records during annual quality assurance site review.
Contract Non-Compliance
Providers will be subject to contract compliance actions and corrective action plans from MSHN
when contract requirements are not met or maintained. Contract actions can take many
forms, including but not limited to corrective action plans, voiding of claims/encounters,
repayment of funds, suspension of referrals, monetary or non-monetary sanctions or contract
termination. The selection, nature, extent, duration and other particulars of any initiated
compliance or enforcement actions are at the sole discretion of MSHN. Providers will be offered
opportunity to correct non-compliance wherever reasonable, and sanctions will be issued in
writing, commensurate with the level of non-compliance and in accordance with the Contract
Non-Compliance Procedure.
Please contact Kyle Jaskulka, Contract Manager for questions and feedback related to
amendments and service agreements, credentialing and re-credentialing processes, the network
provider directory, provider communication systems, the provider appeal process, network
expansion, and the site review process.

28
TREATMENT SERVICES
MSHN’s Treatment Specialists are available to assist treatment providers with questions
pertaining to treatment programming. Treatment Specialists can assist with activities such as
new program proposals, program enhancement, development of women’s specialty services
(WSS) designation/enhancement, training needs related to treatment, and community
collaboration efforts. Please contact the treatment specialist assigned to support your agency to
address any needs or concerns or call (517) 253-7525.
Trisha Thrush: trisha.thrush@midstatehealthnetwork.org
Rebecca Emmenecker: rebecca.emmenecker@midstatehealthnetwork.org
Sherrie Donnelly: sherrie.donnelly@midstatehealthnetwork.org
Shannon Myers: shannon.myers@midstatehealthnetwork.org
General Expectations: Providers should refer to the Michigan Medicaid Manual for complete
descriptions of treatment services along with all relevant MDHHS and MSHN policies and
references noted in this manual. Treatment services requirements and expectations are also
outlined in the MDHHS/OROSC policies located here: OROSC policies & advisories. MSHN offers
additional guidance below:
Annual Plans
The MSHN treatment team’s annual planning process is utilized to help support communication
and collaboration among MSHN staff and the provider network, as well as provide discussions
around planning and service development for the SUD treatment providers. Annual plans
provide an opportunity for the SUD provider to share feedback on their experiences and needs
with providing SUD services, as well as to request technical assistance from MSHN, as needed.
The annual planning process also allows the MSHN treatment team to share information with
providers in a one-on-one venue and discuss the SUD providers programs/services in their
communities. Annual plans are completed usually in spring/summer for the subsequent fiscal
year that begins in October.
Auricular Acupuncture
Auricular acupuncture is a commonly practiced technique involving the stimulation of specific
points on the ear. The National Acupuncture Detoxification Association (NADA)-standardized 3-
to 5-point ear acupuncture protocol, has evolved into the most widely implemented acupuncture-
assisted protocol, not only for substance abuse, but also for broad behavioral health applications.
MSHN accepts and promotes the use of auricular acupuncture to assist individuals with substance
use disorders in overcoming cravings, anxiety, sleep disturbances, triggers for use, and other
issues related to recovery from substances.
Biopsychosocial Assessment
General Assessment Guidance: Under the current 1115 Waiver agreement The Michigan
Department of Health and Human Services (MDHHS) requires a standardized assessment for
individuals with substance use disorders. Minimum requirements for a standardized (research-
based, tested and validated) assessment is one that is multi-dimensional, provides a Diagnostic
and Statistical Manual based diagnosis, an ASAM level of care placement output and be
validated for the age of the consumer. MDHHS has approved ASAM Continuum as the sole SUD
biopsychosocial assessment tool for
adults
. The GAIN I Core has been selected as the SUD
biopsychosocial assessment tool for use with
adolescents
. The ASAM Continuum and GAIN I

29
Core became statewide requirements as of October 1, 2021. ASAM Continuum training is
required prior to implementation of the assessment in practice. The GAIN I Core requires
training and certification prior to implementation.
Co-Occurring Mental Health and Substance Use Disorders
Co-Occurring Capable refers to an ASAM category of addiction treatment programs that
accommodate individuals with mental health disorders that are mild to moderate in severity.
These programs address co-occurring disorders (COD) in treatment of individuals. This is
reflected in organizational policies, procedures, assessment, and programming.
• Providers are expected to screen all consumers for co-occurring mental health and
substance use disorders, at the point of access and throughout treatment.
• Provider will provide continuous, comprehensive and individualized services to
consumers with substance use and mental health disorders in a coordinated or
integrated manner.
• MSHN provider programs will demonstrate competency in the provision of services for
those who have co-occurring conditions.
• Acknowledging the high rate of co-occurrence of mental health and SUD symptoms, all
MSHN providers are expected to be co-occurring capable. It is the expectation of MSHN
that all providers will complete the Dual Diagnosis Capability in Addiction Treatment
(DDCAT) self-scoring assessment and provide supporting documentation for each
indicator. Providers will develop and implement DDCAT goals annually and provide
feedback on progress of achieving those goals during the subsequent years annual
planning process. Further information on the DDCAT process may be obtained from the
MSHN Treatment team.
SAMHSA also offers an advisory for Substance Use Disorder Treatment for People with Co-
Occurring Disorders that can be accessed here online as an additional resource.
Cultural Competency
MSHN is committed to supporting all Region 5 residents in achieving health and wellness.
Towards that end, MSHN expects its contracted SUD providers to ensure equitable access to
high quality care for all persons served regardless of race, color, national origin, religion, sex,
gender identity, sexual orientation, disability, age, marital status, income derived from a public
assistance program and/or political beliefs.
MSHN recognizes that cultural competence is a dynamic, ongoing, developmental process that
requires a long-term commitment and is achieved over time. MSHN expects its provider network
members to embrace best practices to support persons served who may be from diverse
cultural backgrounds. Cultural responsiveness includes removing barriers and embracing
differences in order to offer safe and caring environments both for individuals served and for
staff who are members of historically marginalized populations.
SUD prevention/treatment providers should have a cultural competency policy and
documentation of staff training on cultural competency available to MSHN for review.
Service/support/treatment plans and discharge plans must incorporate the natural supports and
strengths specific to the racial and ethnic background of the consumer, family, community,

30
faith-based, and self-help resources. Prevention, education and outreach efforts should include
linkages with racial, ethnic, and cultural organizations throughout the community.
Discharge Planning
MSHN requires that effective discharge planning will be provided for consumers, and that
follow-up services meet contractual and regulatory requirements.
Discharge planning is considered an integral part of SUD treatment. Consideration of the
continuum of care and long-term recovery needs of the consumer will be considered at every
step of treatment planning, beginning at admission. Discharge planning provides improvements
to the quality of care and improves outcomes and controls cost, by assuring coordination and
collaboration with mental health, SUD and other health providers to fully address the needs of
the consumer. It is critical that all providers and organizations serving a consumer act
together to develop an integrated health aftercare plan and then implement this ongoing
aftercare plan in an environment that eliminates barriers and duplication of services.
Discharge Planning will occur according to best practices and the provider organizations’
admission and discharge policies:
• A review of a consumer's discharge plan for all levels of care will be completed to ensure
that appropriate follow-up care is arranged for those ending treatment.
• A written discharge plan will be prepared to ensure continuity of service and will be
distributed to parties involved to carry out the plan. The plan must include the date and
time of appointment(s) and location for the next service provider(s).
• The MSHN contracted provider network will ensure that all consumers are appropriately
discharged from their care, including entering a discharge into REMI and providing an
Adverse Benefit Determination, when appropriate.
• The discharge summary will include the person’s status at the time of discharge, a
summary of services received, and the discharge rationale.
• Aftercare services are incorporated into the treatment plan, and needs are identified and
addressed in the discharge plan.
• Follow up SUD treatment services from a detox and or residential facility will be
completed not more than seven (7) days after discharge.
Documentation Standards
Accurate documentation is necessary to maintain the best care for people served, allows other
staff to pick up services if needed, and verifies the service occurred for audit purposes. At a
minimum documentation:
• must include name of the person served, date of the service, start and stop time of the
service, and be signed, inclusive of credentials, by the staff completing the service;
• identify the service code and modifiers as appropriate
• must be completed timely to ensure it accurately captures the service content;
• must be completed prior to billing for the service provided;
• identifies the treatment plan goal or objective that is being addressed during the
service;

31
• includes session content, interventions used during the session, progress, and the
response to the session;
• contains enough detail to justify the service code that was billed;
• allows a service to be reconstructed for audit purposes;
• meets the credentialing and professional ethics requirements for documentation;
• identifies any evidence-based practices that were used during the session;
• for groups must include the number of people served in the group.
Evidence-Based Practices
MSHN requires all SUD treatment providers to document and provide evidence-based programs
as a part of their services. Evidence-based practices must be documented in the treatment plan
and in session notes when provided. Treatment providers must demonstrate knowledge and
competencies in practice relevant to service provision. Each provider is monitored at least
annually with regular site visits to verify that evidence-based programs are being provided and
that staff and clinicians have the requisite training and qualifications for the practices in which
they are engaging consumers. Evidence-based practices may include motivational interviewing,
trauma-informed care and positive behavioral supports, as well as many others. Recognizing
the stages of change for persons recovering from SUD is an important component of evidence-
based service provision. Providers should take steps to ensure fidelity to evidence-practice
models, including sustaining fidelity when valid models and/or program staffing changes occur,
which may require new training or credentials in maintaining integrity of clinical service
provision. MSHN reserves the right to endorse evidence-based practices in use by funded
provider programs.
Gambling Disorder Protocol
At designated times, during the course of providing treatment, MSHN contracted SUD
Treatment providers will be prompted by the REMI system to administer a gambling disorder
screening, assessment, and referral:
During Admissions process:
1. Administer the three-question GD screen, the NODS-CLiP.
2. Results of the NODS-CLiP screen must be documented and made available to MSHN
in a format to be provided by MSHN.
3. If the screen is positive for GD, PROVIDER will administer the 9-question NODS-SA
assessment. The assessment outcome must be documented and made available to
MSHN in a format to be provided by MSHN with either a “rule out” of GD or a
diagnosis of gambling disorder.
During Treatment Planning process and ongoing during treatment:
1. If there is a GD diagnosis, the provider shall
add a goal to the treatment plan regarding the GD diagnosis.
2. Provider shall make a referral to the Gambling Disorder Helpline.
3. Progress notes following a referral to the Helpline should document ongoing check-
in regarding GD with the consumer to encourage follow-

32
through with the Helpline and to discuss parallels and differences in their addictions
to gambling and to substances.
At Discharge:
1. At discharge, providers need to report the following to MSHN: “If a GD diagnosis was
identified at admission: 1) Was a GD goal added to the TX plan? 2) Was consumer
referred to the GD Help-Line?” 3) If consumer was transferred to a different
provider/LOC, did coordination of care include submission of the treatment plan with
GD goal(s) to the next provider?”
Group Therapy
According to SAMHSA TIP 41,
Substance Abuse Treatment: Group Therapy
, group therapy is
therapeutic for treating substance use disorders and reducing isolation. Groups organized
around therapeutic goals provide insight and guidance, enable individuals to observe others’
recovery and create a culture that supports healing and recovery.
TIP 41 introduces five group models that are used in substance use disorder treatment: psycho-
educational, skills development, cognitive-behavioral, support, and interpersonal process.
1. Psychoeducational groups educate consumers about substance abuse;
2. Skills development groups cultivate skills needed to attain and sustain abstinence;
3. Cognitive-behavioral groups alter thoughts and actions leading to substance abuse;
4. Support groups provide a forum to share pragmatic information about maintaining
abstinence and managing day-to-day, chemical-free life; and
5. Interpersonal process groups delve into major developmental issues that contribute to
addiction or interfere with recovery. TIP 41 reflects that resources, training and
theoretical orientation of group leaders, and the needs and desires of consumers is to be
considered when determining the most appropriate group model. The challenge is
matching the individual to the group model for maximum benefit.
Outpatient Treatment Continuum of Services Treatment Policy #9 defines the minimum in
group therapy as face-to-face interventions with three or more consumers, which includes
therapeutic interventions/counseling. MSHN recommends no more than 12 members to a
therapeutic group and 15 members to an educational and/or didactic group to allow consumers
to feel heard and understood, for the leader to know each of them, and for members to feel a
sense of connection and belonging to the group. The exception to the caps is for 1) skills
development groups where 8-10 members is recommended to allow members to practice new
skills and 2) Cognitive-Behavior groups which should be 3-10 members. Please note, if the
provider is utilizing an evidence-based practice curriculum they will want to follow the guidelines
of the number of participants allowed per group to follow the fidelity of the model.
Therapeutic Yoga: Yoga is not a replacement for a program of addiction recovery, but an
adjunct. The word Yoga means “union,” according to the Hazelden Betty Ford Institute article,
Yoga and Addiction Recovery. By focusing on and controlling breath through yoga, the mind-
body system relaxes and moves toward healing, recovery, and wholeness, which is lost in active
addiction. Yoga helps prevent relapse, reduce withdrawal symptoms and drug cravings, and
provide a healthy outlet to cope with potential triggers and daily life stressors. According to the
Office of Recovery Oriented Systems of Care (OROSC), when yoga is offered as a therapeutic

33
practice and the development of an appropriate coping mechanism to help prevent relapse, this
practice is allowed. The treatment plan is to reflect the therapeutic intervention for every
consumer that participates in therapeutic yoga. The focus of the group is to be comprised
mostly of therapeutic verbal conversation and processing; not just yoga itself. It is preferred
that an instructor with trauma experience or qualifications provides the therapeutic yoga,
however, if one cannot be found, a staff person is able to participate along with the yoga
instructor and talk to consumers about times when yoga may be helpful, used as a coping
mechanism, de-stressing mechanism, sharing the experience with their kids, etc. If therapeutic
yoga is provided in residential treatment, it is bundled into the per diem. If therapeutic yoga is
provided in an outpatient service, it could be coded as 90853 or H0005, depending on the
credentials of the counselor/therapist who is co-facilitating.
Individualized Treatment Planning
Per Treatment Policy #6, there are two key requirements of individualized treatment plans.
First, to be individualized, “treatment and recovery planning requires [the provider’s]
understanding that each consumer is unique, and each plan must be developed based on the
individual needs, goals, desires, and strengths of each consumer.” Second, consumer
participation and engagement in the treatment planning process is critical: “Treatment and
recovery plans must be a product of the consumer’s active involvement and informed
agreement. Direct consumer involvement in establishing the goals and expectations for
treatment is required to ensure appropriate level of care determination, identify true and
realistic needs, and increase the consumer’s motivation to participate in treatment.”
Individualized treatment planning should also utilize S.M.A.R.T. (Specific, Measurable,
Attainable, Reasonable, and Time-bound) goals and objectives, with appropriately identified
amount, scope, and duration for each.
MSHN’s expectation for Treatment Plan timelines are as follows:
Outpatient: Initial treatment plan will be completed by the third (3
rd
) session with the
consumer. Periodic Review of outpatient treatment plans should be within 90 days, but for more
intensive services (e.g., IOP) and/or based on higher intensity consumer needs, more frequent
reviews are required.
Residential/Withdrawal Management: Initial treatment plans are due within three (3) days of
the initiation of treatment services (3 calendar days or 72 hours, not 3 business days). Periodic
review of residential treatment plans should take place every fourteen (14) days minimally for
residential services.
Integrated Coordination of Care
MSHN expects providers will collaborate and coordinate services with other care providers as
appropriate after completing a comprehensive assessment of needs. MSHN also expects SUD
treatment providers to coordinate care with a consumer’s previous and current behavioral
health treatment providers. Coordination of care should include the consumer’s primary care
physician (PCP) and if the consumer does not have one, efforts should be made to link the
consumer to a PCP wherever possible. Providers should maintain documentation of coordination
of care between other behavioral health care providers and physical health care
providers. Documentation must include a signed release of information for the primary care
provider, including name and contact information, or documentation of the client's refusal to
34
provide consent. If the client does not have a primary care provider, there is documentation
that they were offered information and referral to a provider of their choice.
Coordination of care is expected to occur with every consumer and will be comprehensive and
based on the consumer's individual needs. It may include, but is not limited to; legal, dental,
transportation, education, employment, and any other areas of need. This also includes
supporting the individual to the next level of care of services and providing the ASAM
Continuum or GAIN I Core assessment with appropriate release of information to the receiving
provider.
Jail-Based Services
This section applies to providers whose service delivery extends to providing SUD treatment in a
jail setting.
Jail-based SUD treatment can be an important aspect for a consumer’s rehabilitation process
and with that in mind, MSHN will authorize, when available, SUD treatment services to those
who meet eligibility criteria. As of 1-1-2021, MSHN has implemented a Block Grant SUD Benefit
Plan to support the block grant funding reduction from MDHHS. As Jail-Based Services are
funded from the block grant fund source, all programs will want to be versed in the Block Grant
SUD Benefit Plan to support individuals who are incarcerated and receiving services. The Block
Grant SUD Benefit Plan is located on the MSHN website here.
However, providing SUD treatment services within the jail setting has barriers and complications
relating specifically to it being provided in the jail. The provider has no control over consumer
availability and knowledge of the actual release due to the jail’s capacity. With MSHN’s
understanding of the barriers and complications involved, the following guidelines should be
utilized when providing services to incarcerated consumers:
• The SUD treatment provider will assess the consumer when the consumer presents for
services and begin the process of developing a treatment plan for post-jail. Jail-based
services are based on the consumer’s medical necessity for SUD services.
• Each consumer will have an individual assessment, treatment plan, and intake
completed (there will be no "group intakes").
• All consumers receiving services while incarcerated will have a referral made to a SUD
provider in their respective county of residence, with an appointment date and time that
is scheduled close to the next business day following their release date. Since there will
be a possibility of consumers being released early, consumers are to have all the
necessary referral information as soon as possible to be able to schedule an
appointment themselves after early release.
• It is an expectation of MSHN if consumers are released from jail early, every attempt will
be made by the provider of jail-based services to contact the consumers to help ensure
a successful transition to their community SUD treatment provider is made. The
attempts to contact the consumer should be documented in the consumer’s file.
• The provider of jail-based services will secure a release to both the receiving provider
and the consumer's home region, if not MSHN.
• All appointment dates and times will be documented in the REMI system for each
consumer in his/her discharge summary. A note will be made in the discharge note
section of the discharge summary in REMI stating if the consumer was released early.

35
• The provider of jail-based services will ensure that each consumer that receives any jail-
based services will have documentation in REMI for the services.
MDOC Priority Population Technical Requirements
Under an arrangement between the Michigan Department of Corrections (MDOC) and the
Michigan Department of Health and Human Services (MDHHS), MSHN shall be responsible for
medically necessary community-based substance use disorder treatment services for individuals
under the supervision of the Michigan Department of Corrections once those individuals are no
longer incarcerated. These individuals are typically under parole or probation orders and
excludes individuals referred by court and services through local community corrections (PA 5ll)
systems. Through the MSHN FY23 SUD Treatment contract between MSHN and the SUD
Provider Network, MSHN has delegated to providers the responsibility for direct SUD treatment
services.
Referrals, Screening, & Assessment:
Individuals under MDOC supervision are considered a priority population for assessment and
admission for substance use disorder treatment services due to the public safety needs related
to their MDOC involvement. Providers shall ensure timely access to supports and services in
accordance with MDHHS Access Standards.
The MDOC Supervising Agent (SA) will refer individuals in need of substance use disorder
treatment through the following established referral process at MSHN.
For residential referrals only: If an individual has not been receiving any SUD treatment
services and the supervising agent would like to refer the person to residential treatment, the
supervising agent will send CFJ 306 (MDOC referral form) and the MDHHS 5515 (release of
information) to MDOCreferrals@midstatehealthnetwork.org. The Utilization Management (UM)
Department will review the referral documents and make a preliminary referral
recommendation. If residential services are recommended, the consumer will call MSHN UM line
(844-405-3095) and be transferred to an appropriate residential provider.
If an individual is already receiving outpatient SUD treatment services but it is determined they
need residential treatment, the current SUD treatment provider can make the referral directly to
a residential treatment program. MSHN approval is not needed if the referral is being made by
another substance abuse treatment professional. All MDOC residential referrals must originate
from MSHN or from an SUD treatment provider. If an MDOC consumer contacts a residential
treatment provider directly to request services, the residential treatment provider should
contact the MSHN UM Department to ensure that the referral has been approved.
For all other levels of care: Supervising Agents will send the CFJ 306 and the MDHHS 5515
to the receiving provider directly. MSHN UM Department does not need to complete a prior
review/authorization.
Supervising Agents who have not specified a level of care will send those consumers to local
outpatient providers to complete a full biopsychosocial assessment. If the assessment results in
a residential recommendation, the outpatient provider will refer the consumer to the most
appropriate residential program. Residential programs receiving referrals from outpatient

36
providers will accept those referrals as if they are coming from MSHN. Both providers will work
to ensure the full assessment gets transferred to the receiving provider (with appropriate
release).
If the individual is not referred for treatment services, the provider will offer information
regarding community resources such as AA/NA or other support groups to the individual.
Individuals that are subsequently referred through MDOC for substance use disorder treatment
must receive an in-person assessment. The provider may not deny an individual an in-person
assessment via phone screening. In the case of MDOC supervised individuals, assessments
should include consideration of the individual’s presenting symptoms and substance use history
prior to and during incarceration and consideration of their SUD treatment history while
incarcerated. MSHN and/or providers are not required to honor Supervising Agent’s requests or
proscriptions for level or duration of care, services or supports and will base admission and
treatment decisions only on medical necessity criteria and professional assessment factors. The
individual’s individualized master treatment plan shall be developed in a manner consistent with
the principles as defined in the MSHN SUDSP Provider Manual and MDHHS – BSAAS Treatment
Policy #06: Individualized Treatment and Recovery Planning.
Reporting Requirements: Please see the FY23 treatment contract to view full
reporting requirements.
REMI Documentation:
Please see the Help Menu in REMI for additional information on MDOC documentation.
The MSHN point of contact for MDOC related questions is Cammie Myers. Cammie is able to
assist with questions regarding referral, screening, assessment, and training needs. Cammie
can be reached by email at Cammie.Myers@midstatehealthnetwork.org.
Medication Assisted Treatment (MAT)
MSHN adheres to requirements described in all OROSC policies related to MAT. Detail regarding
the state and federal regulations and MSHN’s expectations regarding MAT are in Appendix A of
this manual.
MSHN seeks to ensure that no consumer is denied access to or pressured to reject the full-
service array of evidence-based and potentially life-saving treatment options, including MAT,
that are determined to be medically necessary for the individualized needs of that consumer.
Following the recommendations by SAMHSA, the Centers for Disease Control and Prevention
(CDC), the ASAM, the National Institute for Drug Abuse (NIDA
), MDHHS’s OROSC Treatment
Policies #5 and #6
, and other state and national directives, MSHN requires of its substance use
disorder (SUD) Treatment Provider Network that no MSHN consumer is denied access to or
pressured to reject the full service array of evidence-based and potentially life-saving treatment
options, including Medication Assisted Treatment (MAT), that are determined to be medically
necessary for the individualized needs of that consumer. Per SAMHSA, exclusion of consumers
who are on MAT may be a violation of the Americans with Disabilities Act (ADA) and/or the

37
Rehabilitation Act of 1973. Please reference the SAMHSA brochure Know Your Rights: Rights for
Individuals on Medication-Assisted Treatment.
MSHN-contracted SUD treatment providers are expected to adopt a MAT-inclusive treatment
philosophy in which 1) the provider demonstrates willingness to serve all eligible treatment-
seeking individuals, including those who are using MAT as part of their individual recovery plan
at any stage of treatment or level of care, and without precondition or pressure to adopt an
accelerated tapering schedule and/or a mandated period of abstinence, 2) the provider
develops policies that prohibit disparaging, delegitimizing, and/or stigmatizing of MAT either
with individual consumers or in the public domain.
MSHN adheres to the
MDHHS Medication Assisted Treatment Guidelines for Opioid Use
Disorders.
It is a MSHN expectation that whenever possible, each medication assisted
treatment (MAT) provider offers all medication approved and available for Opioid Use Disorders
(OUD).
Abstinence-Based (AB) Providers: In the interest of consumer choice, MSHN will contract with
Abstinence-Based providers who adhere to written policies and procedures stating the
following:
• If a prospective consumer, at the point of access, expresses his/her preference for an
abstinence-based treatment approach, the access worker will obtain a signed "MSHN
Informed Consent" form (See Appendix D) that attests that the consumer was informed
in an objective and non-judgmental way about other treatment options including MAT,
and attest that the consumer is choosing an abstinence-based provider from an
informed perspective. This includes the consumer’s acknowledgement of receipt of
MSHN’s informational handout/grid titled “Recovery Pathways for Opioid Use Disorder.”
(See Appendix E).
• When a consumer already on MAT (or considering MAT) is seeking treatment services
(counseling, case management, recovery supports, and/or transitional housing) at the
point of access to an AB facility, access staff a) will be accepting and non-judgmental
towards MAT as a choice, b) will not pressure the consumer to make a different choice,
and c) will work with that consumer to do a “warm handoff” to another provider who
can provide those ancillary services while the consumer pursues his or her chosen
recovery pathway that includes MAT.
• Providers’ policies will include language that prohibits delegitimizing, and/or stigmatizing
of MAT (e.g., using either oral or written language that frames MAT as “substituting one
addiction for another”) either verbally with individual consumers, in written materials for
consumers or for public consumption, or in the public domain.
A consensus statement in support of inclusion was endorsed by all ten PIHP’s on November 1,
2017.
Opioid Health Home
According to the Michigan Department of Health and Human Services’ (MDHHS) Opioid Health
Home Handbook, the Opioid Health Home will provide comprehensive care management and
coordination services to Medicaid beneficiaries with an opioid use disorder. Michigan’s OHH
model is comprised of a partnership between a Lead Entity (LE) and Health Home Partners

38
(HHPs) that can best serve the needs of each unique beneficiary. The Lead Entity will be a
regional entity as defined in Michigan’s Mental Health Code (330.1204b).
Health Home Partners will be comprised of two settings – HHP Opioid Treatment Programs
(OTPs) and HHP Office Based Opioid Treatment Providers (OBOTs). The OTP is defined as a
program engaged in opioid treatment of individuals with an opioid agonist medication,
specifically methadone. An OBOT program typically prescribes the partial opioid agonist
buprenorphine and is not licensed to prescribe methadone.
All HHPs must provide Medication for Opioid Use Disorders (MOUD). HHP-OTPs must meet all
state and federal licensing requirements of an OTP. HHP-OBOT providers must attain the proper
federal credentials from the Substance Abuse and Mental Health Services Administration
(SAMHSA) and the Drug Enforcement Agency (DEA) to provide MAT.
Opioid Health Home services will provide integrated, person-centered, and comprehensive care
to eligible beneficiaries to successfully address the complexity of comorbid physical and
behavioral health conditions. Eligible beneficiaries meeting geographic area requirements
include those enrolled in Medicaid, the Healthy Michigan Plan, Freedom to Work, Healthy Kids
Expansion or MIChild who have a diagnosis of opioid use disorder (OUD).
The HHP will employ the following: Behavioral Health Specialist, Nurse Care Manager, Peer
Recovery Coach, Medical Consultant, and a Psychiatric Consultant. In addition to these provider
infrastructure requirements, eligible HHPs should coordinate care with the following professions:
dentist, dietician, nutritionist, pharmacist, peer support specialist, diabetes educator, school
personnel and others as appropriate.
Furthermore, the OHH will provide the following six core health home services as appropriate
for each beneficiary:
1. Comprehensive Care Management
2. Care Coordination
3. Health Promotion
4. Comprehensive Transitional Care
5. Individual and Family Support
6. Referral to Community and Social Support Services
MSHN’s implementation year for FY23 will likely involve some learning and adaptations to the
OHH functions in region 5, and further details will be shared via targeted providers emails,
constant contact, or SUD provider meetings.
Performance Enhancement Plan (PEP)
A MSHN treatment team Performance Enhancement Plan (PEP) is a supportive measure to offer
a provider more intensive technical assistance and monitoring to address quality, performance,
outcomes, and compliance issues. The Performance Enhancement Plan is typically developed

39
and implemented by the MSHN Treatment Team in partnership with the MSHN Utilization
Management Team, QAPI Team, and Quality/Compliance Team. The focus of the PEP is to offer
proscriptive direction to the provider of steps to be taken to address the quality and compliance
issues in concrete and measurable approaches. Utilization of the PEP is considered on an
individualized basis per provider, but could be for any/all of the following:
• Repeat findings and ongoing issues documented in the MSHN QAPI Site Review process
• Repeat and ongoing issues with implementation of quality and compliance standards
• Repeat and ongoing issues with implementing provided technical assistance into practice
• Customer Service or Recipient Rights complaints that warrant further monitoring and
oversight
• The need for increased monitoring and technical assistance to stabilize a program
The timeline of monitoring for a PEP can include a variety of touch points depending on the
individualized needs of the provider and the reasons for the implementation of the PEP. For
occurrences when a need for a PEP is more immediate to address the health and safety needs
of consumers in services, there may be an implementation and review period of monitoring
every 30 days. Other PEPs may warrant time for attention and implementation of technical
assistance or other resources and will be reviewed no more than 90 days out from
implementation or progress review. Performance Enhancement Plans continue to be
implemented and monitored until the items within the plan reach the measurable standards
outlined, and no further needs for assistance have been identified by MSHN or the provider.
Depending on the circumstances which warranted the implementation of the PEP, MSHN can
engage contract non-compliance action as outlined in Section VI.I Contract Remedies and
Sanctions of the FY22 contract and in this provider manual. These steps may include, at the
sole discretion of MSHN, but are not limited to, implementing a full new admission hold or
placing a cap on program admissions, and communication/collaboration with LARA and/or other
accrediting bodies.
Prohibition on Provision of Hypodermic Needles
Providers will assure that no federal or state funds will be used to provide consumers with
hypodermic needles or syringes enabling such consumers to use illegal drugs.
Project ASSERT & SBIRT Programs
For agencies who engage in Project ASSERT (Alcohol & Substance Abuse Services, Education, &
Referral to Treatment) or SBIRT (Screening, Brief Intervention, & Referral to Treatment)
programs in their communities, the provideris required to support data collection and data entry
of encounters into the MSHN REMI system. Providers should utilize the H0002 Brief Screen
code for authorization and reimbursement for the initial face-to-face screening contact they
have with an individual. The H0002 code is an encounter code that is utilized to report peer
recovery coach interactions with individuals when the focus of the encounter is screening, brief
intervention, and referral to treatment services. Following the brief screen, the provider would
need to choose and complete the ASSERT Screening in REMI. The ASSERT Screening consists
of five pages; Basic Information, Substance Use History, Mental Health Symptoms/Medical,
Screening Results/Referrals, and Signatures. If a Brief Screening was completed by the provider
prior to the Project ASSERT Screening, data collected in the Brief Screening will be prefilled. A
narrative guide to support provider submission of data in REMI can be found in the REMI “Help”

40
menu located under the title “Completing Project ASSERT Screening Documents in REMI,” as
well as a short video clip to walk providers through the process.
For providers to utilize the H0002 code, the peer recovery coach supporting Project ASSERT or
SBIRT activities must be appropriately trained according to Medicaid guidelines and be either
CCAR trained or State Certified. Following the initial face-to-face screening encounter, peer
recovery coaches conducting Project ASSERT & SBIRT will continue efforts to follow-up with the
individual over the course of the next 30-90 days. Follow-up phone calls that do not result in a
face-to-face encounter would not be reported in REMI. Utilization of the H0002 code does not
require admissions records or BHTEDS data for submission.
Recovery Oriented Systems of Care
ROSC Participation: MSHN will continue leading the journey of transformational system change
to build a better, more Recovery Oriented Systems of Care (ROSC) in the region. This
system change will be inclusive and a long-term process that will entail changes not only
for providers of services and supports but for all parts of the system including fiscal, policy,
regulatory and administrative strategies. MSHN wants to ensure that this process represents a
broad range of stakeholder viewpoints.
a. Providers will act consistent with collaboration and cooperation of efforts in order
to effect positive change in communities/counties.
b. Providers support a process of community change that engages critical thinking and
collaboration with community partners.
c. Providers support a continuum of improved health and functioning in which there are a
variety of diverse roles for all involved to provide input. These roles include prevention and
treatment PROVIDERS, peer support specialists, community-based support services, and
others.
Therefore, all provider partners shall engage in this process; shall participate and provide
input in the development of Recovery Oriented Systems of Care (ROSC) for the region and at
local/county levels.
MSHN asks that provider partners identify a minimum of one representative to participate
in MSHN-convened ROSC meetings. Participation can be defined as in person, by phone,
videoconference, or connection through email list-serve.
Telemedicine
Telemedicine is the use of telecommunication technology to connect a consumer with a health
care professional in a different location. MDHHS requires a real time (synchronous) interactive
system at both the originating and distant site, allowing instantaneous interaction between the
consumer and health care professional via the telecommunication system. Telemedicine should
be used primarily when travel is prohibitive for the consumer or there is an imminent health risk
justifying immediate medical need for services. MSHN does not support asynchronous (store
and forward) telemedicine practices for this population. Providers must ensure the privacy of
the consumer and the security of any information shared via telemedicine. The technology used
must meet the needs for audio and visual compliance in accordance with current regulations

41
and industry standards. Providers must have a contract with or be authorized by MSHN in
order to provide allowable services via telemedicine. Refer to Section 17 of the Medicaid
Provider Manual for more information on telemedicine. Refer to the PIHP/CMHSP Encounter
Reporting document for a list of allowable telemedicine services codes and modifier
requirements.
Transfer
Transfer is the movement of the consumer from one level-of-care service “to another level of
care, program, provider, or facility.” There is to be follow-up communication between the
provider that is transferring the consumer to another level of care, program, provider, or facility
and the provider receiving the consumer to ensure the consumer timely reaches its referral
destination for admission. Timely admission is defined according to MDHHS requirements. The
provider receiving the consumer is to notify the provider making the transfer referral when the
consumer being transferred is admitted, is a no show, or schedules another admission
appointment. Such notification is to be made as agreed upon between the two programs,
providers, or facilities and to keep within requirements. The transferring provider must ensure
all coordination of care documentation is sent to the provider prior to the first appointment with
a valid release. Coordination of care documentation must include the completed ASAM
Continuum assessment and any relevant clinical documentation on the persons progress and
clinical recommendations to allow the provider to continue care seamlessly.
Trauma Informed Care
A trauma-informed approach to behavioral health care shifts away from the view of “What’s
wrong with this person?” to a more holistic view of “What
happened
to this person?” This
becomes the foundation on which to begin a healing recovery process. Employing a trauma-
informed approach creates a place of safety and mutual respect where a person’s whole history
can be considered. This enables trauma survivors and providers to work together to find the
best avenues for healing and wellness. A program, organization, or system that is trauma-
informed follows SAMHSA’s four “Rs” by:
•
Realizing
the widespread impact of trauma and understands potential paths for
recovery
•
Recognizing
the signs and symptoms of trauma in consumers, families, staff, and others
involved with the system
•
Responding
with fully integrated knowledge about trauma into policies, procedures, and
practices
• Resisting
re-traumatization
Acknowledging the high rate of trauma experienced by consumers served, MSHN providers are
expected to be trauma informed and to provide trauma informed care. It is the expectation of
MSHN that all providers shall complete the Trauma Informed Care Organizational Surveyevery
three years. Providers will develop and implement Trauma Informed goals annually and
provide feedback on progress of achieving those goals during the subsequent years annual
planning process. Further information on the Trauma Informed Organizational Survey may be
obtained from the MSHN Treatment team.

42
Trauma-Specific Services
Prevention, intervention, or treatment services that address traumatic stress as well as any co-
occurring disorders that developed during or after trauma. SAMHSA’s six principles of a trauma-
informed approach and trauma-specific interventions are designed specifically to address the
consequences of trauma and to facilitate healing. These principles include:
•
Safety
—Throughout the organization, staff and consumers should feel physically and
psychologically safe.
•
Trustworthiness and transparency
—Organizational operations and decisions are
conducted with transparency and the goal of building and maintaining trust among staff,
consumers, and family members.
•
Peer support and mutual self-help
—Both are seen as integral to the organizational and
service delivery approach and are understood as key vehicles for building trust,
establishing safety, and empowerment.
•
Collaboration and mutuality
—There is true partnering between staff and consumers and
among organizational staff from direct care staff to administrators.
•
Empowerment, voice, and choice
—Throughout the organization, and among the
consumers served, consumers’ strengths are recognized, built on, and validated, and
new skills developed as necessary.
•
Cultural, historical, and gender issues
—The organization actively moves past cultural
stereotypes and biases, considers language and cultural considerations in providing
support, offers gender-responsive services, leverages the healing value of traditional
cultural and peer connections, and recognizes and addresses historical trauma.
In addition to trauma-informed care, promoting recovery and resilience for those who have
experienced traumatic events involves developing and implementing supports that specifically
consider the event and trauma experienced. It also means examining ways to reduce re-
traumatization. Consistent with SAMHSA’s working definition of recovery, trauma-informed
services and supports build on consumer and family choice, empowerment, and collaboration.
Providers shall develop a trauma-informed system for all ages and across the services spectrum
and shall ensure that the following essential elements are provided:
I. Adoption of trauma informed culture: values, principles and development of a
trauma informed system of care ensuring safety and preventing re-traumatization:
• Providers will ensure that all staff, including direct care staff, are trained/has
ongoing training in trauma informed care.
• Policies and procedures shall ensure a trauma informed system of care is
supported and that the policies address trauma issues, re-traumatization and
secondary trauma of staff.
II. Engagement in organizational self-assessment of trauma informed care
III. Adoption of approaches that prevent and address secondary trauma of staff:
• Providers will adopt approaches that prevent and address secondary traumatic
stress of all staff, including, but not limited to:
i. Opportunity for supervision
ii. Trauma-specific incident debriefing
iii. Training
iv. Self-care

43
v. Other organizational support (e.g., employee assistance program).
IV. Screening for trauma exposure and related symptoms for each population:
• Providers shall use a culturally competent, standardized and validated screening
tool appropriate for each population during the intake process and other points
as clinically appropriate.
V. Trauma-specific assessment for each population:
• Providers shall use a culturally competent, standardized and validated
assessment instrument appropriate for each population. Trauma assessment is
administered based on the outcome of the trauma screening.
VI. Trauma-specific services for each population using evidence-based practice(s)
(EBPs); or evidence informed practice(s) are provided in addition to EBPs:
• Providers shall use evidence-based trauma specific services for each population
in sufficient capacity to meet the need. The services are delivered within a
trauma informed environment.
VII. Providers shall join with other community organizations to support the development
of a trauma informed community that promotes behavioral health and reduces the
likelihood of mental illness and substance use disorders:
• Providers shall join with community organizations, agencies, community
collaboratives (i.e., MPCBs) and community coalitions (i.e., Substance Abuse
Coalitions, Child Abuse and Neglect Councils, Great Start Collaboratives,
neighborhood coalitions, etc.) to support the development of a trauma informed
community that promotes healthy environments for children, adults and their
families.
• Education on recovery and the reduction of stigma are approaches supported in
a trauma informed community.
• Substance abuse prevention programming is provided using a SAMHSA
approved, evidence based and trauma informed approach.
(Medicaid Managed Specialty Supports and Services Program, MDHHS Trauma Policy,)
Veteran Services
Iindividuals who are currently serving or have served in the active military in any branch may
qualify for health care benefits through Veteran’s Affairs (VA). More information about various
types of VA benefits, eligibility requirements, and how to apply can be found on the Veteran’s
Affairs website: va.gov/health-care/
SUD providers shall screen any Veteran/military service member to determine whether the
individual has active VA benefits, other third-party liability coverage (TPL), is covered by
Medicaid or Healthy Michigan Plan (HMP) or has no coverage. Federal regulations require that
all identifiable financial resources and other health insurance plans, including military/veteran
health care benefits, be utilized prior to expenditure of Medicaid funds for most health care
services provided to Medicaid beneficiaries. Medicaid is considered the payer of last resort.
If the Veteran/military service member qualifies for VA health benefits or if they need to apply
for VA health benefits, a warm transfer should be completed to the appropriate VA Medical
Center or Outpatient Clinic. A directory of Michigan VA Centers and Outpatient Clinics can be
found on the Veteran’s Affairs website: Michigan – Locations (va.gov)

44
Access and availability of SUD treatment services through the VA may be limited depending on
the type of service an individual needs and distance from the individual’s home to the nearest
VA provider. In order to close service gaps and enhance access to necessary care,
veterans/military service members may be directly admitted to MSHN-funded SUD treatment
without going through the VA if one of the following exceptions apply:
o The individual requires withdrawal management and/or residential treatment
o The medically necessary level of care or type of service is not available through the
benefits provided by the VA
o There is not a VA provider within 30 minutes/miles in urban areas or 60
minutes/miles in rural areas from the beneficiary’s home
o The individual would have to wait more than 14 days for admission to a VA service
provider.
SUD Providers may call the MSHN Utilization Management (UM) Department at 1-844-405-3095
if they have questions regarding a veteran/military member’s eligibility for MSHN-funded
services.
MSHN also employs a Veteran Navigator whose role is to facilitate access to services for
incoming consumers who currently or in the past served in one of the branches of the U.S.
Military and their families. Upon identification of a person who is serving or has served in the
U.S. Armed Forces, the person should be given contact information of how to reach the Veteran
Navigator:
Tammy Foster, Veterans Navigator
tammy.foster@midstatehealthnetwork.org
517.483.2742
The Veteran Navigator is also available to present Military Cultural Competency trainings to
network providers to help improve access for this population. This training will help providers
to better understand the unique barriers that veterans and military personnel face when
accessing services. Call or email our Veteran Navigator if you would like to schedule a training
for your organization.
Warm Transfer
Warm transfer is a process to ensure a consumer is connected to a live representative at
another location to best provide an answer to the access to treatment requests of the
consumer. It entails allowing the caller to express his/her situation and circumstances to
determine as not urgent or emergent and then warm transferring the call. Emphasis is on
engaging the consumer to create a bond and ensure a safety check. This requires open
communication and teamwork, avoiding communication breakdown.
Once the consumer’s situation is determined to be non-urgent or non-emergent, the
representative receiving the call is to ask the consumer if it is okay to transfer him/her and
explains the reasoning for the transfer. This allows the consumer to understand he/she is not
just being passed off to someone else but builds trust with a positive experience for the
consumer. The representative receiving the call connects the consumer to a live representative
to assist the consumer in explaining what the consumer is seeking. Warm transfer means a

45
consumer encounters no telephone “trees,” and is not put on hold or sent to voicemail until
he/she has spoken to a live representative from the access system.
“For non-emergent calls, a person’s time on-hold awaiting a screening must not exceed three
minutes without being offered an option for callback or talking with a non-professional in the
interim. If the consumers situation is a crisis or emergent, the consumer is immediately
transferred to a qualified practitioner without requiring the consumer to call back.”

46
FINANCE AND CLAIMS
Claims: Please contact the claims department for billing inquiries
to claims@midstatehealthnetwork.org. Please note for billing issues that require action to
services submitted and for submission of Explanation of Benefits documentation, providers
should use REMI.
Finance: For finance matters not related to Claims Processing, please contact:
MSHN’s Chief Financial Officer Leslie.Thomas@midstatehealthnetwork.org
Finance Manager Amy.Keinath@midstatehealthnetwork.org
Financial Specialist Brandilyn.Mason@midstatehealthnetwork.org
This may include items such as budgeting questions, payment frequency, and Financial Status
Report (FSR) submission.
General Business Requirements
Providers are responsible to ensure all provision of services are in compliance with local
municipality and state and federal business requirements, including business records, reporting,
and adherence to all relevant statutes. Providers must be in compliance with all applicable
standards and expectations from the most current
MDHHS Substance Use Disorder Services
(SUDS) Program Audit Guidelines,
which include single audit requirements for providers in
receipt of federal funds greater than $750,000 in a fiscal year.
Medicaid Verification/Reimbursement
The provider, upon admitting a consumer record into the REMI system, is responsible to
determine a consumer’s Medicaid or HMP eligibility. Each month while the consumer is in the
program the provider must verify eligibility and coverage. It is the provider’s responsibility to
verify if there has been a change of coverage if the consumer has third party insurance
coverage, Medicaid, or Healthy Michigan Plan (HMP) eligibility prior to authorization. Since
federal regulations are specific regarding billing for Medicaid, HMP, or Community Grant (Block
Grant), and eligibility requirements change from month to month, active eligibility in Medicaid,
HMP, or other third-party insurance plans must be verified on a monthly basis.
Retrospectively, if it is determined that the consumer was NOT covered by Medicaid during the
service period, the claim may be rejected, and the provider notified. It is then the responsibility
of the provider to notify the Utilization Management Department and follow the established
policy/procedure for obtaining payment under Community Grant (Block Grant).
Providers may be requested to assist consumers or MSHN in submitting evidence of consumer
disability and/or treatment provision or cost in order to obtain and maintain benefit eligibility,
including justification for ongoing Medicaid deductibles.
Healthy Michigan Plan (HMP)
Healthy Michigan Plan (HMP), which became effective April 1, 2014, has served to expand SUD
services to enrolled persons and has also expanded the array of services available for persons
with substance use disorders in need of treatment. MSHN providers will continue to

47
offer defined services under this benefit to support consumers (eligible enrollees/beneficiaries)
with substance use disorders, according to published Medicaid Manual parameters.
Provider Authorizations & Claims
The provider shall electronically submit a claim utilizing REMI to request reimbursement for
authorized services once provided. The provider will submit all the necessary information and
support for all billed services. MSHN is the payer of last resort and the provider must be
knowledgeable and seek other payment options wherever appropriate. Questions about
payment source should be directed to MSHN whenever necessary to ensure funded services are
provided. Claims for unauthorized services will not be paid by MSHN. Any determination of
inappropriate use of funding may result in provider repayment to MSHN. Visit the MSHN
website: Provider Network→Provider Requirements→Substance Use Disorder for more
information about reporting requirements.
Medicaid Recipients with other Primary Insurance
MSHN will authorize Medicaid payment of services only after all other active insurances have
been billed and/or denied. Medicaid recipients who have any other insurance either listed on
the Medicaid Card or indicated through 270/271 information or have coverage through Medicare
Part B must be transferred into a program that has an authorized provider. If Medicare is the
primary insurance for SUD treatment, consumers must be transferred into a program that has
an authorized Medicare provider.
For Medicaid recipients who have a primary insurance other than Medicaid, the primary
insurance must be billed for SUD treatment coverage prior to billing MSHN. Services will not be
authorized or paid by MSHN using Medicaid funding until all other insurance coverage has been
exhausted. Providers can contact Third Party Liability to notify MDHHS of any changes to third
party insurance coverage here: Medicaid Coverage page.

48
Medicare/Third Party Liability (TPL) Primary
For All Levels of Substance Use Disorder (SUD) Care
What if Provider is
not on the third-
party panel?
Beneficiary must go to a Medicare or TPL Provider if the service is a covered benefit in the
individual’s insurance policy.
Note: Healthcare Common Procedure Coding System (HCPCS) procedure codes are non-Medicare
covered services unless provided by a SAMHSA certified Opioid Treatment Program.
Exceptions
• The beneficiary has a primary SUD diagnosis for which SUD-specific treatment services are
needed, meets medical necessity criteria, and the provider provides the necessary American
Society of Addiction Medicine (ASAM) level of care necessary to meet the beneficiary’s
treatment needs.
• For office or site-based services, the location of primary service providers must be within 60
minutes/60 miles in rural areas, and 30 minutes/30 miles in urban areas, from the
beneficiary’s residence (i.e., there are no Medicare SUD-licensed programs or providers
within these distances).
• Must get pre-approval from MSHN Utilization Management (UM) department.
• If MSHN UM Department approves exception for Medicare or TPL covered service, bill Block
Grant only and include supporting notes.
Who do I bill first?
• Must bill covered services to third party insurance first, if paneled with the third-party
insurance.
• Can only bill Medicaid or HMP if a denial with supporting Explanation of Benefits (EOB) is
obtained from the primary insurance first. In cases where it is not possible to obtain a
denial, Medicaid or HMP cannot be billed. The services can only be billed to Block Grant,
provided the consumer meets the income eligibility guidelines for Block Grant and there is
documentation in the consumer chart.
• Note: Medicaid can be billed if the beneficiary has a tribal benefit.
Denied Claims
• If the provider is able to bill Medicare or TPL and obtains the denial with supporting EOB,
then the provider can bill Medicaid or HMP, provided the previously noted guidelines are
met.
• Place EOB in beneficiary’s chart.
• In cases where it is not possible to obtain a denial and supporting EOB for covered services
from Medicare or TPL (i.e. not paneled and/or credentialed), Medicaid or HMP cannot be
billed. The services can only be billed to Block Grant, provided the consumer meets the
income eligibility guidelines for Block Grant and there is documentation in the consumer
chart.
• Note: HCPCS procedure codes are non-Medicare covered services unless provided by a
SAMHSA Opioid Treatment Program. MSHN will pay with Medicaid or HMP, if beneficiary is
eligible.
Partial Payment
• Bill beneficiary’s secondary insurance up to third party insurance’s allowable amount or
MSHN’s contracted rate, whichever is less, (minus first party co-pay for Block Grant funds).
• Place EOB in Beneficiary’s chart.
Deductible
• Bill beneficiary’s secondary insurance up to third party insurance’s allowable amount or MSHN’s
contracted rate, whichever is less, (minus first party co-pay for Block Grant funds).
• Place EOB in Beneficiary’s chart.

49
Reimbursable Diagnoses
Services for consumers with substance use disorders will be provided only for applicable and
appropriate substance use disorder diagnoses as included in the DSM-V (effective October 1,
2015) converted to an ICD-10 code. The SUD diagnosis must be the primary diagnosis for SUD
funds to be used for payment of services provided. SUD diagnoses applicable for
reimbursement are delineated in the REMI system. The appropriate ICD-10 code (not DSM)
shall be selected from the drop-down menu for admissions and discharges. When a consumer
does not have a SUD diagnosis, but requires an assessment or early intervention services,
services can be billed through MSHN. According to the Coding Instructions for Michigan
Behavioral Health Treatment Episode Data Set (BH-TEDS), 999.9997 should be used when no
substance use diagnosis exists OR it has not been determined if a SUD exists based on the
assessment performed. The full BH-TEDS instructions can be found in REMI under
‘Documentation’ on the main menu. It is also acceptable to use the diagnosis code Z03.89 in
instances where use or problems associated with a specific drug is identified, but the individual
does not meet criteria for a full diagnosis.
NOTE: While it is acceptable to use either 999.9997 or Z03.89 as the primary diagnosis for BH-
TEDS admission and discharge records, the diagnosis code 999.9997 is not an allowable billing
diagnosis. For instances when an individual does not have a full substance use diagnosis, but a
billable service was provided, the diagnosis code Z03.89 must be used for billing purposes.
Service Codes & Rates
Fee for service payment rates, by each service code, are included in each SUD treatment
provider’s specific contract as
Provider Fee Schedule Report
. MSHN seeks to have common
regional rates and consistent payment methodologies for providers in the region. MSHN
expects funds to be used in accordance with relevant guidelines and to include supporting
documentation. Rates are based on best value, competitive, and comparable market
information. Unless otherwise referenced directly in the contract with providers with specific
codes, the reference for service codes is the
PIHP/CMHSP Encounter Reporting, HCPCS and
Revenue Codes, Reporting Cost per Code and Code Chart
published by MDHHS, the most
current version, located at: Service & HCPCS Codes.
Specialty Grant Funding
MSHN aims to ensure individuals in our region have consistent access to high-quality, locally-
delivered, evidence-based treatment, prevention, and recovery services. Occasionally, MSHN
pursues additional state and federal grant funding that allow us to support new and expanded
services to the area. Upon notice of grant award(s) by MDHHS, SAMHSA, etc., MSHN
announces opportunities for providers to participate in grant-funded services, supports, and
programs to its provider network to gauge interest. These announcements are made via
Constant Contact, SUD Provider Meetings, and during the annual planning process. MSHN may
also release a Request for Proposals (RFP) to solicit proposals to conduct grant-funded services,
supports, and programs. Providers are also encouraged to submit proposals to the Clinical
Department for review and consideration at any time during the year. Providers receiving grant
funding may be subject to additional requirements, such as monthly reports and conducting
GPRA interviews (for treatment and recovery services only).
State Opioid Response Grant (SOR) & Government Performance and Results Act (GPRA) Core
Client Outcome Measures:

50
The purpose of the Michigan State Opioid Response (SOR-3) grant is to increase access to
medication-assisted treatment (MAT) for the three FDA-approved medications; reduce unmet
treatment need; and reduce opioid overdose-related deaths through the provision of
prevention, treatment and recovery activities for opioid use disorders (OUD). Any client
receiving SOR-funded treatment and/or recovery services is required to complete three (3)
interviews utilizing the Center for Substance Abuse Treatment (CSAT) Government Performance
and Results Act (GPRA) Core Client Outcome Measures for Discretionary Services Programs at
specific time-points:
1. Intake – occurs within 24 hours of receiving first SOR-funded services;
2. Discharge – occurs on last day client received SOR-funded services; and
3. 6-month follow-up – occurs 5-8 months post intake-interview date.
Each provider agency receiving SOR-3 grant funding for treatment and recovery services are
required to maintain a rate of at least 80% completion of the 6-month follow-up (6MFU)
interviews. If the 6MFU interview cannot be completed within the 3-month window, the
provider agency shall submit an “administrative discharge” to close out the client. Note:
administrative discharges count negatively against provider and regional 6MFU interview rates.
Due to concerns regarding the COVID-19 virus, approval has been granted to complete all
GPRA surveying over the phone. This includes intake, discharge and follow up GPRA surveys.
GPRA training, technical assistance, and support is provided by MSHN, MDHHS, and the
evaluation team at Wayne State University to aid in maintaining the minimum 6MFU completion
rates. Additional GPRA resources can be provided by contacting MSHN’s grant coordinator
Heather English at Heather.English@midstatehealthnetwork.org.

51
UTILIZATION MANAGEMENT
The MSHN Utilization Management (UM) team is dedicated to providing prompt, professional,
and helpful support to its treatment provider network. MSHN has established consistent UM
practices based on commonly accepted medical necessity criteria consistent with the Office of
Recovery-Oriented Systems of Care (OROSC) prevention and treatment policies, as well as the
Medicaid Managed Specialty Supports and Services contract, the Michigan Medicaid Manual and
other accepted clinical sources (i.e. the current editions of the DSM and ASAM), which are
designed to benefit eligible consumers across the MSHN region. The MSHN UM team consists
of:
Director of Utilization & Care Management: Skye.Pletcher@midstatehealthnetwork.org
Utilization Management Specialist: Nicole.Jones@midstatehealthnetwork.org
Utilization Management Specialist: Cammie.Myers@midstatehealthnetwork.org
Utilization Management Specialist: Kathrine.Flavin@midstatehealthnetwork.org
The UM team is available Monday – Friday from 8:00 am – 5:00 pm. The UM department toll-
free phone number can be used to reach any available UM specialist, as well as the department
email which is monitored daily:
Toll-Free Phone: 844-405-3095
E-mail: um@midstatehealthnetwork.org
Access to Services
MSHN, in partnership with its SUD Provider network and Community Mental Health Service
Provider (CMHSP) network, maintains a regional “no wrong door” 24/7/365 access system for
SUD services in accordance with the Michigan Department of Health & Human Service (MDHHS)
contracts, MDHHS Access Standards, MDHHS Medicaid Provider Manual, and Michigan Mental
Health Code. Access responsibilities and requirements for SUD Providers are described in the
MSHN Access System Policy and MSHN Access System Procedure.
All MSHN-contracted providers are responsible for maintaining policies, procedures, and
practices that comply with the MSHN Access System Policy and ensure that the experience for
individuals seeking SUD treatment services is efficient, consumer-friendly, timely, and effective.
SUD Providers are required to utilize the Level of Care Screening in REMI at the time of the
initial request for services to document access and referral activities.
Individuals seeking SUD treatment services have the right to choose their preferred treatment
provider from the available options. When a provider performs an access screening with an
individual, they must offer options to the person of different providers of the service(s) and
level of care the person needs. If the person chooses to receive services from a different
provider than the one that is performing the screening, a warm transfer should be completed to
connect the person to the provider of their choice. Individuals should not just be given a list of
phone numbers to call, rather they should be actively assisted until a connection has been
made with an appropriate treatment provider.
Eligibility Determination & Medical Necessity
Eligibility for MSHN-funded SUD treatment services is based on the following:

52
a. The individual is a Medicaid or Healthy Michigan Plan (HMP) beneficiary, OR,
b. If uninsured, the individual meets criteria for SUD Block Grant funding according to
the MSHN SUD Income Eligibility & Fee Determination Procedure
c. Provisional diagnostic impression using the current version of the DSM.
d. Medical necessity and level of care determination criteria utilizing the American
Society of Addiction Medicine (ASAM) Criteria:
i. Dimension 1 – Alcohol Intoxication and/or Withdrawal Potential.
ii. Dimension 2 – Biomedical Conditions and Complications.
iii. Dimension 3 – Emotional, Behavioral, or Cognitive Conditions and
Complications.
iv. Dimension 4 – Readiness to Change.
v. Dimension 5 – Relapse, Continued Use or Continued Problem Potential.
vi. Dimension 6 – Recovery Environment.
In considering the appropriateness of any level of care, the four basic elements of Medical
Necessity should be met:
a. Consumer is experiencing a substance use disorder reflected in a primary, validated,
diagnosis as contained in the most recent versions of the DSM or ICD (not
including V Codes) that is identified as eligible for services in the MSHN Provider
Contract.
b. It is the most appropriate, cost-effective, and least restrictive level of care that can
safely be provided for the consumer’s immediate condition based on the current
edition of The ASAM Patient Placement Criteria.
c. A reasonable expectation that the consumer’s presenting symptoms, condition, or
level of functioning will improve through treatment.
d. The treatment is safe and effective according to nationally accepted standard clinical
evidence generally recognized by substance use disorder or mental health
professionals.
Please Note: Court-ordered treatment is not the same thing as medical necessity. An individual
with a court order for SUD services will still need to participate in a biopsychosocial assessment
to determine their needs and make recommendations for clinically appropriate, medically
necessary services.
Block Grant Funding
A limited amount of Block Grant funding is available each fiscal year for individuals who meet
the established financial eligibility criteria. The purpose of the Block Grant funding is to facilitate
entry into necessary substance use disorder treatment for those persons who are uninsured or
underinsured. Please see the MSHN SUD Income Eligibility & Fee Determination Policy and
MSHN SUD Income Eligibility & Fee Determination Procedure for additional information
regarding consumer eligibility around the use of Block Grant funding and applicable co-pays for
which the consumer is responsible.
MSHN does not limit access to Block Grant-funded SUD programs and services only to the
residents of the MSHN region because Block Grant funding is a federal and statewide resource.
Members of federal and state-identified priority populations must be given access to screening
and to assessment and treatment services, regardless of their residency. However, for non-

53
priority populations, MSHN may give its residents priority in obtaining services when the actual
demand for services by residents eligible for services exceeds the capacity of the agencies.
It is the responsibility of the SUD provider to procure a completed and signed copy of the
Income Verification and Fee Agreement form for all consumers accessing Block Grant funding at
the time of admission to treatment. A signed copy of this form and proof of income are required
to be placed in the consumer record and uploaded into REMI.
All consumers must submit proof of application for Medicaid/Healthy Michigan Plan insurance
benefits within 30 days of admission to treatment under the Block Grant funding source. SUD
providers should place documentation of the submitted application in the consumer file and
upload to the consumer chart in REMI. MSHN will deny authorization for Block Grant-funded
services if consumers do not participate in the requested activities to secure health insurance
benefits within the required timeframe.
Out of Region & Out of Network Services
In keeping with the guiding philosophies of a recovery-oriented system of care (ROSC), Mid-
State Health Network (MSHN) strives to offer a full continuum of treatment and recovery
services and supports through its SUD provider network. MSHN has established contracts with
certain out of region (i.e. outside of the MSHN 21-county area) SUD treatment providers for
residential and/or withdrawal management services to ensure adequate availability of these
services to meet the needs of individuals from the MSHN region. Out of region providers must
comply with the MSHN SUD Services Out of Region Coverage Policy.
When an individual’s recovery needs or preferences include the use of a service provider that is
not part of the MSHN contracted provider network, MSHN has established an SUD Services
Single-Case Agreement Procedure in order to procure, authorize, and pay for medically
necessary services on behalf of the individual. All single-case agreements must be approved by
the MSHN UM department prior to the person being admitted to services by the non-contracted
provider.
Types of Utilization Review
Prospective Utilization Review
Prospective utilization review for SUD treatment and recovery services includes the following
components:
1. Service eligibility determination through an access screening process
2. Verification of medical necessity through a clinical assessment process
3. Use of ASAM Continuum as the standardized assessment and level of care tool for
SUD services and supports
Eligibility determination and verification of medical necessity is delegated to MSHN SUD
Providers. Each SUD provider is responsible for ensuring individual service eligibility and medical
necessity determinations are consistent with MSHN policies and procedures. MSHN will monitor
whether the individual eligibility and medical necessity determinations that have been made are
consistent with MSHN policies during annual quality assessment and performance improvement
(QAPI) site reviews. MSHN UM staff will also review individual consumer records through REMI.
The MSHN UM Committee in conjunction with MSHN UM staff will monitor regional compliance

54
with the access eligibility and medical necessity criteria at the population level through the
review of metrics.
Concurrent Utilization Review
Concurrent utilization review for SUD treatment and recovery services includes the following
components:
1. SUD Providers are responsible for ensuring that each individual receiving services
has an individual plan of service (also called a treatment plan or recovery plan)
which outlines the services to be received.
2. The amount, scope, and duration of each service will be determined by the person
receiving services and their SUD Provider through a person-centered and recovery-
oriented process and documented in the treatment plan/recovery plan
3. The treatment plan/recovery plan for each person will specify the frequency of
review
4. SUD Providers will perform periodic treatment plan/recovery plan reviews and
document the individual’s continued service eligibility and medical necessity for the
services being received
5. MSHN UM Department utilizes service authorization protocols in order to trigger
additional concurrent review of medical necessity for authorization requests which
reflect potential over or under utilization of services.
Retrospective Reviews
Retrospective utilization review for SUD treatment and recovery services includes the following
components:
1. Retrospective review will focus on the cost of care, service utilization, and clinical
profiles
2. Inconsistency with regional service eligibility and/or medical necessity criteria;
and/or
3. Possible over and under-utilization of services when compared to the distribution of
service encounters, associated measures of central tendency (i.e. mean, median,
mode, standard deviation), and consumer clinical profiles (i.e., functional needs)
across the region.
The MSHN UM Department will review claims data and service utilization reports to identify
potentially undesirable variance in service utilization and/or cost of care when compared with
regional average data. MSHN UM staff may perform review of individual consumer records in
REMI to verify that the documentation submitted by the SUD Provider supports the medical
necessity and clinical appropriateness of the services that were provided.
Based upon its findings, the MSHN UM Department will use a variety of interventions at the SUD
Provider level to address any identified concerns. Interventions will vary, depending upon the
nature of the variance and anticipated causal factors, but may include the following:
1. Verify data
2. Request additional information and/or clinical documentation from the SUD Provider
3. Request change strategies from the SUD Provider to bring utilization more in line
with regional averages
4. Provide technical assistance/training to the SUD Provider

55
5. Modify or clarify regional service eligibility and/or medical necessity criteria through
proposed revisions to MSHN policies/procedures
6. Set utilization thresholds or limits
7. Address service configuration to affect utilization
SUD Benefit Plans
MSHN has established SUD Benefit Plans for individuals whose services are funded by Block
Grant as well as individuals whose services are funded by Medicaid/HMP. Both benefit plans are
available in the REMI Help menu and they can also be found on the MSHN Website: Contracts
& Rates
The MSHN SUD Benefit Plans identify the specific HCPCS/CPT service codes which are available
for each ASAM Level of Care as well as the authorization guidelines for each type of service.
When the amount of services requested on an authorization is within the authorization
guidelines identified on the benefit plan, REMI will automatically approve the authorization.
When the amount of services requested exceeds the authorization guidelines identified on the
benefit plan the authorization will be sent to the MSHN UM Department for additional review.
The authorization guidelines identified on the Medicaid/HMP Benefit Plan are based on “typical”
service utilization patterns and are not intended to be a limitation or “cap” on services for
Medicaid/HMP beneficiaries. The MSHN UM Department will review all authorization requests
that exceed the benefit plan guidelines and will approve services that are:
• Clinically appropriate and medically necessary to address the individual’s identified
treatment and recovery needs
• Documented in the individual’s treatment or recovery plan
NOTE: Requests that exceed the Block Grant Benefit Plan guidelines may not be approved
subject to the availability of Block Grant funding during the fiscal year. The MSHN UM
Department will review all authorization requests that exceed the Block Grant benefit plan
guidelines for individuals meeting criteria for SUD priority populations and will approve services
based on medical necessity and funding availability.
Authorizations
SUD Providers must use REMI to request authorization for all treatment services. Authorization
requests will be reviewed and approved or denied on a case-by-case basis utilizing ASAM and
medical necessity criteria. Providers should adhere to the following guidance to ensure the
MSHN UM Department is able to process authorization requests efficiently and make timely
authorization decisions.
Timeliness Standards: While MSHN does not require prior authorization for services, MSHN
strongly recommends timely submission of authorization requests in order to prevent potential
delays or denials to authorization and payment for services already rendered. The following
timeframes are recommended: within 1 business day of admission to withdrawal management
services or within 3 business days of admission to all other levels of care. Re-authorization
requests are recommended to be submitted within 3 business days of the expiration of the
previous authorization.

56
Returned Authorization Requests:
MSHN UM specialists
may return an authorization after
reviewing it in order to request further information or corrections from the SUDSP. In these
instances, the SUDSP should respond as soon as possible. Per Medicaid guidelines, an
authorization decision must be reached within 14 days of the date the authorization request
was submitted. If an authorization decision is not reached within 14 days it constitutes a denial
and MSHN must send an Adverse Benefit Determination (ABD) notice to the person served.
When the MSHN UM Department returns an authorization to a provider requesting additional
information, a timely response is needed from the provider in order to adhere to the required
timeframe and prevent unnecessary denials.
Documentation Standards:
When entering authorization requests, please adhere to the
following clinical documentation standards:
o All areas of the authorization request need to be completed in their entirety to ensure
that the MSHN UM Department has enough information to justify continued treatment.
o Please be sure that authorization date ranges are sequential and do not overlap. If the
current authorization expires on 4/30/2022, please begin the re-authorization request on
5/1/2022. Providers may also choose to early terminate an authorization that is no
longer needed in order to begin a new re-authorization. Please refer to the document
“SUD Treatment Episodes (Admission, Discharge, BH TEDS, Authorizations and
Supporting Documents)” located in the REMI help menu for instructions about early
termination of authorizations.
o An individualized treatment/recovery plan or treatment/recovery plan review document
must be uploaded to the REMI consumer chart accompanying each re-authorization
request. The plan or review must be dated within 90 days of the start date of the
authorization request or the authorization will not process. Treatment/recovery plans
must identify treatment goals and objectives as well as specific progress the consumer
has made toward each goal and objective. Treatment/recovery plans must also identify
any services that are being requested in the authorization.
REMI includes a messaging feature that allows users to send secure messages to one another.
Providers may use this feature to communicate questions, concerns, or other relevant
information to MSHN staff members. The messaging feature within REMI meets all standards
with regard to confidentiality of protected health information. The Utilization Management Team
can be found by composing a new message and clicking the icon with 2 people. This will show
a drop-down menu and Utilization Management is one option. This will send a message to all of
the UM staff.
REMI Admissions, Discharges, Transfers
Admissions: An admission record must be completed in REMI for each individual on the date of
their first face-to-face service with an SUD Provider.
Admission to Multiple SUD Providers: At times it may become necessary for one consumer to be
enrolled in treatment services with more than one SUD Provider at the same time. MSHN has

57
established the following guidelines to prevent duplication of services and facilitate best
consumer care:
o The programs must each be providing different services to the consumer (utilizing
different codes) that are not available at the same provider
o There is clinical justification for medical necessity of all services being provided,
established by an assessment
o There is coordination between all programs involved in the consumer’s care, (with
appropriate consumer release of information), which is documented in the consumer’s
clinical chart as well as in REMI authorization requests.
Transfer Between Providers: If a consumer is transferring from one provider to a different
provider OR if a provider has more than one (1) license and the consumer is changing levels of
care to a different license number, then please complete a discharge summary and choose
“transfer” as the reason for discharge. In the comments section please note which provider or
level of care the consumer is transferring to, and date of first appointment with that provider.
Level of Care Changes Within the Same Provider: If a consumer is transferring from one level of
care to a different level of care within the same provider, and both levels of care have the same
license number, a discharge summary is not required until the consumer has completely
finished the treatment episode and is being discharged from all services.
Discharge Summary: A treatment episode is assumed to have ended at the time the consumer
has not been seen for five (5) days for residential treatment or withdrawal management and
sixty (60) days for all other levels of care. Consumers not seen in these timeframes shall be
discharged from the REMI system. (See State Treatment Episode Data Set (BH-TEDS)
Admission/Discharge Coding Instructions at www.mi.gov/mdhhs). Please note, the discharge
date recorded on the REMI system should be the last date the consumer received a billable
treatment service from the provider.
For Medicaid/Healthy Michigan Plan Consumers: If a consumer has not participated in
scheduled services, please send the required Medicaid Advance Notice of Adverse Benefit
Determination to the consumer and allow them at least 10 days to respond. Once that time
period has passed then proceed to enter the discharge summary within REMI, however on the
discharge form the date of discharge will be recorded as the date the consumer was last seen
for services. That date is still considered the date the consumer effectively disengaged from
services, but they are then given the required 10-day response time to have the opportunity to
re-engage in services. If the consumer re-engages in services within that timeframe, the
discharge does not occur.
The MSHN UM department requires providers to complete a quarterly discharge report to
ensure they are adhering to these established timeliness standards. The Discharge Report and
accompanying instructions can be found on the MSHN website: Provider Reporting
Requirements.

58
Provider Appeal Process
Mid-State Health Network (MSHN) has established a process for providers for the resolution of
appeals of MSHN service authorization denials. This process is for when the provider has
already provided the service, the consumer is no longer receiving services at the agency, the
authorization request was subsequently submitted and reviewed, and was denied by MSHN
Utilization Management (UM). An Adverse Benefit Determination notice shall be mailed to the
consumer and a copy of the letter will also go to the provider explaining the denial of payment
for services. The consumer shall be informed that as a Medicaid or Healthy Michigan Plan
beneficiary, he or she is not liable to pay for the service and the provider may not bill the
consumer for the services. Consumers will be encouraged to contact MSHN Customer Service
should he or she receive a bill from the provider, or for any other concerns or questions
regarding the denial of payment for services process.
Providers are first encouraged to contact a MSHN UM Specialist prior to submitting an appeal to
explore why the service(s) was denied and what may be needed to reconsider the payment for
service(s) before requesting an appeal. If a resolution cannot be reached, then a provider may
file an appeal through the MSHN Customer Service Department regarding the service denial.
Providers must follow the Denial of Payment for Services Appeal Process as outlined below for
an appeal request to be processed.
1. If a resolution cannot be reached than providers have sixty (60) calendar days from the
date of the denial to request an appeal. No appeal will be considered after sixty (60)
calendar days.
2. All appeals must be in writing and include:
a. The date of the appeal
b. The impacted consumer
c. The decision grieved
d. Any provider actions taken to resolve the denial
e. The resolution being requested by the provider
f. The supporting rationale for requesting a change in decision
3. Appeal requests must be submitted to the MSHN Customer Service department
(customerservice@midstatehealthnetwork.org) and copied to the MSHN UM department
(UM@midstatehealthnetwork.org).
4. As appropriate, the MSHN Customer Service Department will include input from the
appropriate MSHN staff and/or departments, including:
a. Chief Financial Officer;
b. Chief Compliance & Quality Officer;
c. Deputy Director;
d. Contract Manager;
e. Utilization Management Specialist;
f. Claims Specialist;
g. Director of Utilization & Care Management;
h. Chief Clinical Officer;
i. Medical Director/Addictionist

59
5. The Customer Service Department will communicate the decision to the provider within
thirty (30) calendar days of the receipt of the appeal.
Please note that this Denial of Payment for Services Appeal Process is separate from Mid-State
Health Network’s (MSHN) established Provider Appeal process for contracted providers which
provides mechanisms to dispute contract concerns, payment performance review findings,
contract monitoring and oversight, or adverse credentialing decisions. Please review the
Provider Appeal Procedure for Substance Use Disorder (SUD) Providers procedure for more
information.

60
PREVENTION PROVIDERS
MSHN’s Prevention Specialists are available to assist with SUD Prevention Provider needs,
including but not limited to county prevention coalitions, prevention initiatives, professional and
other trainings, and the Michigan Prevention Data System (MPDS). Please contact the
prevention specialist in your part of the region whenever possible to address any needs or
concerns or call (517) 253-7525.
Sarah Andreotti: Sarah.Andreotti@midstatehealthnetwork.org
Kari Gulvas: Kari.Gulvas@midstatehealthnetwork.org
Sarah Surna: Sarah.Surna@midstatehealthnetwork.org
Contracted Prevention Providers must adhere to appropriate cultural competency, recipient
rights, confidentiality, and privacy conditions in this manual, as well as any other policies of
MSHN or the State of Michigan applicable to the provision of prevention services. Prevention
contract arrangements funded by MSHN are based on identified local community needs and will
vary from one community to another, including short-term projects, ongoing services, and
collaborations with key community partners. Each contract for prevention services will include
specific detail regarding scope of work, reporting and/or outcomes, as well as financial status
reports (FSR) or claims submission for MSHN reimbursement.
Contracted Prevention Providers must notify and receive written permission to make changes to
their submitted and approved prevention services plan.
Prevention Services
MSHN will elect to contract for appropriate prevention services based on local community
needs.
Prevention Providers are required to verify in writing the use of evidence-based services at the
time of contract initiation and/or renewal. In cases of contract renewal, evidence-based services
will be identified in Contracted Provider’s Annual Plan submission.
MSHN requires that all Contracted Prevention Providers adhere to the following MDHHS
prevention guidelines (subject to revisions by MDHHS):
• All staff being funded in part or whole by MSHN, should read the provider manual at the
time of hire and when updated. Provider agency should have prevention staff sign an
attestation that they have read the manual, which should be kept in the staff personnel
file.
• A Substance Abuse Prevention License is required for any non-governmental entity
offering or purporting to offer prevention services. To meet this requirement, Contracted
Prevention Providers must possess an active Community Change, Alternatives,
Information, and Training (CAIT) License registered with the Michigan Department of
Licensing and Regulatory Affairs (LARA).
• Contracted Prevention Provider Staff must possess an active Certified Prevention
Specialist (CPS) or a Certified Prevention Consultant (CPC) certification through the
Michigan Certification Board for Addiction Professionals (MCBAP). Staff may also be
funded if they have a registered development plan through MCBAP, which is being

61
actively pursued and properly supervised. In some cases, this certification requirement
may be waived if prevention services are delivered by specifically-focused prevention
staff. Specifically-focused staff are those that consistently provide a specific type of
prevention service and do not have responsibilities for implementing a range of
prevention plans, programs, or services. Specifically-focused prevention staff must have
completed formal training for the specific program they are conducting, demonstrable
through certificates of completion or similar documentation.
• For each Contracted Prevention Provider Staff (1.0 FTE), a minimum of 600 hours of
direct prevention services must be conducted annually. Of these 600 hours, a minimum
of 480 hours must be face to face services identified in the MPDS system with the
remaining 120 hours being allowable additional hours submitted on their additional
hours reports. Prior to the beginning of the fiscal year, Contracted Prevention Providers
must submit an annual prevention plan detailing the intended scope of work, evaluation
method(s), responsible staff, and anticipated number of direct service hours.
•
• When entering services in MPDS, please note modality in the group note section when
building the group: f2f, hybrid, or virtual
• All direct prevention activities, funded in part or whole with MSHN funding, must be
captured in MPDS, identifying staff providing service.
• All Contracted Prevention Provider Staff funded by MSHN must complete Level 1
Communicable Disease Training at least once every two years. Free Level 1
Communicable Disease Training is available online at: http://improvingmipractices.org.
For new staff, training should be completed within 90 days of hire.
• Prevention activities must be focused on State and Regional priorities which include 1)
Reduction of Underage Drinking, 2) Reduction of Youth Tobacco Use, 3) Underage
Marijuana Use Prevention and/or 4) Older Adult Prevention Activities, 5) Reduction of
Prescription Drug and Over the Counter Medication misuse and abuse. Services should
focus on and risk and protective factors associated with these problems. Providers may
also address additional priority areas, if local data supports them.
• At a minimum, ninety-five percent (95%) of all services must be research-based.
Contracted Prevention Providers are to follow the guidelines outlined in the Guidance
Document on Evidence-Based Programs developed by the State. The document can be
found on the MDHHS website
(https://www.michigan.gov/documents/mdch/Mich_Guidance_Evidence-
Based_Prvn_SUD_376550_7.pdf ). Identified evidence-based programs, must be
administered with fidelity.
• Services should address both high-risk populations and the general community, unless
approved by MSHN prevention staff.
• No more than twenty-five percent (25%) of total direct services/units can be in the
Federal Strategy of Information Dissemination and services under this category must tie
into your agency’s overall prevention plan. Contracted Prevention Providers must have a
system in place to track total number of services/units delivered in each of the approved
Federal Strategies. Providers will be asked to share their tracking system at the time of
MSHN site visit audit.
• Services need to be based on identified, current community needs.
• Services are collaborative in nature representing coordination of resources and activities
with other primary prevention providers – e.g. local health departments, community

62
collaboratives and the MDHHS’s prevention programs for women, children and families,
and older adults.
• Services need to be supportive of local coalitions. New providers interested in providing
prevention services should be a regular participant in county prevention coalition
meetings and have documented discussions during those meetings in order to be
considered for funding.
• Services must fall within one of the six federally defined strategies: information
dissemination, education, problem identification and referral, alternatives, community
based, or environmental.
• Services must be provided in a culturally competent manner. Contracted Prevention
Providers must have a cultural competency policy and staff must attend at least one
cultural competency training annually.
• All media promoting programs funded all or in part by MSHN must acknowledge the
funding source by using text or a logo provided by MSHN.
• If Provider is planning on conducting a local Media Campaign, all materials must be
approved by MSHN and/or MDHHS.
Coordination of Services
All Contracted Prevention Providers must be able to identify at their site visit how services are
coordinated with other community agencies and coalitions. Coordination of services should
minimally include:
• Local Department of Health and Human Services
• Local Community Mental Health Service Provider
• Local Schools
• Law Enforcement
• School Resource Officers (where applicable)
• Teen Health Centers (where applicable)
• Community Coalitions
• Local Health Departments
• Federally Qualified Health Centers (where applicable)
Whenever possible, Contracted Prevention Providers are encouraged to enter into referral
agreements with community agencies. MSHN will offer or support technical assistance for this
upon request.
Program Evaluation
Providers should be aware of and attempt whenever possible to collect data elements identified
in the National Outcome Measures (NOMs), such as: 30-day use, perception of risk/harm of
use, age of first use, perception of disapproval/attitudes, perception of workplace policy,
average daily school attendance rate, number of persons served by age, gender, race, and
ethnicity, family communication around drug and alcohol use, number of evidence-based
programs (EBPs) and strategies used, percentage of youth seeing, reading, watching, or
listening to a prevention message, alcohol-related traffic fatalities, and alcohol- and drug-
related arrests. Visit SAMHSA for more information related to NOMs.

63
Providers are expected to provide MSHN an outcome report after the end of the fiscal year.
This report should identify how activities were evaluated, outcome of those evaluations, and
how the evaluations were utilized to improve programming.
MSHN requires that all prevention services incorporate some method of evaluation. Contracted
Prevention Providers must include all process evaluation data as outlined in Michigan Licensing
rules. In addition, Providers need to incorporate the following processes: Completion of Short-
term Outcome Evaluation identifying knowledge, attitude and behavior changes. For all
programming, outside of information dissemination, providers must be able to demonstrate
program effectiveness, i.e., what were the goals of the program and were those goals
obtained? Development of a Performance Improvement Plan, which incorporates evaluation
outcomes, utilizing data to make program changes, and identifying how services impacted
program goals and objectives. Provider should also collect satisfaction surveys of prevention
programming.
Contracted Prevention Providers need to have an agency/department Performance
Improvement Policy and must demonstrate how prevention services are incorporated into the
plan.
Charging for Prevention Services
If a Contracted Prevention Provider charges a fee for prevention activities, funded in whole or
part by MSHN, the provider must adhere to the following guidelines:
• Providers must have a policy in place that is specific to charging for prevention services,
• This policy must ensure that services will not be denied based on ability to pay,
• A copy of this policy must be submitted to MSHN prior to the beginning of the contract
period, and revised annually,
• Any prevention activities that require payment to participate must have a brochure/flyer
that clearly states that scholarships are available; these materials should be used
whenever promoting the activity, and
• Providers must identify fees collected for prevention activities on the monthly FSRs
under Provider Sources of Funds > Fees & Collections.
Prevention Activity Reporting
To capture activity data, all direct services, funded in whole or part by MSHN, must be
accurately entered into the Michigan Prevention Data System (MPDS) as outlined in the MPDS
User Manual. Provider staff are responsible for reading the MPDS User Manual upon hire and
periodically and must have a process in place to monitor the accuracy of activity data entered.
Provider Agency must maintain documentation in the employee file that acknowledges receipt
and understanding of the prevention MPDS user manual. This process will be reviewed during
the site visit.
Activity data must be entered into the MPDS on a monthly basis. Failure to enter activity data
by the 10
th
of the month following the date of service may result in delayed payment by MSHN.
MSHN Prevention Specialists are available to provide MPDS- related technical assistance and
training to Contracted Prevention Providers upon request. Please consult the MPDS User Manual
prior to contacting your MSHN Prevention Specialist for assistance.

64
Twice a year, prevention and community recovery providers are required to submit a MPDS
Direct Service Hours Report to their assigned MSHN Prevention Specialist. This is an
opportunity for the prevention or community recovery provider supervisor to review and
comment on the status of meeting prevention direct service hour requirements; any adaptations
to programming as a result of review of the units; timeliness of staff data entry; etc. for each
prevention or community recovery staff in the organization. Reports should be run from the
Activity Data Report in MPDS and include the six fields of Group Name, Activity Start Date,
Activity Creation date, Units, Activity Record Number, and Staff. In the email with the report,
program supervisors should summarize activity units into hours per staff person; identifying if
they are on track to meet direct service hour requirements for each individual staff member,
and how the organization plans to address under unit/hour adjustments if they are not on track
to meet requirements. Reports are due to be submitted by the program supervisor to their
agency’s MSHN Prevention Specialist by January 15 for services from 10/1/22-12/31/22 and
submitted by July 15 for services from 1/1/23-6/30/23.
Designated Youth Tobacco Use Representatives (DYTURs)
The federal Synar Amendment requires states to have laws in place prohibiting the sale and
distribution of tobacco products to persons under 21 years-of-age and to enforce those laws
effectively. Annual Synar checks, required by the amendment, show that great strides have
been made the reduction in retailer violations of the law and youth access to tobacco products
in Michigan.
To ensure that the region complies with the expectations set forth by the state, MSHN will
contract with one provider in each of its 21 counties to deliver services through Designated
Youth Tobacco Use Representatives (DYTURs). Providers contracted for DYTUR services will be
responsible for:
• Maintaining and updating the master tobacco retailer list (MRL) at least annually for
each represented county, which minimally includes visiting or calling each retailer to
verify/update contact information;
• By May 15th of each year, providing face-to-face vendor education and non-Synar to at
least 50% of the tobacco retailers in the DYTUR’s designated county(ies) utilizing the
official MDHHS protocol . Providers have a choice to conduct 100% vendor education
(via phone and/or mail) in lieu of non-Synar compliance checks; and
• Annually conducting and completing the Formal Synar compliance checks to all retailers
in the sample draw during the designated time period, taking care to utilize the official
MDHHS protocol . MSHN Prevention Staff will meet with DYTUR providers on securing
proper youth employment requirements.
In addition, DYTURs are expected to:
• Actively engage in county-level tobacco prevention/reduction coalitions or other
substance use disorder prevention coalitions if no tobacco-related coalition is in place;
• Provide education to local law enforcement, chambers of commerce, and other
community groups on the Synar Amendment;

65
• Maintain records of all tobacco compliance checks being completed within their
designated county(ies), including compliance checks conducted outside of MSHN’s
purview;
• Complete the Youth Access to Tobacco Activity Report annually. Appropriate technical
assistance, training, and protocol forms will be provided by MSHN’s prevention
specialists; and
• Attend state-level DYTUR/Youth Tobacco Act (YTA) meetings when possible. If/when
DYTUR staff are not able to attend, please contact your MSHN Prevention Specialists in
advance for call-in information, agendas, minutes, etc.
DYTUR Reporting
Providers contracted for DYTUR services are expected to submit the following annual reports to
MSHN by the due dates provided in separate documentation:
• Revised Master Tobacco Retailer List (MRL)—Please remember, all tobacco
retailers on the MRL must be verified by a phone call or personal visit. Verification must
include the retailer name, address (including county), vendor type, and phone number.
DYTURs are expected to identify retailers selling ENDS (e.g., e-cigs, vape pens, hookah
pens, etc.) in their establishments during the MRL revision process. DYTURs must also
add any known new retailers to the MRL;
• Vendor Education and non-Synar Reports—IMPORTANT: A minimum of 50%
vendor education and non-Synar must be completed prior to the start of the Formal
Synar period. Providers have the choice to conduct 100% vendor education (via phone
and/or mail) in lieu of non-Synar compliance checks.
• Formal Synar Compliance Check Forms; and
• Youth Access to Tobacco Activity Report
In addition, all providers contracted for DYTUR services are expected to enter Youth Tobacco
Act (YTA) activities into the MPDS by the 10
th
of the month following the date of service. These
activities should minimally include vendor education, non-Synar compliance checks, and Formal
Synar compliance checks. To ensure standardization of regional data, DYTURs will be provided
with a data entry guide for YTA-related activities and are expected to input data accurately
according to the instructions given.
DYTUR reporting forms and due dates will be provided by MSHN. Providers are responsible for
reviewing all reporting forms for completeness and accuracy prior to sending to MSHN.
* SAPT Block Grant funds cannot be used for law enforcement compliance checks, including
Formal Synar and non-Synar activities, or tobacco cessation programs.
Early Intervention-Prevention
MSHN adheres to the recommendations described by OROSC in
Treatment Technical Advisory
#9: Early Intervention
. This section will focus on prevention’s role in Early Intervention services.
Prevention Early Intervention (PIR) services typically exist within the community being served
(e.g. schools, community centers, etc.). “Prevention” refers to this level of service under the
federal strategy of Problem Identification and Referral (PIR), and defines it as “helping a person

66
with an acute personal problem involving or related to SUDs, to reduce the risk that the person
might be required to enter the SUDs treatment system” (U.S. CFR, 1996).
PIR aims to identify those who have indulged in the illegal use of drugs in order to assess if
their behavior can be reversed through education. PIR does not include any activity designed to
determine if an individual is in need of treatment. Examples of PIR include driving while
intoxicated education programs, employee assistance programs (EAPs), and student assistance
programs (SAPs) (FY 2012-14 Action Plan Guidance).
PIR service activities are not required to occur in the context of an existing licensed SUD
treatment program; however, providers of Prevention Early Intervention (PIR) services must
have appropriate prevention licensure (CAIT).
PIR services must be delivered by individuals credentialed as a Certified Prevention Specialist
(CPS) or Certified Prevention Consultant (CPC) with appropriate documentation submitted to
and approved by the Michigan Certification Board for Addiction Professionals (MCBAP).
Supervision of PIR programs must be provided by a MCBAP-approved CPS/CPC or a MCBAP-
approved alternative.
Community Coalitions
MSHN strongly believes in the power of community coalitions. MSHN believes that Prevention
Coalitions belong to their communities. As such, MSHN does not fund community coalitions, but
rather supports them in the following ways:
1. MSHN Prevention Staff will provide guidance if requested and attend, whenever
possible, local coalition meetings.
2. MSHN will support a contracted prevention staff member to assist coalition in a part time
coordinator role.
3. MSHN will provide a stipend to each of the 21 county’s coalition to be utilized as deemed
appropriate by the coalition members. Process for this funding includes:
a. Funding will be given yearly to one MSHN contracted provider in each county for
the purpose of acting as the fiduciary for this funding.
b. In order for funding to be utilized, coalition members must discuss, approve and
vote on funding decisions.
c. Coalition voting must be identified in coalition meeting minutes.
d. Provider acting as fiduciary for this funding should provide coalition members
regular budget summary.

67
SELECTED REFERENCES
1. Carroll, K. (Ed.). (2000).
Approaches to Drug Abuse Counseling
. National Institute on Drug
Abuse. Rockville, MD. [On-line].
Available: http://archives.drugabuse.gov/pdf/ADAC/ApproachestoDACounseling.pdf.
2. Center for Substance Abuse Treatment. (2004).
Clinical Guidelines for the Use of
Buprenorphine in the Treatment of Opioid Addiction. Treatment Improvement Protocol (TIP)
Series 40.
Substance Abuse and Mental Health Services Administration. Rockville, MD. [On-
line]. Available: http://buprenorphine.samhsa.gov/Bup_Guidelines.pdf.
3. Center for Substance Abuse Treatment. (2005).
Medication-Assisted Treatment for Opioid
Addiction in Opioid Treatment Programs. Treatment Improvement Protocol (TIP) Series
43.
Substance Abuse and Mental Health Services Administration. Rockville, MD. [On-line].
Available: http://adaiclearinghouse.org/downloads/TIP-43-Medication-Assisted-Treatment-
for-Opioid-Addiction-in-Opioid-Treatment-Programs-51.pdf.
4. Center for Substance Abuse Treatment. (2005).
Substance Abuse Treatment for Persons
with Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series 42.
Substance
Abuse and Mental Health Services Administration. Rockville, MD. [On-line].
Available: http://www.breining.edu/TIP42CoOccDis.pdf.
5. Center for Substance Abuse Treatment. (2009).
Clinical Supervision and Professional
Development of the Substance Abuse Counselor
.
Treatment Improvement Protocol (TIP)
Series 52.
Substance Abuse and Mental Health Services Administration. Rockville, MD. [On-
line]. Available: http://www.readytotest.com/PDFs/TIP52.pdf.
6. Center for Substance Abuse Treatment. (2009).
Substance Abuse Treatment: Addressing
the Specific Needs of Women. Treatment Improvement Protocol (TIP) Series 51.
Substance
Abuse and Mental Health Services Administration. Rockville, MD. [On-line].
Available: http://adaiclearinghouse.org/downloads/TIP-51-Substance-Abuse-Treatment-
Addressing-the-Specific-Needs-of-Women-42.pdf.
7. Mee-Lee, D. (Ed.). (2013).
The ASAM Criteria: Treatment Criteria for Addictive, Substance-
Related, and Co-Occurring Conditions.
American Society of Addiction Medicine. Chevy
Chase, MD.
8. Morris, J, Day, S., Schoenwald, S. (2010)
Turning Knowledge into Practice: A Manual For
Behavioral Health Administrators & Practitioners About Understanding & Implementing
Evidence-Based Practices, 2nd Edition.
The Technical Assistance Collaborative, Inc. Boston
MA. [On-line].
Available: http://www.tacinc.org/media/13067/Turning%20Knowledge%20into%20Practice.
pdf.
9. Munetz, M., Griffin, P. (2006). Use of the Sequential Intercept Model as an Approach to
Decriminalization of People with Serious Mental Illness.
Psychiatric Services 57:
544-549.
[On-line]. Available: http://publicdefender.mt.gov/training/Session3.pdf.
10. Rollnick, S., Miller, W. R. (2013).
Motivational Interviewing: Helping People Change. Third
Edition.
The Guilford Press. New York, NY.
11. The Iowa Practice Improvement Collaborative Project. (2003).
Evidence-Based Practices: An
Implementation Guide for Community-Based Substance Abuse Treatment Agencies.
The
Iowa Consortium for Substance Abuse Research and Evaluation. Iowa City, IA. [On-line].
Available: http://iconsortium.substabuse.uiowa.edu/EBP%20Guide.pdf.
12. Substance Abuse and Mental Health Services Administration. (2009).
Integrated Treatment
for Co-Occurring Disorders Evidence-Based Practices (EBP) KIT.
Center for Mental Health
Services, Substance Abuse and Mental Health Services Administration, U.S. Department of

68
Health and Human Services. Rockville, MD. [On-line].
Available: http://store.samhsa.gov/product/Integrated-Treatment-for-Co-Occurring-
Disorders-Evidence-Based-Practices-EBP-KIT/SMA08-4367.
13. Institute for Social Research. (2011).
Jail Based Substance Abuse Treatment Literature
Review.
Institute for Social Research, University of New Mexico. Albuquerque, NM. [On-
line]. Available: http://isr.unm.edu/reports/2011/jail-based-substance-abuse-treatment-
literature-review..pdf.
14. Mann, C., Frieden, T., Hyde, P., Volkow, N., Koob, G. (2014).
Medication Assisted Treatment
for Substance Use Disorders
. Informational Bulletin. [On-line].
Available: http://medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-07-11-2014.pdf.
15. Substance Abuse and Mental Health Services Administration. (2011).
Dual Diagnosis
Capability in Mental Health Treatment Toolkit Version 4.0
. Substance Abuse and Mental
Health Services Administration. Rockville, MD. [On-line].
Available: http://ahsr.dartmouth.edu/docs/DDCMHT_Toolkit.pdf.
16. Substance Abuse and Mental Health Services Administration. (2012).
General Principles for
the Use of Pharmacological Agents to Treat Individuals with Co-Occurring Mental and
Substance Use Disorders.
Substance Abuse and Mental Health Services Administration.
Rockville, MD. [On-line].
Available: http://www.ncdsv.org/images/SAMHSA_GeneralPrinciplesUsePharmacologicalAge
ntsTreatIndividualsCo-OccuringMentalSubstanceUseDisorders_2012.pdf.
17. Substance Abuse and Mental Health Services Administration. (2013).
Systems-Level
Implementation of Screening, Brief Intervention, and Referral to Treatment
.
Technical
Assistance Publication (TAP) Series 33.
Substance Abuse and Mental Health Services
Administration. Rockville, MD. [On-line].
Available: http://store.samhsa.gov/shin/content//SMA13-4741/TAP33.pdf.
18. Substance Abuse and Mental Health Services Administration. (2014).
Improving Cultural
Competence. Treatment Improvement Protocol (TIP) Series No. 59.
Substance Abuse and
Mental Health Services Administration. Rockville, MD. [On-line].
Available: http://store.samhsa.gov/shin/content/SMA14-4849/SMA14-4849.pdf
19. Substance Abuse and Mental Health Services Administration. (2016).
SAMHSA's Efforts to
Address Trauma and Violence
. Substance Abuse and Mental Health Services Administration.
Rockville, MD. [On-line]. Available: http://www.samhsa.gov/topics/trauma-
violence/samhsas-trauma-informed-approach
20. Tsemberis, S., Gulcur, L., Nakae, M. (2004). Housing First, Consumer Choice, and Harm
Reduction for Homeless Individuals with a Dual Diagnosis.
American Journal of Public Health
4:
651-656. [On-line].
Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1448313/pdf/0940651.pdf.

69
Appendix A: MSHN MAT Protocol
INSTRUCTIONS AND PROTOCOLS FOR THE IMPLEMENTATION OF
MEDICATION-ASSISTED TREATMENT (MAT)
Note: This document establishes technical and service requirements that providers are
contractually obligated to incorporate into the design and delivery of all medication-assisted
treatment (MAT) services funded through Mid-State Health Network (MSHN). MAT service
providers are required to adopt these protocols in their entirety, as well as incorporate the
requirements of the Michigan Department of Health and Human Services, Behavioral Health and
Development Disabilities Administration’s (MDHHS-BHDDA) policies and advisories, and the
Michigan Medicaid Provider Manual.
This document was written and reviewed by MSHN Clinical and Utilization Management staff as
well as reviewed by MSHN’s SUD Medical Director, Dr. Bruce Springer and the MSHN MAT
workgroup. While a primary focus is MAT for Opioid Use Disorder (OUD), additional sections
address MAT’s applications to other addictive disorders as well. Should you have any questions,
please contact MSHN at 517-253-7525
Introduction:
Medication Assisted Treatment, broadly refers to the use of medication in treating addiction to
a variety of substances: opioids (prescription analgesics and heroin), alcohol, cocaine,
benzodiazepines, and marijuana. Consistent with Medicaid rules, MSHN’s policy is that
consumers should have a full-service array of treatment options available
. This should include
MAT for all persons who have been determined medically and clinically eligible for MAT. Since
not all individuals are appropriate for MAT (even when they may meet clinical criteria), MSHN
expects providers to assess and stage every consumer to determine the consumer’s readiness
for change as a means of ensuring that the provision of MAT services will best meet the
individual needs of the consumer. MAT providers must inform consumers of daily attendance
requirements, mandatory counseling requirements, toxicology testing requirements and other
program participation requirements outlined in this protocol document both at admission and
throughout the course of treatment as applicable.
Reviews to determine continued eligibility for methadone dosing and counseling services must
occur at least every four months by the opioid treatment provider (OTP) physician during the
first two years of service. This documentation should be included in the authorization request
sent to MSHN as well as in the consumer’s record. An assessment of the ability to pay for
services and a determination for Medicaid coverage must be conducted monthly.
MEDICATION-ASSISTED TREATMENT & OPIOID USE DISORDER
Medication Assisted Treatment may be provided at a licensed and state-regulated OTP
(methadone, buprenorphine, naltrexone) or in a physician's office or other healthcare setting
(buprenorphine and naltrexone only). Comprehensive maintenance, medical maintenance,

70
interim maintenance, detoxification, and medically supervised withdrawal are types of MAT
services.
• Comprehensive Maintenance Treatment: combines pharmacotherapy with a full
program of assessment, psychosocial intervention and support services; it is the
approach with the greatest likelihood of long-term success for many consumers.
Maintenance treatment is typically indicated for the first two years of a methadone
program.
• Medical Maintenance Treatment: is provided to stabilize consumers and may include
long-term provision of methadone, buprenorphine, or naltrexone with a reduction in
clinic attendance and other services. A consumer may receive medical maintenance at
an OTP after he or she is stabilized fully and typically subsequent to the first two years
of a methadone program.
The minimum required services for MAT are outlined in Federal regulations (42 Code of Federal
Regulations [CFR], Part 8). The MDHHS-BHDDA has published Treatment Policies for both
methadone and buprenorphine/naloxone. These treatment policies are identified in the
reference section of this document and are available on the MDHHS website.
Eligibility Criteria:
To be eligible for medication assisted treatment services funded through MSHN, the intended
recipient must meet the level of care (LOC) determination using the most current edition of the
American Society of Addiction Medicine Patient Placement Criteria (ASAM-PPC) and the most
current Diagnostic and Statistical Manual of Mental Disorders (DSM). Medical necessity
requirements shall be used to determine the need for methadone or buprenorphine/naloxone as
an adjunct treatment and recovery service (Medicaid Provider Manual). Further, the intended
recipient should be assessed for the ability to benefit from MAT services, including the stage of
change in which the consumer is presenting. Individuals are afforded a choice of provider upon
determination of appropriate level of care.
A medical examination at admission will rule out chronic pain disorder without a diagnosis of
OUD considered to necessitate use of opioids. It is the expectation that consumers seeking
opioids for chronic pain issues will be referred to an appropriate medical provider. MSHN does
not fund the use of methadone or buprenorphine/naloxone for pain management. A clear
diagnosis of Opioid Use Disorder must be present prior to any MSHN funds being utilized for
consumers with chronic pain.
General Expectations:
Individual needs and rate of progress vary from person-to-person and, as such, treatment and
recovery must be individualized and based on the needs and goals of the individual (Treatment
Policy #06: Individualized Treatment Planning, 2012). Collaborative care ideally includes:
“multiple professional, individual patients, family members, and to assist patients as they
maneuver through often complex multi-component systems of care,” (Waller, 2014, p.14). The
use of case managers, care coordinators, and recovery coaches is recommended for individuals
whenever possible (Treatment Policy #08: Substance Abuse Case Management Requirements,
2008). Increasing the individual’s recovery capital through these supports, will assist the

71
recovery process and help the individual to become stable and more productive within the
community.
Counseling services should be conducted by the opioid treatment program (OTP) that is
providing the methadone whenever possible and appropriate. When the ASAM LOC is not
outpatient or when a specialized service is needed, separate service locations for methadone
dosing and other substance use disorder services are acceptable, as long as coordinated care is
present and documented in the individual’s record. (Treatment Policy #05: Criteria for Using
Methadone for Medication-Assisted Treatment and Recovery, 2012). These exceptions must be
approved by the MSHN Utilization Management (UM) Department prior to admission into
another treatment program. Please see the Dual Program Enrollment section of the UM Manual
for further instruction.
Comprehensive Treatment Planning:
MSHN expects the provider to begin working on a comprehensive treatment plan with EVERY
consumer immediately upon admission and be able to show documentation of assisting the
consumer with developing a comprehensive recovery plan, which includes but should not be
limited to: building a recovery support network, developing a relapse prevention plan, achieving
a stable living environment, securing stable employment (when appropriate), and improving
overall wellness and quality of life.
Progress will be measured by the documentation of active participation in treatment as
evidenced by: quantifiable evidence of progress toward goals and objectives on a collaborative
recovery plan designed to address treatment, promote recovery and self-sufficiency; reduction
in problem severity, and negative toxicology screens or evidence of engagement in strategies to
address recovery.
According to the Medication-Assisted Treatment Guidelines for Opioid Use Disorder (Waller,
2014), if there is evidence that progress is not being made toward agreed-upon goals, the
diagnosis, treatment modalities, treatment intensity, and treatment goals will be reassessed in
order to revise the treatment plan rather than introduce a premature termination from
treatment.
All agencies that provide methadone assisted treatment will be responsible for completing the
annual assessment to determine if the consumer will continue in treatment and to update
assessment information. An annual assessment is required in order to ensure that consumers
continue to qualify for MSHN-funded substance use disorder treatment services. At this time,
and throughout treatment, the consumer should also be evaluated and educated on the
possibility of tapering off their medication. Tapering should be done with significant consumer
input due to increased relapse potential. Throughout the course of medication-assisted
treatment, specific documentation must be included in the consumer file which evidences
attempts at decreasing the dosage tapering off of the medication, decreasing problem severity,
and provider assisting the consumer in achieving employment and other recovery goals that
promotes self-sufficiency. Without such documentation medication-assisted treatment services
may cease to be funded.

72
Consumers funded through Medicaid for buprenorphine/naloxone or methadone may continue
treatment according to their specific Medicaid benefit as long as medically necessary and
clinically appropriate. Justification for this continued treatment must be documented in the
consumer file and in the REMI system, including treatment attendance, medical necessity, and
ASAM Patient Placement Criteria.
Regulatory Compliance/Coordination of Care:
Legally prescribed medication including controlled substances must be presented to the
physician, who will decide whether these prescriptions are appropriate for the patient who is
taking methadone. Coordination of care with the prescribing physician is required. Upon
admission (within five business days), a release of information and a letter explaining
consumer’s involvement in MAT will be faxed to the prescribing physician, with a copy being
placed in the consumer file.
All MAT providers will require that consumers provide a complete list of all prescribed
medications. Legally prescribed medication, including controlled substances, must not be
considered as illicit substances when the provider has documentation that it was prescribed for
the consumer. Legally prescribed medications that are not being used as prescribed will be
treated as illicit substances and must be documented in the consumer file. Approved examples
of such documentation include copies of the prescription label, pharmacy receipt, or pharmacy
printout.
A Michigan Automated Prescription System (MAPS) report must be completed at admission into
the program (“Treatment Policy #05: Criteria for Using Methadone for Medication-Assisted
Treatment and Recovery,” 2012). For consumers receiving methadone, a MAPS report must be
completed prior to initial dosing and prior to off-site dosing being approved. Off-site dosing is
not allowed without documented coordination of care by the MAT provider's physician and the
prescriber of identified controlled substances, which include, but may not be limited to:
Opioid/Opiates, benzodiazepines, stimulants and muscle relaxants. This coordination must be
documented in the doctor’s notes. Documentation must be individualized, identifying the
consumer, the diagnosis, and the length of time the consumer is expected to be on the
prescribed medication.
If a MAPS report shows prescriptions of controlled substances, this will be addressed on the
consumer’s individualized treatment plan.
According to Treatment and Recovery Policy #05: Criteria for Using Methadone for Medication-
Assisted Treatment and Recovery (2012, p. 5), “Michigan law allows for individuals with the
appropriate physician approval and documentation to use medical marijuana. Although there
are no prescribers of medical marijuana in Michigan, individuals are authorized by a physician to
use marijuana per Michigan law. For enrolled individuals, there must be a copy of the MDHHS
registration card for medical marijuana issued in the individual’s name in the [consumer] chart
or the ‘prescribed medication log’.” A copy of the consumer's
registration card
must be included
in the consumer chart and documented in REMI.
Drug Screens:

73
Drug screens for consumers receiving methadone assisted treatment are considered part of the
daily dosing rate. For consumers receiving buprenorphine/naloxone services, there are two
codes available for drug screens: H0003 Laboratory Analysis for Drug Screen and H0048 Instant
Drug Testing Collection and Handling Only. H0048 should be used for most screens and H0003
only when medically necessary. For further information regarding appropriate use of drug
screens, please contact the UM Department at 844-405-3095.
METHADONE ASSISTED TREATMENT
Methadone Assisted Treatment Expectations:
Disclaimer: the use of medications, or not, is the responsibility of the medical practitioner with
which the consumer is engaged and nothing in MSHN protocols should be interpreted as
medical advice, promotion of one form of medication over another, or in any other way to
interfere with or modify the physician’s orders or practice.
General minimum service requirements for authorizing methadone assisted treatment services:
• Comprehensive biopsychosocial assessment with an initial diagnosis of Opioid Use
Disorder of at least one-year duration;
• Coordination of care with all prescribing physicians, treating physicians, dentists and
other health care providers;
• Physical examination upon admission and as appropriate during the course of treatment;
• Daily attendance requirements for medication dispensing;
• Must be used as an adjunct to Opioid Use Disorder treatment which must include a
counseling component;
• Mandatory toxicology screening at intake and randomly thereafter, toxicology screening
must assay for Opioid/Opiates, cocaine, barbiturates, amphetamines, cannabinoids,
benzodiazepines and methadone metabolites; urinalysis testing shall be performed for
consumers in accordance with Federal, State, and Licensing rules.
• Identification, treatment, or referral for treatment of co-occurring disorders and
neuropsychological problems;
• Counseling to assist in discontinuation of substance abuse and manage drug cravings
and urges;
• Evaluation of and interventions to address family problems;
• HIV and Hepatitis C Virus (HCV) education, counseling, and referral for testing and/or
care; and,
• Referral for additional services as needed.
Behavioral Contracts:
It is MSHN’s expectation that all consumers and providers will adhere to the rules of MAT as
dictated by MSHN as well as the Federal and State governments. However, as per the
Department of Health and Human Services memo dated June 29, 2017, MSHN will not support
the use of behavioral contracts in its provider network. Similarly, MAT providers shall not
mandate or require behavioral contracts for any of their consumers receiving MAT services.

74
Illicit use should be addressed in a meaningful way on the consumer’s individualized treatment
plan.
Block Grant Waitlist for Methadone Assisted Treatment:
At times, the demand for an individual funded through Block Grant and seeking methadone
services may exceed capacity. When this occurs, the MSHN UM Department will place the
individual on a waiting list. Census of the Block Grant funded individual must remain static. As
such, methadone assisted treatment providers may admit an individual approved by the MSHN
Utilization Management Department,
only when a treatment slot becomes available
. Such
admission slots become available only when an existing individual funded through Block Grant is
discharged from treatment services; whether due to program non-compliance, transfer to self-
pay status, obtaining Medicaid, or successful program completion.
The individual funded through Block Grant and placed on the waiting list should 1) be
encouraged to go to local Outpatient treatment services while on the waiting list, 2) be
encouraged to apply for Medicaid or Healthy Michigan Plan, and 3) be told to contact the MSHN
UM Department if he/she obtains Medicaid or Healthy Michigan Plan and is still interested in
receiving methadone assisted treatment services. An individual on the Block Grant waiting list
will be admitted to methadone assisted treatment services according to his/her current priority
status on the waiting list.
When an admission slot becomes available, the MSHN UM Department will make three attempts
to contact the next consumer on the Block Grant waiting list (according to priority status) via
telephone. If unable to make contact with consumer via telephone, the MSHN UM Department
will move to the next consumer according to priority status and repeat the above process until a
consumer is successfully contacted.
Consumers so contacted, will be warm transferred to a methadone assisted treatment provider
of their choice to arrange for an admission appointment. Consumers contacted will have 14
calendar days from the date of initial contact to be admitted into methadone-assisted treatment
services. After 14 calendar days have lapsed, the methadone assisted treatment provider will
contact MSHN UM Department indicating whether the consumer failed to present for admission.
If the consumer fails to present at the methadone assisted treatment provider within 14
calendar days of initial contact by MSHN UM Department, the provider will inform MSHN UM
Department. MSHN UM Department will then review the waiting list to determine the next
consumer to be admitted to methadone-assisted treatment services according to their current
priority status.
If the consumer does present at the methadone assisted treatment provider within 14 calendar
days, the provider will inform MSHN UM Department of the consumer's admission date.
Block Grant-funded consumers meeting criteria for urgent priority population (pregnant
injecting drug users and pregnant substance abusers) will be allowed direct admission into
methadone assisted treatment, if appropriate and will not be placed on the Block Grant waiting
list.

75
Individuals funded through Medicaid or Healthy Michigan Plan will not be placed on the Block
Grant or any other waiting list. Consumers determined to meet eligibility criteria for this level of
care will be directed to the provider of their choice.
For buprenorphine/naloxone assisted services: consumers receiving buprenorphine/naloxone
assisted services will not be placed on a waiting list. Buprenorphine/naloxone assisted services
are NOT an alternative to methadone assisted treatment services. Therefore, if a consumer is
assessed as needing methadone assisted treatment services, they would not be placed in
treatment with buprenorphine/naloxone. Consumers cannot receive buprenorphine/naloxone
while on the waiting list for methadone-assisted treatment services.
BUPRENORPHINE/NALOXONE ASSISTED TREATMENT
Medically Supervised Withdrawal Treatment using buprenorphine/naloxone (Suboxone):
A consumer entering an outpatient program with buprenorphine/naloxone will usually not
require sub-acute detoxification services prior to admission to the outpatient program. It is
expected that the majority of consumers will enter directly into buprenorphine/naloxone-
assisted treatment at the outpatient level without first receiving services through inpatient
withdrawal management . Special exceptions should be referred to MSHN UM Department at 1-
844-405-3095.
According to the Treatment Improvement Protocol #40: Clinical Guidelines for the Use of
Buprenorphine in the Treatment of Opioid Addiction (McNicholas, 2004, p. 48), as published by
the U.S. Department of Health and Human Services (USDHHS), Substance Abuse and Mental
Health Services Administration (SAMHSA), Center for Substance Abuse Treatment (CSAT):
"The literature suggests that the use of buprenorphine for gradual detoxification over long
periods is probably more effective than its use for rapid detoxification over short or moderate
periods. Patients who are unwilling or unable to engage actively in rehabilitation services
without agonist support may not be appropriate candidates for short-term detoxification,
however such patients may benefit from long-term detoxification (or even more so, from
maintenance treatment)."
DISCONTINUATION/TERMINATION/READMISSION
Services are discontinued/terminated, either by Completion of Treatment or through
Administrative Discontinuation. Refer to the following subsections for additional
information.
COMPLETION OF TREATMENT
The decision to discharge a beneficiary must be made by the OTP's or OBOT’s physician, with
input from clinical staff, the beneficiary, and the parent, legal guardian, or responsible adult
(designated by the relevant state authority/CPS). Completion of treatment is determined

76
when the beneficiary has fully or substantially achieved the goals listed in their
individualized treatment and recovery plan and no longer needs methadone as a
medication. As part of this process, a reduction of the dosage to a medication-free state
(tapering) should be implemented within safe and appropriate medical standards.
ADMINISTRATIVE DISCONTINUATION
Administrative discontinuation/discharge refers to termination of medication assisted treatment
(MAT) due to non-compliance with treatment recommendations, and/or engaging in activities or
behaviors that impact the safety of other consumers and/or staff in the treatment
environment.
Process for Implementing Administrative Discontinuation:
Repeated episodes of non-compliance or other infractions should be considered on a case-by-
case basis. Unless there is an immediate and urgent safety concern, the provider should
document efforts taken to assist consumers in coming into compliance. If unsuccessful in
achieving compliance, a warm transfer should (when it’s possible) be attempted and facilitated
to another MAT provider.
Administrative discharge can leave the consumer at risk of severe withdrawal symptoms,
relapse, overdose and death. It should be a last resort when other efforts have been
unsuccessful. METHADONE: Administrative discontinuation of services can be implemented
by
Immediate Termination
or
Enhanced Tapering Discontinuation
which involves accelerated
decrease of the methadone dose (usually by 5 percent a day).
(Sources: Medicaid Provider Manual 12.2.F.2, p.87-89 & Treatment Policy #5, p.9-11)
It may be necessary for the OTP to refer beneficiaries who are being administratively
discharged to another level of
care. Justification for non-compliance termination must be documented in the
beneficiary's chart. An Adverse Benefit Determination should be issued, when applicable.
INCLUDED SERVICES
Medication-Assisted Treatment in an outpatient setting is intended for the purpose of 1)
managing the effects of withdrawal from opioids (prescription painkillers and heroin) and/or
alcohol; 2) stabilizing the consumer and 3) providing maintenance treatment. Ancillary services
such as individual therapy, group therapy, Recovery Supports, acupuncture, and/or Case
Management will be available during a consumer's episode of care.
Covered services for methadone and pharmacological supports and laboratory services, as
required by Federal regulations and the Administrative Rules for Substance Abuse Service
Programs in Michigan, include:
• Methadone medication

77
• Nursing services
• Physical examination
• Physician encounters (monthly)
• Laboratory tests
• TB skin test (as ordered by physician)
AUTHORIZATION PARAMETERS
Please see the MSHN Utilization Management authorization parameters included in REMI for a
complete list of codes.
Please note the following:
• A reauthorization will not be approved unless the provider has entered
every
toxicology
report for the consumer into REMI prior to the reauthorization request.
• Providers will be required to complete an annual re-assessment for continuing care and
will enter re-assessment information into REMI.
• Additional services such as medication reviews, drug screens, and actual dosing may
vary depending on the service provider.
MAT GUEST DOSING
Guest dosing is allowable between different locations of the same MAT provider. The two
locations are to have an internal policy for documentation and payment.
MEDICAL MARIJUANA CARD: EXPECTATION OF PROVIDERS
If the consumer does not consent to coordination of care with all prescribing physicians,
including the physician who certified the use of medical marijuana, off-site dosing will not be
permitted in accordance with Treatment and Recovery Policy #05: Criteria for Using Methadone
for Medication-Assisted Treatment and Recovery (2012, p. 5
).
ALCOHOL USE DISORDER & MEDICATION-ASSISTED TREATMENT
Medication-Assisted Treatment (MAT) for alcohol use disorder includes three FDA approved oral
medications that help reduce cravings for alcohol and can be a component of MAT in working
with consumers struggling with alcohol use disorder. The MSHN expectation is that medication
will be an adjunct to other services like outpatient individual and group therapy, case
management and peer recovery supports as dictated by ASAM and medical necessity.
1.
Disulfiram (
Brand name:
Antabuse)
– This medication blocks an enzyme that is involved in
metabolizing alcohol. Disulfiram produces unpleasant side effects when combined with
alcohol in the body.
Antabuse
is used in certain people with chronic alcoholism. This
medicine can help keep the consumer from drinking because of the unpleasant side effects
that will occur if consuming alcohol while taking
Antabuse
.
Antabuse
is used together with
behavior modification, psychotherapy, and counseling support to help stop drinking. Any
foods, beverages, products that contain alcohol or medications that contain alcohol MUST

78
be avoided when using disulfiram. Also, many patients with other health issues may not be
safe candidates for disulfiram.
2.
Acamprosate Calcium (Brand name: Campral)
– This medication helps promote
abstinence from alcohol in patients with alcohol dependence
who are abstinent at treatment
initiation
. Treatment with Acamprosate
should be part of a comprehensive management
program that includes psychosocial support. The efficacy of Acamprosate
in promoting
abstinence has been demonstrated most effective in subjects who have undergone
detoxification and achieved alcohol abstinence prior to beginning Campral treatment. The
efficacy of Campral in promoting abstinence from alcohol in polysubstance abusers has not
been adequately assessed.
3.
Naltrexone HCL (Brand name: Re-Via, Vivitrol)
This medication, (an opiate antagonist that
works in the brain to prevent feelings of well-being, paint relief, etc.) is used to treat alcohol
abuse by reducing cravings. It can help consumers drink less alcohol or stop drinking
altogether. The efficacy of naltrexone in promoting abstinence has been demonstrated most
effective in subjects who have undergone detoxification and achieved alcohol abstinence
prior to beginning naltrexone treatment. It decreases the desire to drink alcohol when used
with a treatment program that includes counseling, support, and lifestyle changes.
PLEASE NOTE: The medications referenced in this section are not funded through MSHN.
However, MSHN will fund medically appropriate ancillary services that accompany medication
like outpatient therapy, case management and peer recovery supports for consumers receiving
these medications as part of their substance abuse treatment.
BENZODIAZAPINE USE DISORDER & MEDICATION-ASSISTED TREATMENT
Medication-Assisted Treatment (MAT) for Benzodiazepine Use Disorder includes the
anticonvulsant medication
Neurontin
. The MSHN expectation is that medication will be adjunct
to other services like outpatient individual and group therapy, case management and peer
recovery supports as dictated by ASAM and medical necessity.
Gabapentin (Brand name: Neurontin)
– The anticonvulsant Neurontin has demonstrated a
positive impact on reducing cravings for benzodiazepines as well as offering a reduction in the
severity of withdrawal effects like seizures and anxiety. Recently, there have been reports of
patients overusing or misusing gabapentin. Gabapentin remains an important medication in
treating SUD with various drugs. Patients receiving gabapentin should be followed carefully,
prescribed in the lowest effective dose and receive counseling around this issue. Gabapentin
should not be stopped abruptly. It may be prudent in certain situations to give one refill at a
time and monitor for misuse. Other anticonvulsants such as carbamazepine and valproate have
shown benefits also.
PLEASE NOTE: The medications referenced above are not funded through MSHN. However,
MSHN will fund medically appropriate ancillary services that accompany medication like
outpatient therapy, case management and peer recovery supports for consumers receiving
these medications as part of their substance abuse treatment.

79
ATTENTION: Please note that use of gabapentin (Neurontin), carbamazepine and valproate to
reduce cravings and/or to reduce the severity of withdrawal symptoms is not FDA-approved.
There is evidence of its effectiveness for this use, however. Any decision regarding use of this
medication for MAT purposes should only take place after a transparent and clear conversation
between doctor and patient regarding benefits and risks and notification of its FDA status.
COCAINE USE DISORDER & MEDICATION-ASSISTED TREATMENT
Medication-Assisted Treatment (MAT) for cocaine use disorder includes two oral medications
that help reduce cravings. The MSHN expectation is that medication will be adjunct to other
services like outpatient individual and group therapy, case management and peer recovery
supports as dictated by ASAM and medical necessity. These medications include:
1.
Desipramine
, an antidepressant may be helpful in patients with cocaine use disorder, with
depression and without antisocial personality disorder. May work with patients with
comorbid opioid use disorder on buprenorphine MAT or along with contingency
management.
2.
Disulfiram
(250 mg/day) blocks conversion of dopamine to norepinephrine and has been
shown to be helpful for cocaine use disorder. It is FDA approved for alcohol use disorder.
3.
Topiramate
(an anticonvulsant) has also shown benefit in decreasing cocaine use.
4.
Bupropion HCL (Brand name: Wellbutrin)
- Wellbutrin is most commonly used for
depression but has been shown to help reduce cravings for cocaine.
PLEASE NOTE: The medications referenced above are not funded through MSHN. However,
MSHN will fund medically appropriate ancillary services that accompany medication like
outpatient therapy, case management and peer recovery supports for consumers receiving
these medications as part of their substance abuse treatment.
ATTENTION: Please note that use of Desipramine, Disulfiram, Topiramate, and Bupropion HCL
(Wellbutrin) to reduce cravings is not FDA-approved. There is evidence of its effectiveness for
this use, however. Any decision regarding use of this medication for MAT purposes should only
take place after a transparent and clear conversation between doctor and patient regarding
benefits and risks and notification of its FDA status.
METHAMPHETAMINE USE DISORDER AND MEDICATION ASTED TREATMENT.
Recent studies have suggested that a combination of IM naltrexone (Vivitrol) monthly combined
with oral bupropion (Wellbutrin and others) may be modestly effective in reducing craving for
and use of methamphetamine. Several other medications have been tried in order to diminish
cravings for methamphetamine. These have shown little success. Psychosocial approaches such
contingency management, CBT, group therapy, diagnosing and treating psychiatric illness and
even exercise programs have shown some benefit.
MARIJUANA USE DISORDER & MEDICATION-ASSISTED TREATMENT

80
Medication-Assisted Treatment (MAT) includes two medications that have been effective as one
component of working with consumers who have marijuana use disorder. The MSHN
expectation is that medication will be adjunct to other services like outpatient individual and
group therapy, case management and peer recovery supports as dictated by ASAM and medical
necessity.
1.
Gabapentin (Brand name: Neurontin)
– The anticonvulsant Neurontin, used primarily
to treat seizures, has demonstrated a positive impact on reducing cravings for marijuana
as well as a reduction in the severity of withdrawal effects in adults. Recently there
have been reports of patients overusing or misusing gabapentin. Gabapentin remains an
important medication in treating SUD with various drugs. Patients receiving gabapentin
should be followed carefully, prescribed the lowest effective dose and receive counseling
around this issue. Gabapentin should not be stopped abruptly. It may be prudent in
certain situations to give one refill at a time and monitor for misuse.
2. Acetylcysteine (
(Brand name: Mucomyst)
– This medication, when inhaled, helps open
the airways due to lung diseases such as emphysema, bronchitis, cystic fibrosis and
pneumonia. When taken orally, Acetylcysteine helps prevent liver damage caused by an
overdose of acetaminophen (Tylenol). For use with adolescent consumers abusing
marijuana, this medication may help reduce cravings according to one study.
PLEASE NOTE: The medications referenced above are not funded through MSHN. However,
MSHN will fund medically appropriate ancillary services that accompany medication like
outpatient therapy, case management and peer recovery supports for consumers receiving
these medications as part of their substance abuse treatment.
ATTENTION: Please note that use of gabapentin (Neurontin) to reduce cravings and/or to
reduce symptoms associated with withdrawal from marijuana use is not FDA-approved. There is
evidence of its modest effectiveness for this use, in some studies. Any decision regarding use
of this medication for MAT purposes should only take place after a transparent and clear
conversation between doctor and patient regarding benefits and risks and notification of its FDA
status.
REFERENCES AND IMPLEMENTATION GUIDANCE
The U.S. Department of Health and Human Services, Substance Abuse and Mental Health
Services Administration, Center for Substance Abuse Treatment, has issued treatment
improvement protocols (TIPs) to assist with the implementation of these services.
Treatment Improvement Protocol #43 (TIP-43), “Medication-Assisted Treatment for
Opioid/Opiate Addiction in Opioid/Opiate Treatment Programs ", Substance Abuse and Mental
Health Services Administration, Center for Substance Abuse Treatment
(http://www.atforum.com/SiteRoot/pages/addiction_resources/MAT-TIP_43-
MMT_Guidelines2005.pdf)
Treatment Improvement Protocol #40 (TIP-40), “Clinical Guidelines for the Use of
Buprenorphine in the Treatment of Opioid/Opiate Addiction", Substance Abuse and Mental
81
Health Services Administration, Center for Substance Abuse Treatment (available from
http://buprenorphine.samhsa.gov/Bup_Guidelines.pdf)
Substance Abuse Treatment/Recovery Policy # (TP-5), “Criteria for Using Methadone for
Medication - Assisted Treatment/Recovery", Michigan Department of Community Health, Bureau
of Substance Abuse and Addiction Services (available from
http://www.michigan.gov/documents/Treatment_Policy_05_Enrollment_Criteria_for_Methadone
_145925_7.pdf)
Substance Abuse Treatment/Recovery Policy # (TP-3), “Buprenorphine", Michigan Department
of Community Health, Bureau of Substance Abuse and Addiction Services (available from
http://www.michigan.gov/documents/Treatment_Policy_03_Buprenorphine_145923_7.pdf)
“Medication for the Treatment of Alcohol Use Disorder: A Brief Guide,” Substance Abuse and
Mental Health Services Administration, Center for Substance Abuse Treatment (available from
http://store.samhsa.gov/shin/content//SMA15-4907/SMA15-4907.pdf )
Additional resources used in the development of this treatment protocol include:
Michigan Medicaid Provider Manual (available from http://www.mdch.state.mi.us/dch-
medicaid/manuals/MedicaidProviderManual.pdf)
American Society of Addiction Medicine Patient Placement Criteria-3
rd
Edition (available from
http://www.asam.org/publications/patient-placement-criteria)
Waller, R.C., MD, MS. “Medication-Assisted Treatment Guidelines for Opioid Use Disorders”,
(available from https://macmhb.org/sites/default/files/attachments/files/Waller%20-
%20Opioid%20Tx%20Guidelines.pdf).

82
Appendix B: Recovery Housing Technical Requirement
Purpose
To establish requirements as the Pre-Paid Inpatient Health Plan (PIHP) for the implementation
of recovery housing. Individuals with substance use disorders (SUD) who have embarked on a
treatment and recovery pathway often have living environments in the community that
contributed significantly to their drug and/or alcohol abuse. It puts them at risk for relapse and
death. Recovery housing is a vital resource for individuals seeking a supportive housing
environment that can promote and sustain the recovery process.
Definitions
Recovery housing is defined by the Office of Recovery Oriented Systems of Care (OROSC) as
“providing a location where individuals in early recovery from a behavioral health disorder are
given time needed to rebuild their lives, while developing the necessary skills to embark on a
life of recovery. This temporary arrangement will provide the individual with a safe and secure
environment to begin the process of reintegration into society, and to build the necessary
recovery capital to return to a more independent and functional life in the community. These
residences provide varying degrees of support and structure. Participation is based on individual
need and the ability to follow the requirements of the program.” Recovery housing is expected
to be a safe, structured, and substance free environment.
The Substance Abuse and Mental Health Services Administration
(SAMHSA) goes on to say:
“… Recovery housing benefits individuals in recovery by reinforcing a substance-free lifestyle
and providing direct connections to other peers in recovery, mutual support groups and
recovery support services. Substance-free does not prohibit prescribed medications taken
as directed by a licensed prescriber, such as pharmacotherapies specifically approved by the
Food and Drug Administration (FDA) for treatment of opioid use disorder as well as other
medications with FDA-approved indications for the treatment of co-occurring disorders.
(Additional information regarding recovery housing best practices can be found on the SAMHSA
website located here.)
Policy
Across Region 5’s twenty-one counties, MSHN supports active and vibrant recovery communities
of which recovery housing is a critical component. Drawing on MDHHS’s Office of Recovery-
Oriented Systems of Care (OROSC)’s Treatment Technical Advisory #11, the National Alliance of
Recovery Residences (NARR) guidelines, and clinical best practices, MSHN has established the
following expectations of recovery houses which are part of MSHN’s SUD provider network.
Consumers residing in recovery housing must be actively engaged in formal
outpatient treatment with a credentialed outpatient provider.
It is the expectation that
an assessment by a credentialed SUD treatment provider be completed prior to admission.
Information including the name and date, if known, of the provider who completed the
assessment should be documented on the recovery housing Screening and Intake form. In the
instance a person has successfully completed a SUD residential episode, and has met the
criteria for recovery housing, but is not connected to an outpatient provider, the recovery

83
provider will have 14 days to connect the person to an outpatient provider. (See SAMHSA
“Recovery Housing Best Practices” for additional information).
Case management, although part of the outpatient treatment services, is not sufficient on its
own. Recovery housing is an adjunct to treatment and an individual in recovery housing must
attend treatment in a formal outpatient setting at least one time in 30 days to receive funding
for recovery housing. The recovery housing provider is responsible for monitoring consumer
attendance in treatment by coordinating care with the treatment provider. Evidence of
coordination of care efforts must be located in the consumer’s file. Recovery housing must be
identified in the consumer’s recovery plan and the recovery plan must also be present in the
consumer’s recovery housing file.
Service Description
MSHN expects recovery housing providers to employ recovery coaches to enhance a consumer’s
recovery experience. If the provider cannot offer this service, they must coordinate care with
another local provider of recovery coaching services while the recovery house actively seeks to
hire a
trained
recovery coach.
The provider of the recovery house will maintain a file on each consumer admitted. All provided
services must be formally documented on the consumer’s individual service/recovery plan. This
includes, but is not limited to, individual peer support services, peer group services, and/or case
management. All services provided must be documented via an individualized progress note.
All progress notes should include a summary of what occurred during the service, start and stop
time, date of service, and be signed by the facilitator. In addition, facilitators must indicate any
relevant certification/credential and list the date the note was signed.
The recovery house file should include but not be limited to:
• Basic demographic information
• Releases of information are required in consumer file for the following: primary care
physician, outpatient provider, MSHN, emergency contact
• Primary Care Physician information needs to minimally include the physicians name,
practice name, address, and telephone number to meet MDHHS standards.
• Evidence of enrollment with an outpatient provider
• Application
• Screening: This includes an agency screening as well as the Brief Screening completed
in REMI
• Signed consumer acknowledgement of discussion and receipt of recovery housing rules
and expectations
• Recovery Plan developed with the consumer and recovery coach and included in the
consumer’s file at the Recovery House. Recovery/Service Plans must include the
following components:
• Individualized Plans of Service developed in partnership with the consumer as
evidenced by the consumer’s words
• Goals & objectives are written using specific, measurable, attainable, realistic &
time limited elements.
• Evidence of regular care coordination with service providers
• Evidence of regular attendance with a formal outpatient provider
• Evidence of regular drug screening, if necessary (this service is not billable to MSHN)

84
• Evidence of weekly house meetings
• Recovery coaching progress notes if recovery coaching is being provided on location
• Block Grant Income Eligibility & Fee Determination form
It is the expectation of MSHN that consumers who meet clinical criteria will be admitted to
services regardless of their participation in a medication assisted treatment program.
Length of Stay
MSHN will fund up to 90 days of recovery housing based upon determination of need. Recovery
housing is limited to one admission per 12-month period. Recovery housing providers should
screen individuals prior to admission to determine if the person has participated in recovery
housing within the last 12 months. Recovery housing providers can also contact the MSHN UM
Department to confirm an individual’s eligibility for MSHN-funded recovery housing services.
Recovery housing providers will work with each consumer and the consumer’s outpatient
treatment provider to develop an individualized plan identifying either alternative housing to
which the consumer will go after discharge or alternative sources of funding to pay for the
consumer’s continued stay in recovery housing.
Utilization Patterns
Recovery housing providers will submit an authorization request in REMI for recovery housing
services (H2034) for a maximum of 90 days.
MSHN requires that recovery houses be certified through MARR/NARR at a level III
or higher. A level III recovery house has administrative oversight and provides
more structure than levels I and II and has at least one paid staff person. A level IV
recovery house is highly structured and employs administrative and credentialed
clinical staff.
Standards for Recovery Housing
Access – Screening: All recovery houses should have a standard screening tool which
determines if the person is appropriate for recovery housing and rules out admission of
individuals who may present a safety risk to self, staff, or other residents.
Access - Application for Admission: Once screened as admissible due to an absence of
safety concerns, recovery houses should have an application process that allows for current
residents to offer input on prospective new residents. This input should not constitute veto
power over any individual’s admission. Clear criteria should be established regarding what are
and are not appropriate variables for residents to consider. Race, religion or sexual orientation,
for example, should
not
be considered relevant for consideration whereas a known history for
being emotionally abusive corroborated by multiple residents might be relevant for
consideration by the group.
Admission Policy: It is the expectation that all recovery housing providers have a policy and
procedure in place which outlines admission criteria. This should include, but is not limited to:
• Criteria designating the amount of time a person is established in their recovery prior to
admission.

85
• Process to ensure that a person has been connected to and receiving services from a
treatment provider prior to consideration for recovery housing.
• Criteria that would preclude an individual from being admitted into recovery housing.
Health and Safety: All recovery houses should have an on-call emergency contact who is
available on a 24/7/365 basis. The individual who is on-call does not need to be on-site but
does
need to be accessible by phone during non-business hours including evenings, weekends
and holidays. Recovery houses should consistently have Naloxone Rescue kits immediately on
hand.
House Rules & Meetings: Recovery houses play a critical role in establishing a sense of what
a healthy and functional family (in this case, a surrogate family) can look like. Towards that
end, house rules including mutual respect, clear and appropriate boundaries and shared division
of labor should be in place. Weekly house-meetings should take place at the house where
residents live and where they are permitted to strengthen relationships, share concerns, air
grievances and problem-solve disputes in a way that allows for and models healthy and
respectful dialogue. If a recovery house has multiple locations in a community, there is value in
having a regular meeting that brings together multiple houses to establish a larger sense of a
recovery community beyond the individual recovery house. This multi-house recovery
community meeting should not replace the house-level meeting more than once per month.
This establishes an expectation that the house will function like a family unit with a designated
weekly time that the unit comes together to ensure things are operating smoothly.
MAT-inclusion: Medication assisted treatment (MAT) is another vital resource needed by
many individuals, particularly those with an opioid use disorder. MAT and recovery houses
evolved out of separate communities, siloed service delivery systems, and disparate belief
systems, resulting in a severely limited supply of recovery houses that adequately support
persons receiving MAT. In 2018, NARR, produced a White Paper titled “MAT-Capable Recovery
Residences: How government can enhance and expand recovery residence capacity to
adequately support Medication Assisted Recovery.” NARR notes that “A residence [RR] may
deny residency based on eligibility requirements that are essential to the safety and welfare of
the residents and maintenance of the recovery support environment. While an applicant
prescribed MAT can be legally denied for other reasons,
categorical exclusions solely based on
the MAT prescription violate provisions of the ADA
[emphasis added].” NARR refers individuals
who face discrimination or exclusion based on their use of MAT to the SAMHSA
“Know Your
Rights”
brochure here which concludes simply: “It is illegal to discriminate against people
because they are on MAT.”
MSHN’s expectation is that recovery houses in MSHN’s provider network will comply with federal
law and NARR standards and will be inclusive of people who are on Medication Assisted
Treatment. If technical assistance is needed regarding how to integrate people on MAT in a
recovery house with people who are on an abstinence-based recovery pathway, please contact
your MSHN Treatment Specialist for assistance.
Reporting Criteria: Any overdose or incident that requires the administration of Narcan on
the property must be reported through the Incident Review for Substance Use Disorder (SUD)
Providers process as required within 48 hours of the occurrence.

86
Training for Recovery Housing Staff: In addition to Peer Recovery Coach training, and
trainings required by MSHN, the following trainings are highly
recommended
for all recovery
housing staff. Please refer to the MSHN Regional Training Grid attached to your contract for a
list of all
required
trainings.
• Peer Recovery Support Service (PRSS) plan – How to write them, implement them and
document them
• Progress notes – What to include
• Care Coordination – How to coordinate with other providers (treatment, PCPs, social or
legal services, etc.)
• Ethics
• First Aid/CPR
Please check MSHN’s weekly newsletter in Constant Contact for news of upcoming trainings.
Warm Transfer: In the event that the recovery house does not have the capacity to meet the
needs of an individual, appropriate services, will be identified and a warm transfer will be
conducted between the recovery house and the identified services.
References/Legal Authority
• Treatment Technical Advisory #11: Recovery Housing
(http://www.michigan.gov/documents/mdhhs/TA_T_11_Recovery_Housing_532174_7.pdf)
• National Alliance of Recovery Residences (http://narronline.org)
• SUD Treatment- Income Eligibility & Fees (http://www.midstatehealthnetwork.org/provider-
network/docs/Finance%20-%20Income%20Eligibility%201%200-08-2015.pdf)
• SUD Treatment- Income Eligibility & Fee Determination
(http://www.midstatehealthnetwork.org/provider-network/docs/Finance%20-
%20SUD%20Income%20Eligibility%20Procedure.pdf)
• Mid-State Health Network Substance Use Disorder Provider Manual
(http://www.midstatehealthnetwork.org/provider-
network/docs/MSHN%20SUD%20Provider%20Manual%20Final%202-1-17.pdf)
• Michigan Association of Recovery Residences (https://narronline.org/cm-business/michigan-
association-of-recovery-residences/)
• National Alliance for Recovery Residences (http://narronline.org/)

87
Appendix C: Technical requirement for SUD Transportation Services
MSHN strives to reduce transportation barriers to accessing SUD treatment and recovery
services, using the best quality, consumer-friendly, cost-efficient means possible. Transportation
services are not a guaranteed benefit and are limited by the availability of Substance Abuse
Block Grant funding during each fiscal year. Transportation needs must be identified during the
screening and assessment process and clearly documented within the consumer’s individualized
treatment plan. If transportation needs arise during the course of a treatment episode,
documentation of the need must be included in the consumer chart (i.e.: progress note,
treatment plan review, recovery plan, etc.) and it must be included on an amended treatment
or recovery plan. The treatment or recovery plan must include goals related to helping the
consumer reduce barriers to transportation and must promote consumer self-sufficiency and
empowerment.
Transportation services authorized by the PIHP are available only after all other transportation
options have been exhausted. These options include but are not limited to natural/community
supports and local MDHHS transportation assistance.Efforts to obtain other available and
appropriate means of transportation must be documented in the consumer chart and shall be
subject to MSHN confirmation. For consumers using transportation services, a transportation log
must be included in the consumer chart. Transportation logs must include the following: date of
service, signature/initials of consumer and program staff person(s), purpose of transportation
and destination(s) with total mileage or number of bus tickets or gas cards issued.
The MSHN Utilization Management department will monitor the utilization of transportation
codes region-wide and will work closely with the MSHN Finance department to monitor
availability of block grant funding for transportation assistance.
LEVEL OF CARE
Withdrawal Management& Residential Treatment
Transportation services are available to all consumers who meet medical necessity criteria for
these levels of care. The withdrawal management residential service provider is responsible for
determining the consumer’s transportation needs during the course of the screening process.
The following parameters apply to transportation services for these levels of care:
• Least costly method of transportation must be used; starting travel begins at the
consumer’s home and/or point of pick up (i.e., bus station) and destination is complete
when consumer reaches the designated treatment center.
• Justification for using a form of transportation assistance other than least costly must be
documented in the consumer chart. Examples of justification for using other forms of
transportation include but are not limited to: the consumer does not reside on a public
transportation route; the consumer has a specific physical or emotional disability which
would make utilizing public transportation a hardship for that consumer; or the
impairment caused by the consumer’s substance use disorder poses safety concerns or
high risk of relapse when using public transportation.
Routine transportation provided to the consumer during the course of the residential treatment
episode is considered intrinsic in the residential service delivery and is factored into the per
diem reimbursement rate for residential treatment services (H0018/H0019).

88
Available Transportation Codes
• A0110 Bus Transportation- supporting documentation (i.e.: receipt for Greyhound bus
ticket, etc.) must be uploaded to REMI at the time the claim is submitted
• S0215 Non-Emergency Transportation (per mile)- IRS mileage reimbursement rate; May
be used by treatment center to bill for transportation expense in cases where treatment
center staff members provide transportation to the consumer. This service code may
only be used when long-distance bus transportation is not available or if this is the least
costly means of transportation; May be used in combination with long-distance bus
transportation to transport consumer from the bus station to the treatment center; May
also be used when treatment center staff provide transportation to consumers
throughout the duration of the residential treatment episode for excessive, non-routine
transportation as outlined above.
• T2003 Gas Card- $5.00 per unit; this code is available only if the individual is unable to
utilize a bus route to get to the withdrawal management or residential treatment
program. The maximum units permitted depends on distance to the treatment facility
and must be clearly documented in the consumer chart. The provider is responsible for
evaluating individual need and assisting consumers with planning.
Outpatient
Transportation assistance is available for outpatient SUD services for Women’s Specialty
Consumers and their dependent children only.
Public transportation (bus tokens) should be the first method of transportation used, whenever
possible. Justification for using a form of transportation assistance other than public
transportation (bus tokens) must be documented in the consumer chart. Examples of
justification for using other forms of transportation include but are not limited to: the consumer
does not reside on a public transportation route; the consumer has a specific physical or
emotional disability which would make utilizing public transportation a hardship for that
consumer; or the impairment caused by the consumer’s substance use disorder poses safety
concerns or high risk of relapse when using the public transportation system.
AVAILABLE TRANSPORTATION CODES
• A0110 Bus Tokens- $1.50 per unit; consumers may be given the number of tokens
necessary for one round trip between their home and the recovery treatment provider
for each day they attend treatment. The same limitation applies, per day, for each
dependent child accompanying a consumer to Women’s Specialty treatment services.
• T2003 Gas Card- $5.00 per unit; this code is available only for consumers who do not
reside on a public transportation route. The maximum units permitted depends on
individual consumer needs and must be clearly documented in the consumer chart. The
provider is responsible for evaluating individual need and assisting consumers with
planning.
• S0215 Mileage – IRS mileage reimbursement rate; May be used in addition to A110
if/when consumer requires transportation from public transportation point to treatment
facility; May also be used to assist consumers with recovery-oriented service access
outside of the treatment center. Mileage is to be utilized using least costly methods and
only when required to assist consumers with treatment plan goals.

89
Appendix D: MSHN Informed Consent Related to MAT
Assurance of Informed Consent
Regarding Medication Assisted Treatment (MAT)
I have been fully informed about the treatment and recovery options that are available to me
for substance use disorder treatment. MSHN’s “Recovery Pathways for Opioid Use Disorders”
information sheet was provided to me and explained.
• Medication-Assisted Treatment (MAT) was explained to me as the use of doctor-
prescribed medications, in combination with counseling, case management, and
recovery supports for the treatment of addiction.
• It was explained to me that MAT can successfully treat addictions, and can reduce
cravings, prevent relapse and overdose, and help sustain recovery.
• I was given the opportunity to ask and discuss my questions and concerns to my
satisfaction.
• I have felt encouraged to choose the recovery pathway that is best for me at this time,
and I feel my choice in recovery pathways has been respected.
I have read the statements above and had sufficient time to consider them carefully. I have
been fully informed of my treatment options. With my signature below, I attest that I am
choosing to engage in treatment with _____________________ [
Provider Name
]. I understand that I can
stop treatment at any time, and, upon request, I can receive information and assistance with
transferring to a different provider of my choice.
__________________________________
________________________________
Consumer Signature Consumer Name (Printed)
__________________________________
Date
__________________________________ ________________________________
Intake Staff Signature Intake Staff Name (Printed)
NOTE: MSHN’s “Recovery Pathways for Opioid Use Disorders” was provided and explained (initial here):
________
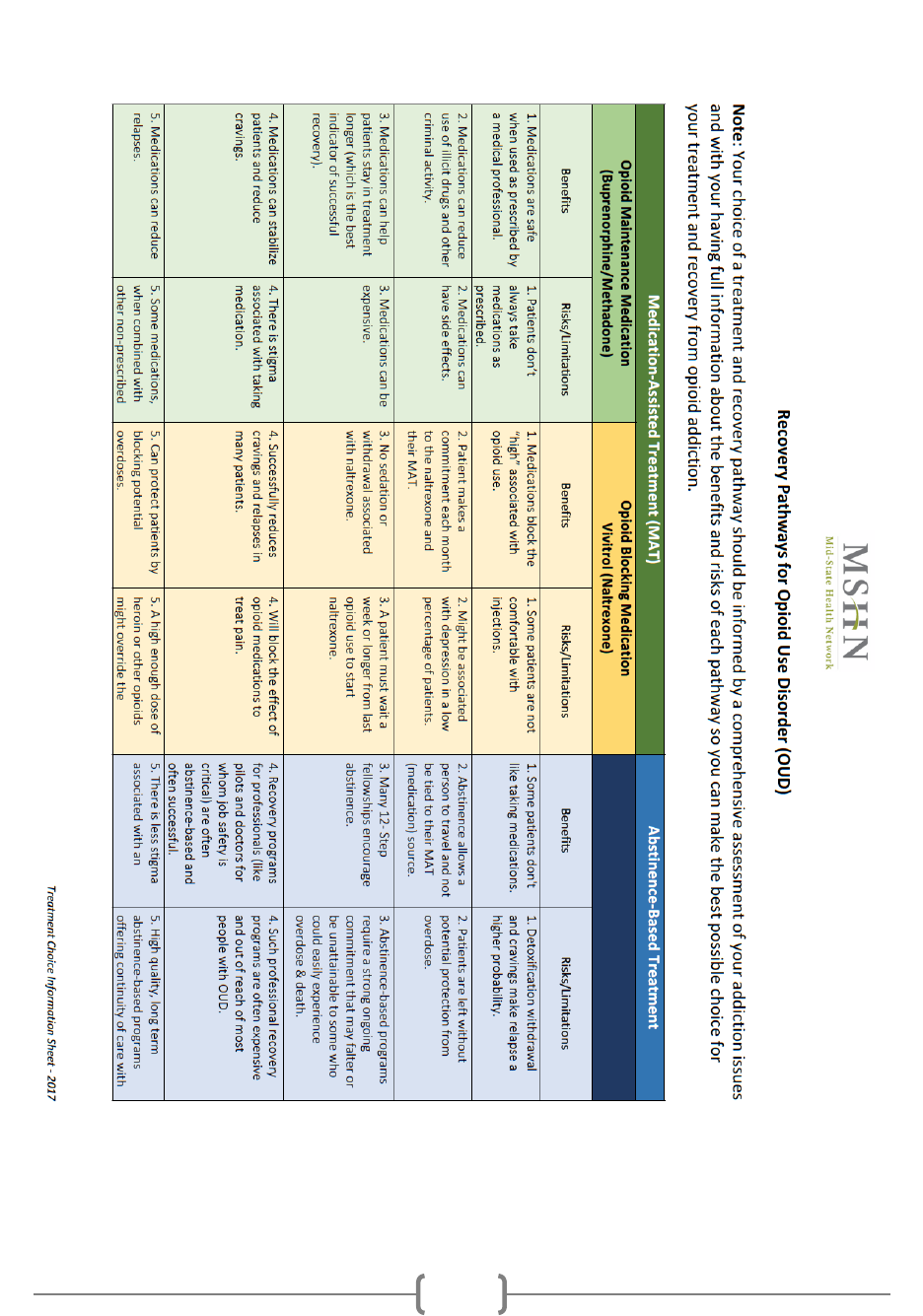
90
Appendix E: Informational Grid on Recovery Pathways for Opioid Use Disorder
(OUD)

91
Informational Grid on Recovery Pathways for Opioid Use Disorder (OUD)
