
Guidance for Industry
Preclinical Assessment of
Investigational Cellular and Gene
Therapy Products
Additional copies of this guidance are available from the Office of Communication, Outreach
and Development (OCOD), (HFM-40), 1401 Rockville Pike, Suite 200N, Rockville, MD 20852-
1448, or by calling 1-800-835-4709 or 301-827-1800, or e-mail [email protected], or from the
Internet at
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guida
nces/default.htm.
For questions on the content of this guidance, contact OCOD at the phone numbers or e-mail
address listed above.
U.S. Department of Health and Human Services
Food and Drug Administration
Center for Biologics Evaluation and Research
November 2013
Contains Nonbinding Recommendations
Table of Contents
I. INTRODUCTION............................................................................................................. 1
II. BACKGROUND............................................................................................................... 2
III. PRECLINICAL STUDY CONSIDERATIONS............................................................. 4
A. Preclinical Program Objectives........................................................................... 4
B. Recommendations for General Preclinical Program Design............................ 4
1. Investigational CGT Products Used in Preclinical Studies................... 4
2. Animal Species Selection.......................................................................... 5
3. Selection of Animal Models of Disease/Injury........................................ 6
4. Proof-of-Concept (POC) Studies............................................................. 7
5. Toxicology Studies .................................................................................... 9
6. Product Delivery Considerations........................................................... 11
7. Good Laboratory Practice (GLP).......................................................... 12
8. The Principles of Reduction, Refinement, and Replacement of Animal
Use ............................................................................................................ 13
9. Product Development for Later-Phase Clinical Trials........................ 14
10. Preclinical Study Reports....................................................................... 14
11. Communication with OCTGT Pharmacology/Toxicology Staff ........ 15
IV. RECOMMENDATIONS FOR INVESTIGATIONAL CELL THERAPY (CT)
PRODUCTS..................................................................................................................... 15
A. Introduction......................................................................................................... 15
B. Animal Species/Model(s).................................................................................... 16
C. Study Designs ...................................................................................................... 18
D. CT Product Fate Post-Administration.............................................................. 18
1. Survival/Engraftment............................................................................. 19
2. Distribution.............................................................................................. 19
3. Differentiation and Integration ............................................................. 20
4. Tumorigenicity........................................................................................ 20
E. CT Products with Implantable Scaffolds.......................................................... 21
1. Cells.......................................................................................................... 21
2. Scaffolds................................................................................................... 21
3. Biocompatibility...................................................................................... 21
4. Cell Seeding ............................................................................................. 22
5. Study Groups........................................................................................... 22
6. Biological Responsiveness ...................................................................... 22
7. Dose Response and Durability of the Response ................................... 22
8. Safety........................................................................................................ 23
V. RECOMMENDATIONS FOR INVESTIGATIONAL GENE THERAPY (GT)
PRODUCTS..................................................................................................................... 23
A. Introduction......................................................................................................... 23
B. Animal Species/Model(s).................................................................................... 23
C. Study Designs ...................................................................................................... 24
i
Contains Nonbinding Recommendations
ii
1. Overall Safety Considerations............................................................... 24
2. Vector-Specific Considerations.............................................................. 25
3. Transgene Considerations...................................................................... 26
4.
Ex vivo
Genetically Modified Cells ....................................................... 27
5. Biodistribution Considerations.............................................................. 27
VI. RECOMMENDATIONS FOR INVESTIGATIONAL THERAPEUTIC VACCINES
........................................................................................................................................... 28
A. Introduction......................................................................................................... 28
B. Animal Species/Model(s).................................................................................... 29
C. Study Designs ...................................................................................................... 29
VII. CONCLUSION ............................................................................................................... 29
VIII. REFERENCES................................................................................................................ 30

Contains Nonbinding Recommendations
Guidance for Industry
Preclinical Assessment of Investigational Cellular and Gene
Therapy Products
This guidance represents the Food and Drug Administration’s (FDA’s) current thinking on this
topic. It does not create or confer any rights for or on any person and does not operate to bind
FDA or the public. You can use an alternative approach if the approach satisfies the
requirements of the applicable statutes and regulations. If you want to discuss an alternative
approach, contact the appropriate FDA staff. If you cannot identify the appropriate FDA staff,
call the appropriate number listed on the title page of this guidance.
I. INTRODUCTION
The Center for Biologics Evaluation and Research (CBER)/Office of Cellular, Tissue and Gene
Therapies (OCTGT) is issuing this guidance to provide sponsors and individuals that design and
implement preclinical studies with recommendations on the substance and scope of preclinical
information needed to support clinical trials for investigational cellular therapies, gene therapies,
therapeutic vaccines, xenotransplantation, and certain biologic-device combination products
which OCTGT reviews (hereinafter referred to as CGT products).
1
This guidance finalizes the draft guidance entitled “Guidance for Industry: Preclinical
Assessment of Investigational Cellular and Gene Therapy Products” dated November 2012 and
supersedes the recommendations in section VIII in the guidance entitled “Guidance for Industry:
Guidance for Human Somatic Cell Therapy and Gene Therapy” dated March 1998 (Ref. 1). We
have revised our recommendations to reflect our current knowledge gained through
advancements in the field and through experience gained through OCTGT’s review of CGT
products. Thus, this guidance clarifies OCTGT’s current expectations regarding the preclinical
information that would support an Investigational New Drug Application (IND)
2
and a
Biologics License Application (BLA)
3
for these products.
1
This guidance applies only to CGT products which are regulated under Section 351 of the Public Health Service
Act (PHS Act) (42 U.S.C. 262) which OCTGT reviews. This guidance does not apply to therapeutic vaccines for
infectious disease indications that are typically reviewed in CBER/Office of Vaccines Research and Review
(OVRR).
2
See Title 21 of the Code of Federal Regulations (CFR) Part 312 (21 CFR Part 312).
3
See 21 CFR Part 601.
1

Contains Nonbinding Recommendations
CGT products within the scope of this guidance meet the definition of “biological product” in
section 351(i) of the PHS Act (42 U.S.C. 262(i)). For a CGT product that is also a component of
a combination product
4
such as a CGT product and a dedicated delivery system, a single IND is
generally sufficient. The IND application should contain preclinical information, as described in
this guidance, on the biological product and on the delivery system, along with any other
information required by the applicable regulations.
This guidance does not apply to those human cells, tissues, and cellular and tissue-based
products (HCT/P’s)
regulated solely under section 361 of the PHS Act (42 U.S.C. 264) as
described under 21 CFR Part 1271 or to products regulated as medical devices under 21 CFR
Part 820. This guidance also does not apply to the therapeutic biological products for which the
Center for Drug Evaluation and Research (CDER)
5
has regulatory responsibility. In addition,
this guidance does not apply to those biological products which OVRR reviews (for example,
preventive (prophylactic) vaccines), or to those biological products that CBER’s Office of Blood
Research and Review reviews.
We note that we have previously provided guidance documents incorporating recommendations
regarding preclinical development for several specific product areas (Refs. 2 through 7). This
guidance is intended to complement that information.
FDA’s guidance documents, including this guidance, do not establish legally enforceable
responsibilities. Instead, guidances describe the FDA’s current thinking on a topic and should be
viewed only as recommendations, unless specific regulatory or statutory requirements are cited.
The use of the word should in FDA’s guidances means that something is suggested or
recommended, but not required.
II. BACKGROUND
The general content and format of information to be included in the submission of an IND can be
found in 21 CFR 312.23. Section 312.23(a)(8) states that, prior to administration of an
investigational pharmaceutical agent in a clinical trial, the sponsor must provide “[a]dequate
information about the pharmacological and toxicological studies…on the basis of which the
sponsor has concluded that it is reasonably safe to conduct the proposed clinical investigations.
The kind, duration, and scope of animal and other tests required vary with the duration and
nature of the proposed clinical investigations.” The design and conduct of preclinical
pharmacological and toxicological studies are thus important to inform regulatory decisions that
help define the safe administration of an investigational CGT product in humans. The specific
4
Forward specific questions regarding jurisdiction over a combination product to the Office of Combination
Products (OCP) at 301-427-1934 or [email protected]
. Information about the Request for Designation (RFD)
program and guidance related to the regulation of combination products are available at the OCP website
http://www.fda.gov/oc/combination
. Forward questions regarding the applicability of specific regulations to
products, for which jurisdiction has already been determined, to the FDA Center with jurisdiction.
5
Information pertaining to those therapeutic biological products that were transferred from CBER to CDER can be
found at:
http://www.fda.gov/AboutFDA/Centers
Offices/OfficeofMedicalProductsandTobacco/CBER/ucm186789.htm.
2

Contains Nonbinding Recommendations
product characteristics and putative mechanism(s) of action (MOA(s)), the target disease
indication, and the method of product delivery will help define the elements and design of the
preclinical testing program.
OCTGT is responsible for the regulation of CGT products for a variety of clinical indications.
These products are frequently the result of novel manufacturing processes, and/or contain
components that have not been previously tested in formal toxicology studies or in clinical trials.
We note that the general scientific principles within the fields of pharmacology and toxicology
apply to CGT products; however, specific terms (e.g., absorption, distribution, metabolism, and
excretion (ADME)) either may not apply, or do not currently have widely accepted definitions
with respect to use with CGT products. The diverse biology and clinical indications and the
rapid and fluid state of the evolving scientific research into these product areas pose unique
scientific challenges in terms of regulatory review.
As a consequence, the regulatory review process for evaluation of investigational CGT products
necessitates a careful risk-benefit analysis performed in the context of the particular clinical
indication under study. The intrinsic material composition and putative MOA(s) of CGT
products differ from small molecular weight drugs, macromolecular biologic drugs (i.e.,
therapeutic proteins), and medical devices. Therefore, the traditional, standardized approaches
for preclinical toxicity testing, which were developed for drug development and device testing,
are often not appropriate for evaluating the safety of CGT products. OCTGT uses a flexible,
science-driven review process to address safety issues in a context that considers both the
biology (and biomechanics if applicable) of the product and the intended clinical indication.
Although flexible, such an approach incorporates the basic toxicological principles that underlie
more traditional, standardized preclinical testing.
6
Inherent in such an approach to regulation is the need for communication between the sponsor
and the review office. Given the significant pace at which information pertaining to novel CGT
products is accumulating as a consequence of basic research, we recommend early and ongoing
communication with OCTGT Pharmacology/Toxicology staff during product development.
These communications help to ensure that regulatory expectations related to safety,
demonstration of potential activity, and understanding of possible MOA(s) are addressed.
6
Although CGT products fall outside the scope of the International Conference on Harmonisation (ICH) Safety (S)
guidances, the basic testing principles in the following documents may be useful as reference: “Guidance for
Industry: S6 Preclinical Safety Evaluation of Biotechnology-Derived Pharmaceuticals” dated July 1997 and
“Guidance for Industry: S6 Addendum to Preclinical Safety Evaluation of Biotechnology-Derived Pharmaceuticals”
dated May 2012 available at
http://www.fda.gov/Drugs/GuidanceComplianceRegu
latoryInformation/Guidances/ucm065007.htm.
3

Contains Nonbinding Recommendations
III. PRECLINICAL STUDY CONSIDERATIONS
A. Preclinical Program Objectives
The preclinical studies that are conducted are an important element of the overall
development pathway for an investigational product. The overall objectives for a
sufficient preclinical program for a CGT product include, as applicable:
1. Establishment of biological plausibility.
2. Identification of biologically active dose levels.
3. Selection of potential starting dose level, dose-escalation schedule, and dosing
regimen for clinical trials.
4. Establishment of feasibility and reasonable safety of the investigational
product’s proposed clinical route of administration (ROA).
5. Support of patient eligibility criteria.
6. Identification of physiologic parameters that can guide clinical monitoring.
7. Identification of potential public health risks (e.g., to the general public,
caregivers, family members, close contacts (for example co-workers), and
intimate contacts).
The resulting data from preclinical studies should address these objectives in order to
guide the design of early-phase clinical trials, as well as establish a platform for the
conduct of future preclinical studies, such as reproductive/developmental toxicity studies,
that may be needed to support later phases of product development.
B. Recommendations for General Preclinical Program Design
1. Investigational CGT Products Used in Preclinical Studies
When possible, the investigational CGT product that will be administered to the
patient population should be used in the definitive preclinical studies.
7
Recommendations germane to specific product types are discussed throughout
this document. Each lot of an investigational CGT product used in the preclinical
in vitro and in vivo studies should be characterized according to appropriate
criteria, consistent with the stage of product development (Refs. 8 and 9).
Similarities and differences between product lots intended for preclinical use and
7
For purposes of this guidance, the term “definitive preclinical studies” also referred to as “pivotal preclinical
studies,” are the key IND-enabling studies that are conducted to assess the overall safety and rationale for
administering a CGT product in humans. These studies should be based on safety and proof-of-concept data
obtained from smaller, pilot studies.
4

Contains Nonbinding Recommendations
lots intended for clinical use should be highlighted and discussed in the IND
submission. However, in certain cases, due to the species-specific nature of the
clinical product (e.g., some vector-expressed human transgenes: human-derived
cellular therapy (CT) products), testing the CGT product intended for clinical
administration in animals may not be informative, and therefore testing of an
analogous product may be a suitable alternative.
8
In these situations, the design
of the preclinical testing program is considered on a product-by-product basis.
Considerations regarding investigational product incompatibility issues are
discussed in section IV.B. of this document for CT products and in section V.B.
for gene therapy (GT) products.
2. Animal Species Selection
The animal species selected for assessment of bioactivity and safety should
demonstrate a biological response
9
to the investigational CGT product similar to
that expected in humans in order to generate data to guide clinical trial design.
Some factors that should be considered when determining the relevant species
include: a) comparability of physiology and anatomy to that of humans; b)
permissiveness/susceptibility to infection by, and replication of, viral vectors or
microbial vectors for gene therapy; c) immune tolerance to a human CT product
or human transgene expressed by a GT product; and d) feasibility of using the
planned clinical delivery system/procedure.
Assessment of these factors necessitates consideration of the specific product and
clinical indication. “Non-standard” test species, such as genetically modified
rodents (i.e., transgenics or knockouts) or large animals (e.g., sheep, pigs, goats,
and horses) may be acceptable when adequate justification is provided. Although
safety and effectiveness of the investigational CGT product in vitro and in vivo
can possibly be evaluated in one animal species, other contributory factors (e.g.,
source of the CGT product, ROA) may result in the need for testing in more than
one species. Prior to initiation of the definitive preclinical studies, we recommend
the conduct of in vitro studies (e.g., functional assays, immunophenotyping,
morphologic evaluation) and in vivo pilot studies, to establish the biological
relevance of a specific animal species to the investigational product(s).
We recommend that sponsors conduct a detailed assessment of the relevancy of
each animal species used in support of each potential clinical trial. A summary of
this assessment should be submitted as part of the preclinical section of the IND.
8
For purposes of this guidance, analogous cellular products are cellular products derived from the animal species
used for testing that are analogs of the ultimate clinical product in phenotype and biologic activity.
9
For purposes of this guidance, a “biological response” is a pharmacological response to the administered product.
5
Contains Nonbinding Recommendations
3. Selection of Animal Models of Disease/Injury
Preclinical studies performed in animal models of disease/injury may provide
insight regarding the relationships of dose to activity and toxicity. Animal models
of disease/injury that are used in basic research or discovery science phases of
product development are also potentially useful for generating data to support
clinical trials for CGT products. Due to features of CGT products (e.g.,
potentially prolonged duration of intended product effect, product persistence in
vivo, complex MOA involving interaction between the CGT product and the
disease environment, invasive ROA), animal models of disease/injury may be
preferable to healthy animals to assess the activity and safety of these products.
Therefore, preclinical studies in disease/injury models are encouraged to better
define the risk-benefit ratio associated with investigational CGT products. In
addition, use of disease/injury models provides the opportunity for possible
identification of activity-risk biomarkers that may be applicable for monitoring in
clinical trials.
a. Information describing limitations of potential animal model(s)
Potential limitations of these preclinical animal models can exist. Examples
of these limitations include:
i. Inherent variability of the model.
ii. Limited historical/baseline data for the model.
iii. Technical limitations with the physiological and anatomical
constraints of the model.
iv. Animal care issues.
v. Limited fidelity in modeling human pathophysiology of the
disease/injury of interest.
Each model has inherent strengths and weaknesses; thus, no single model will
predict with complete accuracy the efficacy and safety outcome of the
investigational CGT product in the patient population. The activity and safety
profile of the CGT product may be influenced by the timing of administration
relative to the onset of disease, thus the disease state at the initiation of
product administration should be characterized and documented in the IND
submission.
6
Contains Nonbinding Recommendations
b. Information supporting the choice of animal model(s)
The IND submission should include information supporting the
usefulness/ability of the selected animal model(s) to mimic the target disease
population and to permit assessment of the safety of the investigational CGT
product that takes into account each of the following:
i. The similarities and differences between the pathophysiology of the
disease/injury animal model and the pathophysiology of the
disease/injury of humans.
ii. The effect of the disease/injury status of the animal on the
pharmacology/toxicology of the investigational CGT product (i.e.,
altered sensitivity of the animal model to the specific product under
study).
iii. Detrimental effects of the administered product on existing disease/
injury status (i.e., exacerbation of an existing disease/injury condition
or induction of a new disease/toxicity).
We recommend that, when appropriate, sponsors consider using a tiered
approach for determining selection of an appropriate animal model.
Performance of pilot studies involving the intended investigational CGT
product may assist in evaluating the suitability of a particular animal
species/model for use in the definitive preclinical studies. Moreover, multiple
animal models may be necessary to adequately identify functional aspects and
potential toxicities of a single product under study. In these situations, the
preclinical testing paradigm may include the use of 1) large and small animal
models, 2) multiple small animal models, or 3) only large animal models.
The number and type of studies performed will be guided by the biological
attributes of the investigational CGT product. Please refer to current CBER
guidances (Refs. 2 through 4) that include information and recommendations
regarding tiered testing approaches for CGT products.
4. Proof-of-Concept (POC) Studies
A primary objective of POC studies is to establish the feasibility and rationale for
use of an investigational CGT product in the targeted patient population. POC
studies help inform the benefit side of the risk-benefit assessment of the CGT
product. Such data may be essential in the assessment of novel products with
substantial inherent risks. In addition, data from POC studies can contribute
significantly to animal species selection (refer to section III.B.2 of this document).
POC studies should investigate the following:
7
Contains Nonbinding Recommendations
a. The pharmacologically effective dose range (i.e., minimally effective dose
and optimal biological dose).
b. Optimization of the ROA and confirmation that the CGT product reaches
the target anatomic site/tissue/cell.
c. Optimization of the timing of product administration relative to onset of
disease/injury.
d. Optimization of the dosing schedule.
e. Characterization of the putative MOA or hypothesized biological activities
of the investigational CGT product.
Collectively, this information serves to establish the rationale for, and feasibility
of, the proposed clinical trial. Features of study design, such as the inclusion of
appropriate concurrent controls, randomization, or blinding methods, may
increase the strength of the resulting study data, thus should be considered.
Preclinical in vitro assays intended to assess aspects of the biological activity of
an investigational CGT product (e.g., growth factor secretion, immunological
response profile, expression of a neurotransmitter) can provide supporting POC
information.
Use of in vitro studies is strongly encouraged for identification of potential safety
issues and MOA of an investigational CGT product. However, this testing alone
is not sufficient to reliably anticipate the outcome of physiological and functional
integration of the product following in vivo administration. Accordingly, the
preclinical testing program should incorporate a stepwise, multifactorial approach
to achieve an understanding of the biological plausibility for use of the
investigational CGT product in the intended patient population.
For in vivo preclinical testing, the use of animal models of disease/injury is
encouraged, as such studies allow for the characterization of resulting
morphological changes in conjunction with observable functional/behavioral
changes. For a general discussion regarding these animal models, refer to section
III.B.3 of this document.
Data derived from in vitro and in vivo preclinical POC testing can guide the
design of both the preclinical toxicology studies, as well as the early-phase
clinical trials, while contributing to defining reasonable risk for the investigational
CGT product in the intended patient population.
8
Contains Nonbinding Recommendations
5. Toxicology Studies
Preclinical assessment of the safety of an investigational CGT product contributes
to the definition of an acceptable risk-benefit ratio for a proposed clinical trial.
The safety assessment should be sufficiently comprehensive to permit
identification, characterization, and quantification of potential local and systemic
toxicities, their onset (i.e., acute or delayed), the possibility for resolution of any
toxicities, and the effect of product dose level on toxicity findings.
a. Primary considerations for toxicology study design:
Each of the following should be considered in the design of the toxicology
study:
i. The proposed clinical indication.
ii. The amount and quality of published preclinical or clinical safety
information for the specific CGT product under investigation or for a
similar product (i.e., known toxicities or adverse effects).
iii. The amount and quality of existing pharmacology (in vitro/in vivo) or
POC data for the specific CGT product under investigation or for a
similar product.
iv. Previous preclinical/clinical experience with the proposed clinical
delivery device/delivery procedure or with any related
device/procedure.
v. The biological responsiveness of the animal species to the
investigational CGT product.
vi. The putative MOA of the CGT product.
vii. The intrinsic properties of the CGT product.
viii. The pathophysiology of the animal disease/injury model, if one is
used.
Animal species in which the CGT product is biologically active should be used in
the toxicology studies; supporting data should be provided that justify species
selection (refer to section III.B.2 of this document). Although healthy animals
represent the standard model test system employed to conduct traditional
toxicology studies, study designs using animal models of disease/injury are
frequently modified to incorporate important safety parameters that allow for
9
Contains Nonbinding Recommendations
assessment of the potential toxicology of an investigational CGT product (i.e.,
hybrid pharmacology-toxicology study design). Such data can supplement, or
possibly be used in lieu of toxicology studies in healthy animals.
b. Secondary considerations for toxicology study design
The overall design of the toxicology studies should mimic the proposed
clinical trial design as closely as possible. Preclinical toxicology study
designs should include the following, as applicable:
i. Adequate numbers of animals per gender that are appropriately
randomized to each group. If the number of animals that can be dosed
in a single day is limited due to the complexity of the dosing procedure or
the timing of product administration relative to disease status of the
model, then appropriate randomization methods or other factors should be
considered in an attempt to reduce study bias as much as possible.
The
number of animals required for each group will vary depending on the
safety concerns for the investigational CGT product, the species,
model, and the delivery system.
ii. Appropriate control groups. Examples include animals that are left
untreated, receive sham surgery, or are administered formulation
vehicle only, adjuvant alone, null vector, or scaffold alone.
Justification should be provided for the specific control group(s)
selected.
iii. Multiple dose levels of the investigational CGT product, which should
bracket the proposed clinical dose range, if feasible. Results obtained
from POC studies should guide selection of the target dose levels for
both preclinical safety assessment and for clinical development. The
highest dose level used in preclinical models may be restricted due to
animal size, tissue volume/size, ROA, or product manufacturing
capacity. Justification, with supporting data, should be provided for
the specific dose levels selected.
iv. A dosing schedule that reflects the intended clinical dosing regimen, to
the extent possible.
v. A ROA that mimics the intended clinical route as closely as possible.
The delivery device intended for use in the clinical studies should be
used to administer the investigational CGT product in the definitive
toxicology studies; justification should be provided if the intended
clinical delivery device is not used. As discussed in section III.B.6 of
this document, additional preclinical studies may be necessary to
assess the safety of a delivery device and the delivery procedure.
10
Contains Nonbinding Recommendations
vi. Multiple sacrifice time points to capture potential acute, chronic,
and/or delayed-onset toxicities, as well as the potential for resolution
of toxicities. The time intervals designated for the sacrifice time
points will depend on the animal model used, the investigational
product, the dosing schedule, the pharmacodynamic and
pharmacokinetic response observed, and the proposed patient
population. The POC studies, as well as the GT product tissue
biodistribution profile and the CT product fate post-administration,
should help guide the selection of study duration and sacrifice time
intervals.
vii. Safety endpoints that capture potential toxicities. Standard parameters
monitored include mortality (with cause of death determined, if
possible), clinical observations, body weights, physical examinations,
food consumption/appetite, water consumption (as applicable), clinical
pathology (serum chemistry, hematology, coagulation, urinalysis),
organ weights, gross pathology, and histopathology.
viii. Additional parameters specific to either the investigational CGT
product used and/or specific to the intended patient population.
Examples of product-specific study parameters include humoral or
cellular immune responses, vector biodistribution, CT product fate,
behavioral testing, neurological exams, ophthalmic exams, cardiac
assessments, imaging (i.e., MRI, ultrasound, radiography), presence of
abnormal/ectopic growths (i.e., hyperplasia, tumors), putative
biomarkers, and specialized histopathology (i.e., immunohisto-
chemistry). The data collected should include both morphological and
functional assessment, whenever possible, to determine whether an
association exists between non-terminal and terminal findings.
Reversibility of any findings should also be addressed. Refer to other
sections of this document for guidance that is specific to product class.
These preclinical data will help guide clinical trial design. For example, data
generated from the toxicology studies will potentially establish a No-Observed-
Adverse-Effect-Level (NOAEL), which will help determine selection of the
starting dose level and subsequent dose-escalation scheme for the clinical trial. In
addition, this information will potentially allow for circumvention or mitigation of
significant toxicities in patients.
6. Product Delivery Considerations
The ROA used to deliver the investigational CGT product in the definitive
preclinical studies should mimic the ROA to be employed in the clinical setting to
the greatest degree possible. If it is not possible to replicate the clinical ROA in
the animal model, then alternative routes/methods should be proposed and
scientifically justified as a part of the preclinical development plan.
11
Contains Nonbinding Recommendations
To assess the potential risks associated with the method of product administration,
the delivery device system used in the definitive preclinical studies should be
identical to the planned clinical product delivery device, if possible. In definitive
studies where the planned clinical delivery device system cannot be used,
justification for the delivery system that is utilized should be provided. The IND
sponsor is responsible for providing sufficient data to allow FDA to determine the
safety of the delivery device system. The IND submission should state whether a
device master file (MAF) has been submitted to the Center for Devices and
Radiological Health (CDRH) for the delivery device. If a MAF exists, the IND
submission should include a letter of authorization from the MAF holder granting
permission for FDA to cross-reference specific information in the MAF. CBER
will consult with CDRH review staff as necessary to determine whether the
information provided in the device MAF is sufficient in detail (e.g., facilities and
manufacturing procedures and controls; synthesis, formulation, purification and
specifications for chemicals, materials; biocompatibility (Ref. 10), preclinical
data; clinical study data) to support use in the clinical trial. If a MAF for the
delivery device does not exist or if the information is not sufficient to support the
proposed use, CDRH review staff may be consulted to determine the type and
extent of information that should be included in the IND submission to support
the use of the device in the proposed clinical trial.
Potential risks that may be associated with use of a novel device and/or delivery
procedure for an investigational CGT product should be identified and evaluated.
The use of a large animal species (healthy animal or a disease/injury model) to
test the safety of a delivery device may be appropriate in certain situations, such
as assessment of risk associated with use of a previously untested device for
intracranial product delivery, or assessment of risk associated with use of an
investigational delivery system for placement of the CGT product into the heart or
the brain. As indicated above, safety data for the delivery device and delivery
procedure may derive from existing active regulatory submissions (i.e., INDs,
Investigational Device Exemptions (IDEs), MAFs). As also indicated above, in
these circumstances, the IND submission for the investigational CGT product
should include letters of cross-reference from the sponsors of these existing
submissions. Published studies that involve the use of the clinical delivery device
and delivery procedure may also provide supportive safety data.
7. Good Laboratory Practice (GLP)
According to 21 CFR Part 58 (Part 58), all preclinical toxicology studies are to be
conducted in compliance with GLP. However, we recognize that some
toxicology assessments may not fully comply with the GLP regulations. For
example, toxicology data for investigational CGT products are sometimes
collected in POC studies that use an animal model of disease/injury, which may
require unique animal care issues and technical expertise that may not be
available at a GLP testing facility. Similarly, studies that incorporate some
12

Contains Nonbinding Recommendations
endpoints included in the toxicology study, such as vector biodistribution, cell
fate, or specific immunological endpoints may not be available at a GLP testing
facility. Compliance of in vitro and in vivo pharmacology/POC studies with GLP
is not required. If collection of safety endpoints (i.e., histopathology) in such
studies is planned, conduct of these study parameters in compliance with GLP is
recommended.
“For each nonclinical laboratory study subject to the [GLP] regulations under part
58, a statement that the study was conducted in compliance with [GLP] in part 58,
or, if the study was not conducted in compliance with those regulations, a brief
statement of the reason for the noncompliance,” must be submitted in the final
study report (21 CFR 312.23(a)(8)(iii)). This explanation should include the areas
of deviation and whether the deviation(s) impacted study outcome. However, in
these instances, consideration should be given to having an independent Quality
Assurance (QA) unit/person provide an oversight function with respect to the
conduct of the toxicology study and each resulting final study report (similar to
that described in 21 CFR 58.35).
Preclinical studies that incorporate safety parameters in the study design should
be conducted using a prospectively designed study protocol. Results derived from
these studies should be of sufficient quality and integrity to support the proposed
clinical trial. A summary of all deviations from the prospectively designed study
protocol and their potential impact on study integrity and outcome should be
provided in the preclinical study report.
8. The Principles of Reduction, Refinement, and Replacement of Animal Use
The recommendations in this guidance incorporate the principles of the “3Rs,” the
fostering of test method protocols that encourage reducing, refining, and replacing
animal use, and the applicable provisions of the Animal Welfare Act
Amendments of 1976 (7 U.S.C. 2131 et seq.), including the use of institutional
animal care and use committees (IACUCs).
10
The preclinical program for each
investigational CGT product should be individualized with respect to scope,
complexity and design in order to maximize the predictive value of these studies
for clinical safety and therapeutic activity. We encourage sponsors to take
advantage of opportunities for reducing, refining and replacing animal use during
the process of designing a preclinical development program. Such opportunities
might include (Ref. 11):
a. Reduction by use of a single species, by use of a single study to gather
both pharmacological and toxicological data whenever practical (refer to
sections III.B.2 through 5 of this document), and by use of non-terminal
10
ICCVAM Authorization Act of 2000. See 9 CFR Part 2, Animal Welfare Act. Additional information on the
federal government’s implementations of the principles of the 3Rs may be found at the Interagency Coordinating
Committee on the Validation of Alternative Methods (ICCVAM) website at http://iccvam.niehs.nih.gov
.
13

Contains Nonbinding Recommendations
evaluations instead of multiple cohorts of animals with terminal endpoints,
when justified.
b. Refinements such as incorporation of pain management and humane
endpoints, and the use of non-terminal imaging modalities.
c. Replacement of selected animal studies with in vitro studies, if such
alternatives exist or can be developed.
The suitability of these efforts should be considered with respect to their effect, if
any, on the ability of the preclinical testing program to provide necessary data
regarding the safety and activity of the CGT product.
9. Product Development for Later-Phase Clinical Trials
As development of an investigational CGT product progresses to later-phase
clinical trials, consideration should be given to the conduct of additional
preclinical studies to address any outstanding issues. For example, if
manufacturing/formulation changes occur such that the comparability of the later-
phase CGT product to the product used in early-phase clinical trial(s) is uncertain,
additional in vitro and/or in vivo preclinical studies may be needed to bridge the
two products. Such bridging studies allow data collected with the early-phase
product to support later-phase development or licensure. Additional preclinical
studies may be necessary if the dosing regimen or patient population changes
significantly from the early-phase clinical trials. In addition, the potential for
reproductive/developmental toxicity may need to be addressed, depending on
product type or target patient population. In general, such studies should be
conducted prior to Phase 3 clinical trials.
11
In contrast, due to the biological
attributes of the CGT products (e.g., stem cells and integrating viral vectors), the
conduct of studies to assess the carcinogenicity/tumorigenicity potential generally
occurs during the early stages of product development (Refs. 12 and 13).
Consultation with OCTGT throughout the CGT product development program is
recommended to ensure that the timing and design of any additional preclinical
studies are adequate to allow for seamless product development.
10. Preclinical Study Reports
A report must be submitted for each in vitro and in vivo preclinical study intended
to demonstrate the safety of an investigational CGT product
(21 CFR 312.23(a)(8)). Although complete reports for pharmacology/POC
studies are not required, sufficient information from these studies should be
11
Although CGT products fall outside the scope of the ICH guidance entitled “Guidance for Industry: M3(R2)
Nonclinical Safety Studies for the Conduct of Human Clinical Trials and Marketing Authorization for
Pharmaceuticals” dated January 2010, it may be useful to consider the recommendations as to the timing of
reproduction/developmental toxicity studies set forth in the ICH M3(R(2). Available at
http://www.fda.gov/Drugs/GuidanceComplianceRegu
latoryInformation/Guidances/ucm065006.htm.
14

Contains Nonbinding Recommendations
provided to allow for independent interpretation of the study results. Each
complete study report should include, but is not limited to: a) a prospectively
designed protocol and listing of all protocol amendments; b) a detailed description
of the study design (e.g., the test system used, animal species/model used, control
and investigational products administered, dose levels, detailed procedures for
product administration and collection of all study protocol parameters); c)
complete data sets for all parameters evaluated, including individual animal data
and tabulated/summary data; and d) analysis and interpretation of the results
obtained.
11. Communication with OCTGT Pharmacology/Toxicology Staff
We recommend communication with OCTGT Pharmacology/Toxicology staff
early in the investigational CGT product development program. Useful general
information can be gained from FDA guidances and presentations at scientific
meetings. However, preclinical testing programs for CGT products often need to
be highly individualized; therefore, a sponsor may need discussions with OCTGT
regarding CBER expectations for the specific product and indication. Such
advice can be obtained initially through a pre-pre-IND interaction,
12
which is a
non-binding, informal, targeted scientific and regulatory discussion between
reviewers from the Pharmacology/Toxicology Branch, other applicable reviewers,
and the sponsor at an early stage of product development. The advice given by
OCTGT in this interaction should be considered when preparing final protocols
for definitive preclinical studies, as well as in preparing various sections of the
briefing document for the pre-IND meeting.
13
IV. RECOMMENDATIONS FOR INVESTIGATIONAL CELL THERAPY (CT)
PRODUCTS
A. Introduction
CT products vary with respect to characteristics such as formulation (including
combination with a scaffold or other non-cellular component), the genetic relationship of
the cells to the patient (autologous, allogeneic, xenogeneic), and the cell source. CT
products can be generally classified as: stem cell-derived CT products; or mature/
functionally differentiated cell-derived CT products. If the CT product is derived from an
induced pluripotent stem cell (iPSC), the product has the possibility of expressing
characteristics of both stem cell-derived and mature/functionally differentiated cell-
derived products; therefore, both fundamental source categories of CT products should be
12
FDA Vaccines, Blood & Biologics: OCTGT Learn. Available at
http://www.fda.gov/BiologicsBloodVacci
nes/NewsEvents/ucm232821.htm.
13
See SOPP 8101.1 – “Scheduling and Conduct of Regulatory Review Meetings with Sponsors and Applicants”
found at
http://www.fda.gov/BiologicsBloodVacci
nes/GuidanceComplianceRegulatoryInformation/ProceduresSOPPs/ucm07
9448.htm.
15
Contains Nonbinding Recommendations
considered during the product development process. The in vivo biological activity and
safety profile of the investigational CT product is influenced by product origin (donor
source, tissue source), as well as the level of manipulation and stage of differentiation at
the time of administration. Regardless of the type of CT product, if the cells originate
from animal tissue or cells (xenotransplantation products), additional considerations
apply (Refs. 5 and 14).
1. Tissue sources of stem cells include: a) adult (e.g., hematopoietic, neural,
mesenchymal, cardiac, adipose, skin); b) perinatal (e.g., placental, umbilical
cord blood); c) fetal (e.g., amniotic fluid, neural); and d) embryonic. Stem
cell-derived products are characterized by a variable capacity for self-
renewing replication through cycles of cell division and the capacity for
differentiation into a variety of cell types with specialized
properties/functions. Such differentiation and replication are primarily
controlled by the physiologic milieu of the host in which the cells reside
following in vivo administration (Ref. 15). Similarly, contamination of a
differentiated CT product with undifferentiated stem cells or incompletely
differentiated progenitor/precursor cells poses potential safety concerns. For
additional discussion of this safety issue, please refer to the FDA briefing
document and transcript of the April 2008 Cellular, Tissue and Gene
Therapies Advisory Committee meeting to discuss safety concerns for the
development of CT products derived from human embryonic stem cells (Ref.
12).
2. Functionally differentiated tissue-derived CT products may be obtained from
adult human donors (autologous or allogeneic) or from animal sources
(xenogeneic). Source cells can include chondrocytes, pancreatic islet cells,
hepatocytes, neuronal cells, and various immune cells. CT products derived
from functionally mature tissues typically do not possess the property of self-
renewing proliferation and the capacity to differentiate into multiple cell
types; however, they may retain some cellular characteristics of their tissue of
origin. Additionally, their characteristics may change after in vivo
administration, based on specific extracellular cues.
B. Animal Species/Model(s)
For a general discussion regarding the selection of biologically relevant animal species
and animal models of disease/injury, refer to sections III.B.2 and 3 of this document.
Additional considerations for CT products can include:
1. The ability to access the anatomic site for product administration.
2. The ability to deliver a specific absolute cell dose to the target site.
3. The availability of immunodeficient animals, which may allow for long-term
assessment of the safety of the human CT product.
16

Contains Nonbinding Recommendations
Administration of human cells into animals is complicated by the immunogenic
responses of healthy immune-competent animals, potentially resulting in the rejection of
the administered human cells. This response may prevent adequate evaluation of the
activity and safety of the human cellular product. When conducting preclinical studies to
evaluate the activity and safety of a human cellular product, the cross-species
immunogenicity may necessitate alteration of the animal model in order to create an in
vivo immune tolerant niche for the administered human cells. Various models that have
been considered include:
Immunosuppressive agents in immune-competent animals;
Genetically immunodeficient animals;
Humanized animals;
14
Administration into an immune privileged site; or
A combination of these scenarios.
The administration of analogous cellular products in the preclinical studies is also a
potentially acceptable option. The scientific value of this approach is optimized when the
analogous CT product is substantially similar to the human CT product. However,
preclinical testing using an analogous cellular product can introduce uncertainty
regarding the relevance of the data due to potentially different biological activities,
molecular regulatory mechanisms, and impurities/contaminants. Therefore, if this
preclinical testing pathway is used, the level of analogy of the animal cellular product
with the intended human cellular product should be characterized. Examples may
include:
Established procedures for tissue/sample harvest.
Cell identification, isolation, expansion, and in vitro culture procedures.
Cell growth kinetics (e.g., cell doubling time, cell growth curve, and time
to cell proliferation plateau).
Phenotype and functional properties (e.g., secretion of growth factors and
cytokines, cell population-specific phenotypic/genotypic markers).
Final product formulation/cell-scaffold seeding procedures (as applicable).
Final product storage conditions and cell viability.
14
For purposes of this guidance, the term “humanized animals” refers to animals carrying functional human genes,
cells, tissues, and/or organs, used in biological research for human therapeutics.
17
Contains Nonbinding Recommendations
The degree of similarity of these parameters for the analogous CT product should be as
close to the proposed human CT product as possible in an attempt to maximize the
applicability of data derived from the animal studies.
FDA has held advisory committee meetings that discussed the selection of appropriate
animal models for human-derived CT products intended to treat clinical conditions such
as Type 1 diabetes (Ref. 16), cardiac disease (Ref. 17), and cartilage repair (Ref. 18).
Additionally, an FDA advisory committee discussed relevant preclinical animal models
for the testing for safety and activity of xenotransplantation products intended to treat
acute liver failure and Type 1 diabetes mellitus (Ref. 19).
C. Study Designs
In addition to the general guidance on the preclinical testing program provided in section
III.B. of this document, considerations when designing preclinical studies for
investigational CT products include the following:
1. The targeted cellular phenotype(s).
2. The source of the cell(s).
3. The extent of ex vivo manipulation performed (e.g., selection, purification,
expansion, activation).
4. The fate of the cells post-administration (engraftment, migration,
differentiation, tumorigenicity (see section IV.D. of this document)).
5. The probability of a host immune response to the administered cells.
6. Administration site reactions.
7. Potential inflammatory response in target and/or non-target tissues.
8. Unregulated/dysregulated proliferation of the cells within the host.
An FDA advisory committee discussed many of these safety issues in the context of
pluripotent stem cells (Ref. 12). Some of these concerns are discussed in more detail
below.
D. CT Product Fate Post-Administration
Determination of the fate of the investigational CT product following administration in
animals is an important contribution to characterizing the product activity and safety
profile. When conducted early in the preclinical testing program, assessment of cell fate
can help characterize the putative MOA by determining if engraftment is important and
18
Contains Nonbinding Recommendations
necessary to achieve the desired pharmacological response. Additionally, cell fate can
help justify the selection of the animal species/models, justify the duration of the
definitive studies, and identify potential target organs of toxicity.
Considerations of cell fate in vivo include:
1. Survival/Engraftment
Cell viability and subsequent engraftment may be affected by:
a. The biocompatibility of the cell delivery device and the CT product
(considerations include cell shearing, adsorption onto the walls of the
catheter/syringe).
b. The ROA.
c. The genetic relationship of the cells to the host animal (autologous/
syngeneic, allogeneic, or xenogeneic).
d. The immune status of the host animal.
e. The timing of cell administration relative to the onset of the disease/injury
(i.e., the pathophysiologic status of the microenvironment).
If long-term cell survival/engraftment is necessary to achieve effectiveness of the
CT product, the animals should be followed for an interval sufficient to allow for
comprehensive evaluation of in vivo cell survival, anatomic engraftment, and
biologic activity.
2. Distribution
As a consequence of their biologic attributes, CT products administered in vivo
are not subject to conventional chemical analyses; therefore, standard ADME and
pharmacokinetic testing techniques and profiles are not applicable. Although
influenced by specifics of the CT product and its ROA, cells have an inherent
potential to distribute to sites other than to the target organ/tissue. Various
methods, such as imaging modalities used for detection of radioisotope-labeled
cells, genetically modified cells (e.g., expressing green fluorescent protein),
nanoparticle-labeled cells (e.g., iron-dextran nanoparticles), or the use of
polymerase chain reaction (PCR) analysis and immunohistochemistry to identify
cells of human origin or cells of a karyotype different than the host (e.g., gender),
have been used to assess distribution. A potential advantage of in vivo imaging
techniques is that in many instances, the same animal can be evaluated over time,
thus decreasing variability and reducing the number of animals used. Data should
be provided to support the viability and function of the CT product if the cells are
modified to enable use of such imaging techniques.
19
Contains Nonbinding Recommendations
3. Differentiation and Integration
Cellular differentiation capacity, the plasticity of phenotypic expression
attributable to transdifferentiation or fusion with other cell types, as well as
structural and functional tissue integration, may all be influenced by physiologic
factors within either the local microenvironment into which the CT product is
administered or the final location/niche in which the cells ultimately reside.
Therefore, conditions found within the local microenvironment into which the
cells are placed are likely to have an impact on the safety and/or bioactivity of the
CT product. Given the biological attributes of some CT products, the potential
for ectopic expression in target and non-target tissues also exists. Depending on
their differentiation status and the extent of manipulation the cells undergo prior
to in vivo administration, parameters such as cell morphology, phenotype, and
level of differentiation following in vivo administration should be assessed in the
animal studies.
4. Tumorigenicity
The potential for tumorigenicity, dysplasia, or hyperplasia to occur should be
considered and addressed as appropriate for the specific biologic properties of
each investigational CT product. Factors that may influence the tumorigenicity
assessment include:
a. The differentiation status profile of cell types within the CT product
(ranging from undifferentiated/embryonic to terminally
differentiated/specialized).
b. The extent of cell manipulation employed during manufacture of the
product and the resulting growth kinetic profile (e.g., minimal, culture
expansion only, culture expansion with/without growth factors, ex vivo
differentiation, ex vivo transduction with or without cell expansion).
c. The expressed transgene (e.g., various growth factors) of genetically
modified cells.
d. The potential to induce or enhance tumor formation from existing sub-
clinical host malignant cells.
e. The target patient population.
Studies conducted in animals to assess tumorigenicity should use the intended
clinical product, not analogous animal cells. There is currently no scientific
consensus regarding the selection of the most relevant animal models to evaluate
tumorigenic potential or the ability of current animal models to predict clinical
outcome. However, it is important that animal studies designed to assess this
endpoint for CT products show in vivo survival of the cells for a sufficient length
20

Contains Nonbinding Recommendations
of time to allow for potential tumor formation (Ref. 12).
15
Additional study
design considerations include: 1) appropriate control groups (e.g.,
undifferentiated cells, partially differentiated cells, positive controls, vehicle
controls); 2) adequate numbers of animals per group to ensure statistical
significance of any biological observations, including any background incidence
of tumor formation; 3) inclusion of at least one dose level that constitutes the
maximum absolute amount of cells that can be administered; 4) delivery of the
CT product targeting the planned clinical anatomic site; and 5) sufficient study
duration.
E. CT Products with Implantable Scaffolds
In addition to the considerations presented in sections IV.B through D of this document,
overall preclinical study designs for these combination products should take into account
the following:
1. Cells
Similar to all CT products, cell characterization should be provided prior to
scaffold seeding to support use of the CT component (Ref. 8).
2. Scaffolds
Any scaffold construct (synthetic or non-synthetic polymers) used should be
identical in composition to the intended clinical scaffold. The scaffold should be
adequately characterized for composition, degradation profile, biomechanical
performance, and biocompatibility (with respect to host response to the scaffold
component and to the cell component of the product). The specific tests that are
needed to sufficiently characterize a scaffold are determined by its composition
and intended use. The specific testing expectations for scaffold materials will
share some features similar to the testing expected if the scaffold were to be used
as an implant alone. However, the details of the manufacturing process and the
cells used will likely influence the specific tests needed.
3. Biocompatibility
Depending on the material(s) that constitute the intended clinical product,
biocompatibility testing may be warranted. Biocompatibility test results in
accordance with the Blue Book Memorandum #G95-1 “Use of International
Standard ISO-10993, Biological Evaluation of Medical Devices Part-1:
Evaluation and Testing,” (Ref. 10) should be consulted for approaches to
biocompatibility testing. In addition, ASTM F748-04, “Standard Practice for
Selecting Generic Biological Test Methods for Materials and Devices” may also
15
For purposes of this guidance, a “sufficient length of time” means the period of time within which one would
reasonably expect to detect a signal in a particular in vivo testing system.
21

Contains Nonbinding Recommendations
be an acceptable approach for conducting biocompatibility testing.
16
A complete
test report describing the tests performed, the specific methods utilized, and the
results should be included in the regulatory submission.
4. Cell Seeding
The same cell seeding procedure/seeding density as proposed clinically should be
used for the CT product administered to the animals.
5. Study Groups
Groups should consist of animals administered the intended clinical product (i.e.,
scaffold seeded at varying cell densities) and appropriate controls.
6. Biological Responsiveness
Safety and POC of the administered product and product components should be
demonstrated via inclusion of biochemical, morphological (i.e., composition and
architecture of the tissue), and functional endpoints. Functional endpoints may
include mechanical testing, which will depend on product design, product
components, the method/location of product administration, putative MOA, and
disease indication. The mechanical properties of the repaired, replaced, or
regenerated tissue should be compared to appropriate concurrent controls. FDA’s
guidance document entitled “Guidance for Industry: Preparation of IDEs and
INDs for Products Intended to Repair or Replace Knee Articular Cartilage” dated
December 2011 (Ref. 2) offers recommendations on mechanical testing that may
be applied to some cell/scaffold products.
7. Dose Response and Durability of the Response
The optimal dose and length of time needed to assess repair, replacement, or
regeneration of clinical lesions (i.e., construct performance) and the durability of
the effect should be determined. In addition, the biodegradation profile of the
scaffold construct should be evaluated. The study duration will vary based on the
product and the clinical indication, but should be sufficient to provide data to
show durability of effect. For example, study duration of one year in a relevant
animal injury model is recommended for determination of product performance
and assessment of durability for products intended for repair/replacement of knee
cartilage (Ref. 2).
16
The referenced document is an American Society for Testing and Materials Standard (ASTM). The standard is
available at http://www.astm.org
, or contact ASTM Customer Service at se[email protected].
22

Contains Nonbinding Recommendations
8. Safety
Local toxicities (e.g., tumorigenicity, altered tissue function at the injection site,
inappropriate cellular differentiation, or inflammatory infiltrates) may be due to
interactions of the product components with the tissue or to the degradation of
product components at the site of administration. Cell migration outside of the
target tissue may lead to systemic toxicities, such as ectopic tissue formation and
tumorigenicity. The immunogenic potential of the construct (i.e., the scaffold
and/or the cells) could also cause toxicity. Both acute and long-term in vivo
safety of the product should be evaluated.
V. RECOMMENDATIONS FOR INVESTIGATIONAL GENE THERAPY (GT)
PRODUCTS
A. Introduction
As a general matter, OCTGT reviews the following GT products:
1. Non-viral vectors (e.g., plasmids).
2. Replication-deficient viral vectors (e.g., adenovirus, adeno-associated virus
(AAV), retrovirus, lentivirus, poxvirus, herpes simplex virus (HSV)).
3. Replication-competent oncolytic vectors (e.g., measles, reovirus, adenovirus,
vesicular stomatitis virus, vaccinia).
17
4. Microbial vectors used for gene therapy (e.g., Listeria, Salmonella, E. coli,
Bacteriophage).
5. Ex vivo genetically modified cells.
B. Animal Species/Model(s)
For a general discussion regarding the selection of biologically relevant animal species
and animal models of disease/injury, refer to sections III.B.2 and 3 of this document.
Specific considerations for the selection of relevant animal species/model for
investigational GT products include:
1. Assessment of the permissiveness/susceptibility of various animal species to
infection by, and replication of, the viral vector.
17
Oncolytic vectors are oncolytic viruses that have been genetically modified to carry an exogenous therapeutic
gene. Oncolytic viruses which are not so modified are not gene therapies, and are therefore beyond the scope of this
guidance. Considerations related to preclinical assessment of these oncolytic viruses may resemble those for GT
products derived from similar viral sources. Sponsors of oncolytic virus products should consult the OCTGT
Pharmacology/Toxicology staff for product specific recommendations.
23
Contains Nonbinding Recommendations
2. Pharmacological response of the species to the expressed transgene.
3. Sensitivity of the species to the biological actions of the ex vivo genetically
modified cells.
If the above parameters relevant to a specific GT product cannot be met using common
laboratory animal species, modifications should be considered. For example, genetically
modified animals expressing the human receptor target have been used to characterize the
biologic activity, and thus the potential pathology, of some viruses. Similarly,
immunodeficient animals have been used to evaluate the safety of genetically modified
human cells. In instances where the expressed transgene is not biologically active in the
animal species, use of the clinical vector expressing an analogous transgene that is active
in the laboratory species may suffice, especially if clinical or preclinical data for the
expressed protein exist. In such instances, comparison of the intended clinical product
and the animal analogue should be provided (e.g., sequence, target specificity, expression
levels).
C. Study Designs
In addition to the general guidance on the preclinical testing program provided in section
III.B. of this document, safety concerns for both ex vivo and in vivo administration of an
investigational GT product derive from multiple factors, such as: the potential for
adverse immune responses to the ex vivo genetically modified cells, the vector, or the
expressed transgene; vector and transgene toxicities; and the potential risks of the
delivery procedure. For example, administration of genetically modified cells or vector
to vital organs, such as the brain or heart, generate concerns for potential toxicity from
the product itself, as well as for possible risks associated with the delivery device and the
delivery procedure. These issues should be addressed in the preclinical testing program
before initiation of clinical trials.
1. Overall Safety Considerations
Although assessment of the safety of the in vivo administered vector depends on
the biological properties of each vector type, concerns that should be addressed
include:
a. Toxicities due to the components of the final formulation (e.g., liposomes
and various excipients/contaminants).
b. Toxicities due to the ROA used.
c. Aberrant localization to non-target cells/tissues.
d. Level and persistence of vector and expressed transgene.
24
Contains Nonbinding Recommendations
e. Level of viral replication in non-target cells/tissues.
f. Immune activation or suppression.
g. Immune response directed against the vector.
h. Phenotype/activation state of target cell(s).
i. Potential for insertional mutagenesis or oncogenicity.
j. Potential for germline transmission.
k. Potential horizontal transmission of replication competent vectors from the
patient to family members and health care providers (i.e., shedding).
2. Vector-Specific Considerations
Some examples of potential toxicities characteristic of specific vector types
include:
a. Non-viral vectors - potential for immune response to the DNA or to
extraneous bacterial sequences.
b. Replication-deficient viral vectors:
i. Adenovirus - potential for a significant immune response and
inflammatory response to the vector and possible adverse effects
from any contaminating replication-competent adenovirus.
ii. Adeno-Associated Virus (AAV) - 1) although AAV remains
episomal in the transduced cell, the potential for random integration
into host DNA, resulting in insertional mutagenesis and any
subsequent adverse biological effects exists, and 2) potential immune
response to the capsid proteins.
iii. Retrovirus and Lentivirus - 1) production of a replication-competent
retrovirus/lentivirus (RCR/RCL) during manufacturing, 2) potential
for insertional mutagenesis, resulting in oncogene activation, 3)
potential for germline integration, and 4) potential for altered
expression of host genes.
iv. Poxvirus - 1) ability to infect and replicate in many types of human
tissues and cells, 2) potential for toxicity in immune-compromised
populations such as cancer patients, and 3) renal/cardiac concerns.
25
Contains Nonbinding Recommendations
v. Herpes Simplex Virus (HSV) - tropism to the central nervous system
and the potential for latency and reactivation.
c. Replication-competent oncolytic vectors - 1) potential viral infection and
replication in normal cells, and 2) increased viral spread and replication in
non-target tissues in immune-suppressed patients or when administered in
combination with radiation, chemotherapy, prodrugs, or other agents.
d. Microbial vectors used for gene therapy - 1) lack of adequate attenuation
of the microbe, 2) ability to replicate in non-target tissues, 3) excessive
induction of proinflammatory cytokines, and 4) lack of antibiotic
susceptibility.
Although the appropriate duration of clinical follow-up of GT trial participants for
adverse events is primarily a trial design issue, vector characteristics and
preclinical data are used to inform clinical trial decisions. CBER has issued a
guidance for industry entitled “Guidance for Industry: Gene Therapy Clinical
Trials - Observing Subjects for Delayed Adverse Events” dated November 2006
(2006 Guidance) (Ref. 6), that discusses the potential risks of delayed adverse
events following exposure to GT products as a consequence of persistent
biological activity of the genetic material or other components of the products
used to carry the genetic material. As specified in that guidance, factors that are
likely to increase the risk of delayed adverse events in humans include persistence
of the viral vector, integration of genetic material into the host genome, prolonged
expression of the transgene, and altered expression of the host’s genes. The 2006
Guidance should be consulted and, if found to be applicable to the investigational
GT product under study, should be used to guide the design of relevant preclinical
studies to address potential long-term safety issues that may result from
administration to humans.
3. Transgene Considerations
When determining the safety of an expressed transgene and/or translated protein,
sponsors should consider the following: a) local versus systemic expression; b)
level and duration of expression; and c) acute versus chronic effects. While
persistent transgene expression may be a desired endpoint for some GT products,
it can also be an undesired outcome for other products due to overexpression,
accumulation of transgene protein, or the risk of an abnormal immune response.
Prolonged expression of transgenes such as growth factors, growth factor
receptors, or immunomodulating agents, may be associated with long-term risks
due to unregulated cell growth, malignant transformation, autoimmune reactions
to self-antigens, altered expression of the host’s genes, or other unanticipated
adverse effects (Refs. 6 and 20). The conduct of long-term preclinical studies
should be considered to evaluate these concerns.
26
Contains Nonbinding Recommendations
In addition, assessment of the in vivo transgene expression profile is
recommended for: vectors expressing a new transgene(s) with an unknown
potential to induce toxicity; or vectors expressing a transgene with a known or
suspected potential to induce toxicity if aberrantly expressed in non-target tissues.
Quantitation of transgene expression using methods such as a quantitative
Reverse Transcriptase PCR (RT-PCR) assay can help determine: the threshold
level of expression associated with beneficial or deleterious effects for specific
tissues/organ systems; and correlation of the kinetics of transgene expression with
desired activity or undesired toxicity profiles.
In addition, potential immunogenic/neutralization responses directed against the
expressed transgene and/or directed against self/endogenous proteins can be a
concern. For example, delivery of transgenes that encode various endogenous
enzymes, receptors or structural proteins may elicit antibodies against both the
transgene and against the endogenous components expressed in normal cells and
tissues, resulting in an adverse response. Similarly, transgenes that express fusion
or chimera proteins can theoretically be immunogenic due to their foreign
(xenogeneic) nature. These concerns should be addressed in the preclinical
testing program.
4. Ex vivo Genetically Modified Cells
The safety assessment of the cellular component of ex vivo transduced cells
includes endpoints that are similar to those evaluated for CT products, as noted in
sections IV.C and D of this document. The significance of the issues described in
these sections will depend on the cell type(s), the vector construct, and/or the
transgene used. The preclinical study designs should address relevant factors
specific to each product.
5. Biodistribution Considerations
The characterization of the vector biodistribution profile following in vivo
administration is an important component of the preclinical development program
for GT products. These data are used to determine the potential for vector
presence in desired target tissues/biological fluids (e.g., blood, cerebral spinal
fluid), in non-target tissues/biological fluids, and in the germline (Refs. 21 and
22). The characterization of the vector presence, persistence, and clearance
profile can inform the selection of the GT product dosing schedule, the
monitoring schedule for various activity/safety parameters, and the animal
sacrifice time points in the definitive preclinical studies. The biodistribution data,
coupled with other preclinical safety endpoints such as clinical pathology and
histopathology, help determine whether vector presence or gene expression
correlates with any tissue-specific detrimental effects in the animals.
27

Contains Nonbinding Recommendations
Prior to administration in humans, biodistribution studies should be considered
for:
a. Investigational GT products that belong to a new vector class.
b. Established vectors with significant changes in the vector backbone.
c. Established vectors with a significant formulation change.
d. Established vectors with a significant change in the ROA.
e. Established vectors with a significant change in the dosing schedule and/or
the vector dose levels.
Justification should be provided if biodistribution studies are not conducted prior
to initiation of early-phase clinical trials.
Tissue/biological fluid analysis should be conducted at the molecular level, using
a quantitative PCR (Q-PCR) assay to determine the number of vector copies per
microgram of genomic DNA at specified time points post-vector administration.
Depending on the ROA and biology of the investigational GT product (vector
type and expressed transgene), additional tissues (i.e., beyond the tissues listed in
section IV.B.2 of the FDA guidance entitled “Guidance for Industry: Gene
Therapy Clinical Trials - Observing Subjects for Delayed Adverse Events” dated
November 2006) may need to be collected and analyzed (Ref. 6). In addition, the
presence of a vector sequence in tissues/biological fluids may trigger further
analysis to determine the transgene expression levels.
VI. RECOMMENDATIONS FOR INVESTIGATIONAL THERAPEUTIC VACCINES
A. Introduction
Therapeutic vaccines are designed to mediate their therapeutic effect in vivo through
induction or modulation of the antigen-specific host immune response, targeted to an
extrinsic or intrinsic antigenic moiety, thereby ameliorating or treating a specific disease.
Prophylactic vaccines, in contrast, are designed for the prevention of disease, and these
vaccines are beyond the scope of this guidance.
18
For a discussion of preclinical
considerations specific for therapeutic cancer vaccines, refer to the FDA guidance
entitled “Guidance for Industry: Clinical Considerations for Therapeutic Cancer
Vaccines” dated October 2011 (Ref. 7). Therapeutic vaccines for non-oncology
18
As noted in section I of this document, OVRR reviews preventive (prophylactic) vaccines, as well as therapeutic
vaccines for infectious diseases.
28

Contains Nonbinding Recommendations
29
indications generally consist of a target peptide/protein containing the epitope of interest
(hapten), which may be combined with or conjugated to a carrier and is often co-mixed or
co-administered with an adjuvant.
19
These vaccines may be cell- or gene-based.
B. Animal Species/Model(s)
As discussed in sections III.B.2 and 3 of this document, the selection of the animal
species/ model depends on the putative MOA and the target specificity of the
investigational product. Ideally, the animal species should be responsive to the biological
effects of the vaccine, allowing for the assessment of potential biological activity in
conjunction with safety. In addition to the use of healthy animals, consider assessing the
safety of the therapeutic vaccine in models of disease/injury representative of the target
patient population, recognizing that the species/model may not mimic all immunological
aspects of that population. Justification, with supporting in vitro and/or in vivo data,
should be provided for the animal species and model(s) used.
C. Study Designs
The design of preclinical studies for investigational therapeutic vaccines should follow
the considerations presented in sections III.B.4 and 5 of this document. In addition,
parameters to evaluate immunological specificity, immune activity, and the potential for
immune toxicity should be included. Immune activity testing should include
characterization of the humoral and cellular response profile, with correlation of resulting
data with pharmacological and/or toxicological findings. To characterize the onset,
persistence, and extent of the systemic humoral and cellular immune response to the
vaccine, study designs should include the collection of samples over time from the same
animal.
20
VII. CONCLUSION
This guidance recommends both a general framework for planning a preclinical program
intended to support clinical trials of cellular and gene therapies, and more detailed
recommendations for considerations for designing preclinical studies specifically for
investigational CGT products. Although the technical recommendations provided in this
document and the opportunities for pre-submission interactions with OCTGT staff should
facilitate the design of appropriate preclinical studies to support use of the CGT products in
clinical trials, the adequacy of any specific preclinical study or program will depend on the
specific study design, subsequent implementation, and on the resulting data. Accordingly, it is
important to provide a comprehensive preclinical assessment in the IND submission.
19
For general principles regarding preclinical considerations for adjuvants in therapeutic vaccines, refer to the
European Medicines Agency “Guideline on Adjuvants in Vaccines for Human Use” dated January 2005 at:
www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003809.pdf
.
20
For general principles regarding preclinical study designs for therapeutic vaccines, refer to the World Health
Organization (WHO) document, “WHO Guidelines on Nonclinical Evaluation of Vaccines” dated November 2003
at: www.who.int/biologicals/publications/
nonclinical_evaluation_vaccines_nov_2003.pdf.
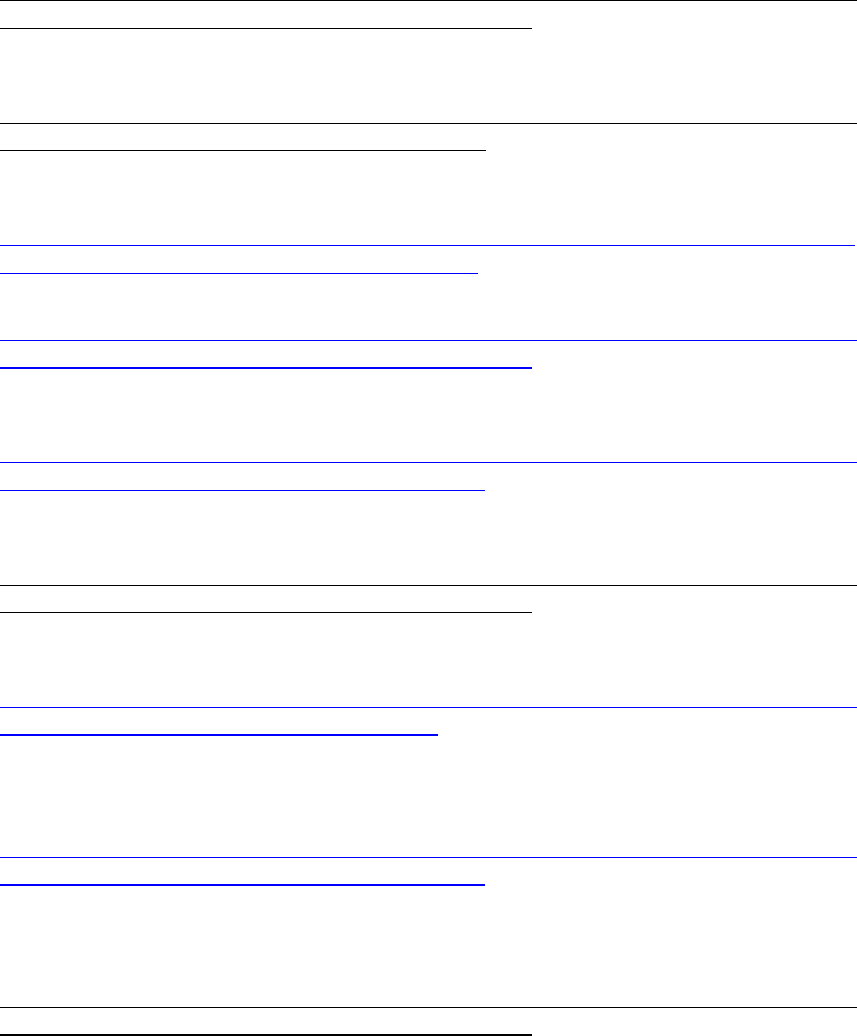
Contains Nonbinding Recommendations
VIII. REFERENCES
1. Guidance for Industry: Guidance for Human Somatic Cell Therapy and Gene Therapy;
March 1998,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/CellularandGeneTherapy/ucm072987.htm.
2. Guidance for Industry: Preparation of IDEs and INDs for Products Intended to Repair or
Replace Knee Articular Cartilage; December 2011,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/CellularandGeneTherapy/default.htm.
3. Guidance for Industry: Considerations for Allogeneic Pancreatic Islet Cell Products;
September 2009,
http://www.fda.gov/biologicsbloodvaccines/guidancecomplianceregulatoryinformation/g
uidances/cellularandgenetherapy/ucm182440.htm.
4. Guidance for Industry: Cellular Therapy for Cardiac Disease; October 2010,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/CellularandGeneTherapy/ucm164265.htm.
5. Guidance for Industry: Source, Animal, Product, Preclinical, and Clinical Issues
Concerning the Use of Xenotransplantation Products in Humans; April 2003,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/Xenotransplantation/ucm074354.htm.
6. Guidance for Industry: Gene Therapy Clinical Trials - Observing Subjects for Delayed
Adverse Events; November 2006,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/CellularandGeneTherapy/ucm072957.htm.
7. Guidance for Industry: Clinical Considerations for Therapeutic Cancer Vaccines;
October 2011,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/Xenotransplantation/default.htm.
8. Guidance for FDA Reviewers and Sponsors: Content and Review of Chemistry,
Manufacturing, and Control (CMC) Information for Human Somatic Cell Therapy
Investigational New Drug Applications (INDs); April 2008,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/Xenotransplantation/ucm074131.htm.
9. Guidance for FDA Reviewers and Sponsors: Content and Review of Chemistry,
Manufacturing, and Control (CMC) Information for Human Gene Therapy
Investigational New Drug Applications (INDs); April 2008,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/CellularandGeneTherapy/ucm072587.htm.
10. CDRH Blue Book Memo #G95-1: Use of International Standard ISO-10993, 'Biological
Evaluation of Medical Devices Part 1: Evaluation and Testing' (Replaces #G87-1
#8294); May 1995,
30

Contains Nonbinding Recommendations
http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocument
s/ucm080735.htm.
11. R. Robinson, Three Rs of animal testing for regenerative medicine products. Sci. Transl.
Med. 3:112:112fs11 (2011).
12. Cellular, Tissue and Gene Therapies Advisory Committee (CTGTAC) Meeting #45;
April 10-11, 2008 - Cellular Therapies Derived from Human Embryonic Stem Cells -
Considerations for Pre-Clinical Safety Testing and Patient Monitoring,
http://www.fda.gov/ohrms/dockets/ac/08/minutes/2008-0471M.htm.
13. Biological Response Modifiers Advisory Committee (BRMAC) Meeting #38; March 4,
2005 – Update on Retroviral Vector-Mediated Insertional Tumorigenesis,
http://www.fda.gov/ohrms/dockets/ac/cber05.html#CellularTissueGeneTherapeis.
14. PHS Guideline on Infectious Disease Issues in Xenotransplantation; January 2001,
http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformatio
n/Guidances/Xenotransplantation/ucm074727.htm.
15. Fink DW and SR Bauer. “Stem Cell-Based Therapies: Food and Drug Administration
Product and Pre-Clinical Regulatory Considerations”. In The Essentials of Stem Cell
Biology (Second Edition). R Lanza, J Gearhart, B Hogan, D Melton, R Pedersen, J
Thomson, E Thomas, I Wilmut (Eds.); Elsevier Academic Press: Burlington, MA, 2009.
16. Biological Response Modifiers Advisory Committee (BRMAC) Meeting #36; October 9-
10, 2003 – Allogeneic Pancreatic Islets for Type 1 Diabetes,
http://www.fda.gov/ohrms/dockets/ac/cber03.html#BiologicalResponseModifiers.
17. Biological Response Modifiers Advisory Committee (BRMAC) Meeting #37; March 18-
19, 2004 – Cellular Products for the Treatment of Cardiac Disease,
http://www.fda.gov/ohrms/dockets/ac/cber04.html#BiologicalResponseModifiers.
18. Cellular, Tissue and Gene Therapies Advisory Committee (CTGTAC) Meeting #38;
March 3-4, 2005 – Cellular Products for Joint Surface Repair,
http://www.fda.gov/ohrms/dockets/ac/cber05.html#CellularTissueGeneTherapeis.
19. Cellular, Tissue and Gene Therapies Advisory Committee (CTGTAC) Meeting #47; May
14, 2009 – Animal Models for Xenotransplantation Products Intended to Treat Diabetes
or Liver Failure, http://www.fda.gov/AdvisoryCommittees/CommitteesMeetingMaterials/
BloodVaccinesandOtherBiologics/CellularTissueandGeneTherapiesAdvisoryCommittee/
ucm129403.htm.
20. Serabian, M. and Y. Huang. Preclinical Safety Evaluation of Gene Therapy Products; in
‘Preclinical Safety Evaluation of Biopharmaceuticals - A Science-Based Approach to
Facilitating Clinical Trials’, Ed. Cavagnaro JA. Wiley Publishing, 2008.
21. ICH Considerations: General Principles to Address the Risk of Inadvertent Germline
Integration of Gene Therapy Vectors; October 2006,
http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Consideration_documents/
GTDG_Considerations_Documents/ICH_Considerations_General_Principles_Risk_of_I
GI_GT_Vectors.pdf.
31

