
Burden of Diabetes in California
California Department of Public Health
Chronic Disease Control Branch
June 2019

i
This publication was prepared in May 2019 by the Chronic Disease Control Branch. This report
is an update of the Burden of Diabetes in California 2014 and 2009 reports. All content in this
document is in the public domain and may be reproduced with the following citation:
Taylor CW, Downie C, Mercado V. (2019). Burden of Diabetes in California. California
Department of Public Health. Sacramento, California.
Inquiries regarding the content of this report may be directed to:
Dr. Catrina Taylor, PhD, MSPH
Senior Epidemiologist/Biostatistician
Health Information and Statistics Section
Chronic Disease Control Branch
California Department of Public Health
MS 7208, P.O. Box 997377
Sacramento, CA 95899-7377
(916) 552-9900
CDCBAdministrati[email protected]
This publication was supported by Grant/Cooperative Agreement Number NU58DP006540-01-
00 (1815 Prevention Forward grant, CDC-RFA-DP18-1815) from the Centers for Disease
Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do
not necessarily represent the official view of the CDC.
© 2019 California Department of Public Health,
Center for Healthy Communities,
Chronic Disease Control Branch

ii
TABLE OF CONTENTS
Table of Figures ................................................................................................................. iv
Message from the Chronic Disease Control Branch Chief ............................................... vi
I. Introduction....................................................................................................................... 1
II. Diabetes Definitions ........................................................................................................ 1
III. Data Sources ................................................................................................................. 2
IV. Burden of Diabetes and Prediabetes in California ....................................................... 3
Prevalence of Diabetes ................................................................................................... 3
Estimated Prevalence of Type 2 Diabetes by County in California ............................... 4
Prevalence of Prediabetes .............................................................................................. 5
Estimated Prevalence of Prediabetes by County in California ....................................... 6
Prevalence of Gestational Diabetes ................................................................................ 7
Prevalence of Diabetes, Prediabetes, and Type 2 Diabetes Among
California Adults by Selected Socio-Demographic Characteristics ............................... 8
Prevalence of Diabetes, Prediabetes, and Type 2 Diabetes
by Selected Risk Factors ............................................................................................... 10
Summary of Diabetes Burden in California ................................................................... 11
V. Diabetes Comorbidities ................................................................................................ 12
Summary of Diabetes Comorbidities ............................................................................ 16
VI. Diabetes Complications and Healthcare Use ............................................................. 17
End Stage Renal Disease (ESRD)................................................................................ 17
Ophthalmic Complications ............................................................................................. 18
Lower Extremity Amputations........................................................................................ 19
Healthcare Use .............................................................................................................. 20
Financial Cost of Diabetes and its Complications ........................................................ 23
VII. Diabetes Mortality ....................................................................................................... 24
CDPH ............................................................................................................................. 26
Community-Related Diabetes Activities ........................................................................ 28
Diabetes-Related Policies in California ......................................................................... 28
IX. Conclusions ................................................................................................................. 28
Appendix............................................................................................................................ 29
Data Sources ................................................................................................................. 29
CHIS ........................................................................................................................... 29
California BRFSS ....................................................................................................... 31

iii
CDC WONDER Database ......................................................................................... 32
California Vital Statistics Data .................................................................................... 32
OSHPD Patient Discharge Data ................................................................................ 32
California Department of Finance Population Data ................................................... 33
United States Census Bureau California Population Data ........................................ 33
Statistical Methods......................................................................................................... 33
Age Adjustment .......................................................................................................... 33
Confidence Intervals .................................................................................................. 33
Unstable Estimates .................................................................................................... 33
Supplementary Data ...................................................................................................... 34
References ........................................................................................................................ 36

iv
TABLE OF FIGURES
Figure 1. Estimated prevalence of diabetes among those with or
without a previous prediabetes diagnosis, 2013-2017 ................................... 3
Figure 2. Estimated age-adjusted prevalence of type 2 diabetes in
California by county, 2017 ............................................................................... 4
Figure 3. Estimated prevalence of prediabetes among those
with and without a subsequent diabetes diagnosis, 2013-2017..................... 5
Figure 4. Estimated age-adjusted prevalence of prediabetes
in California by county, 2017 ........................................................................... 6
Figure 5. Estimated prevalence of resident California women hospitalized for
labor and delivery with gestational diabetes mellitus, 2005-2014 .................. 7
Figure 6. Estimated prevalence of diabetes, prediabetes, and type 2 diabetes
among California adults by age, race/ethnicity, and gender, 2013-2017 ...... 8
Figure 7. Estimated prevalence of diabetes, prediabetes, and type 2 diabetes among
California adults by education and federal poverty levels, 2013-2017 .......... 9
Figure 8. Estimated prevalence of diabetes, prediabetes, and type 2
diabetes by body mass index and cigarette smoking status, 2013-2017 .... 10
Figure 9. Estimated prevalence of hypertension, cardiovascular disease,
high cholesterol, and arthritis among California adults with
diabetes, prediabetes, and without diabetes, 2013-2017 ............................. 12
Table 1. Estimated prevalence of other chronic conditions among California
adult population with diabetes, prediabetes, and without diabetes,
by age, gender, and race/ethnicity, 2013-2017 ............................................ 14
Table 2. Estimated prevalence of insurance coverage among California
adult population with diabetes, prediabetes, and without diabetes,
by age, gender, and race/ethnicity, 2013-2017 ............................................ 15
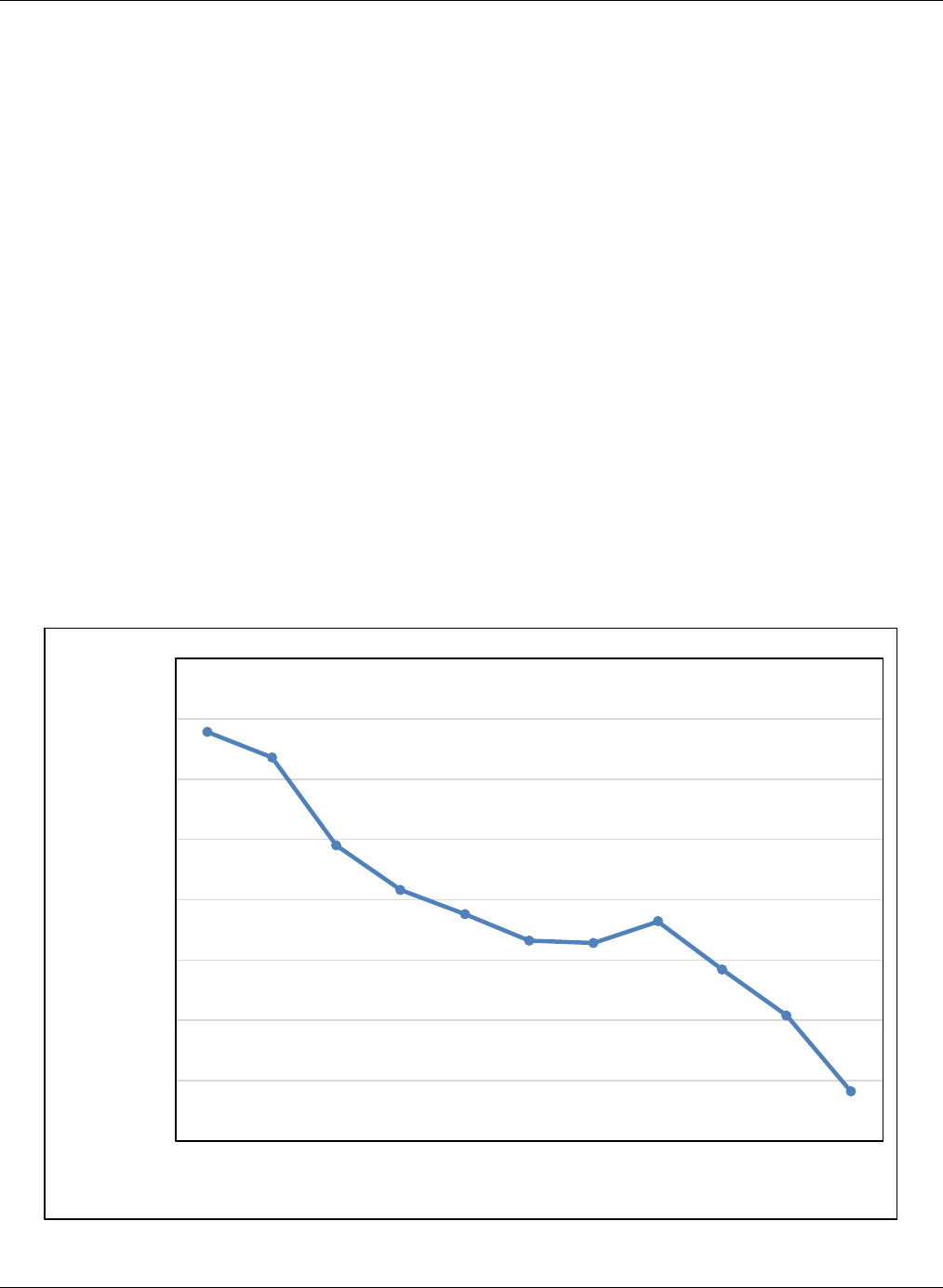
Figure 10. Estimated prevalence of diabetes-related ESRD per 100,000
adult diabetes hospitalizations, 2006-2016................................................... 17
Figure 11. Estimated prevalence of diabetes-related ophthalmic hospitalizations
per 100,000 adult diabetes hospitalizations, 2006-2016 .............................. 18
Figure 12. Estimated prevalence of diabetes-related lower extremity
amputations per 100,000 diabetes hospitalizations, 2006-2016 .................. 19
Table 3. Estimated prevalence of diabetes and related care among California adult
population with diabetes, by age, gender, and race/ethnicity, 2013-2016... 21
Figure 13. Leading causes of death in California, 2017................................................. 24
Figure 14. Age-adjusted diabetes mortality rates per 100,000 by
race and ethnicity in California, 2007-2016 .................................................. 25
Appendix Table 1. Variable definitions and associated CHIS questions ....................... 30
Appendix Table 2. Variable definitions and associated BRFSS questions .................... 31
Appendix Table 3. Diabetes complications definitions and ICD-9-CM
and ICD-10-CM codes ...................................................................... 32
Appendix Table 4. Estimated age-adjusted prevalence of diabetes, type 2 diabetes,
and prediabetes among adults (≥ 18 years old) by
counties in California in 2017 ............................................................
34

v
MESSAGE FROM THE CHRONIC DISEASE CONTROL BRANCH CHIEF
June 1, 2019
The estimated prevalence of prediabetes and diabetes among California adults has
significantly increased since 2013, with higher rates among racial and ethnic minorities and
older adults. In 2017, nearly 2.6 million California adults reported having type 2 diabetes, with
15.6 percent of adults estimated to have prediabetes; worsening trends include increases in
prevalence of gestational diabetes. We also have geographic areas in California that have
higher prevalence of diabetes. Finally, on average, medical expenditures for California adults
with diabetes are 2.3 times more expensive than for those without diabetes and those who
have diabetes are at higher risk of comorbidities and death.
As the California Department of Public Health, Center for Healthy Communities, Chronic
Disease Control Branch works to combat chronic disease by addressing determinants of
health, this Report illustrates how poverty, limited education, smoking and obesity are
associated with higher prevalence of diabetes. Thus, it is vital for patients to have access to
regular health care and treatment, including evidence-based lifestyle change programs, in
order to limit complications and poor health outcomes. This includes the management and
prevention of high blood sugar, high blood pressure and high blood cholesterol to reduce
diabetes-related complications.
I invite you to review the Report and utilize the information to further our collaborative efforts to
reduce the preventable disability and premature death from diabetes in California.
Sincerely,
Jessica Núñez de Ybarra, MD, MPH, FACPM, Chief
Chronic Disease Control Branch
California Department of Public Health

Burden of Diabetes in California 1 | P a g e California Department of Public Health
I. INTRODUCTION
Diabetes is the seventh leading cause of death in California, contributing to 9,592 deaths
among adults in 2017.1 In 2017, it was estimated that 3.1 million California adults were
diagnosed with diabetes, representing approximately 1 out of every 9.3 California adults.2 It
was also estimated that 1 out of every 6.4 California adults were diagnosed with prediabetes.2
The National Diabetes Statistics Report, 2017 from the Centers for Disease Control and
Prevention (CDC) indicates that 30.3 million people, or 9.4 percent of the United States
population, have some form of diabetes3—and many with type 2 diabetes do not know they
have the disease. Additionally, it is estimated that 84 million people have prediabetes, an
indicator of higher than normal blood sugar levels that increases the risk for developing type 2
diabetes, and approximately 90 percent of people do not know that they have prediabetes.4
II. DIABETES DEFINITIONS
Diabetes is a complex metabolic disorder in which the body is unable to produce insulin, or has
a decreased ability to use insulin, or both. Diabetes is classified into four main types: type 1,
type 2, gestational, and secondary or other specific types of diabetes. Type 1 diabetes is an
autoimmune disease in which the insulin-producing pancreatic beta cells are destroyed by
autoimmune attack, meaning the body is no longer able to produce insulin, resulting in severe
hyperglycemia. Type 2 diabetes is caused by a combination of insulin resistance (largely due
to obesity) and relative insulin insufficiency. Gestational diabetes is a form of glucose
intolerance that occurs during pregnancy among women who have never been diagnosed with
diabetes prior to pregnancy. Other types of diabetes result from specific genetic conditions
(such as maturity-onset diabetes of youth), surgery, medications, infections, pancreatic
disease, and other illnesses.5 Prediabetes (also called impaired glucose tolerance) is a
condition in which blood sugar levels are higher than normal, but not high enough to be
diagnosed as type 2 diabetes. Type 2 diabetes is the most common form of diabetes,3
accounting for 90 to 95 percent of all diabetes cases. Type 1 diabetes accounts for about 5
percent of all diabetes cases,6 and other types of diabetes account for less than 5 percent of
all diagnosed cases. When the body cannot use or produce insulin properly hyperglycemia, or
high blood glucose, occurs.7 Uncontrolled hyperglycemia can lead to diabetes-related
disabilities such as blindness, nerve damage, amputations, and kidney failure.8
Type 1 diabetes is most often diagnosed in children and young adults, but it can occur at any
age. Insulin resistance typically characteristic of type 2 diabetes can also co-occur with
type 1 diabetes.9 There is no known way to prevent type 1 diabetes, and the only treatment is
lifelong use of insulin.
Unlike type 1 diabetes, type 2 diabetes can be prevented. Awareness of risk factors for type 2
diabetes, which include older age, race/ethnicity, personal history of prediabetes or gestational
diabetes, a family history of type 2 diabetes, or obesity and physical inactivity is necessary to
be able to take action and delay development of the disease.2 10 Nationally, diabetes rates vary

Burden of Diabetes in California 2 | P a g e California Department of Public Health
by race and ethnicity, with American Indian/Alaska Native, African American, Hispanic/Latino,
and Asian/Pacific Islander adults about twice as likely as white adults to have type 2
diabetes.11 Type 2 diabetes can be controlled through healthy food choices, physical activity,
and weight loss, but insulin or oral medication may also be necessary.
Gestational diabetes occurs more often in African American, Hispanic/Latino, and American
Indian/Alaska Native women, as well as in women who are obese or have a family history of
type 2 diabetes.10 Insulin may be required to bring maternal blood glucose to normal levels and
avoid complications in the infant.12 Evidence suggests that women who experience gestational
diabetes, and their children, are more likely to develop type 2 diabetes later in life.10
People with prediabetes are at high risk of developing type 2 diabetes, as well as heart
disease and stroke.4 Studies have shown that people with prediabetes who lose weight and
increase their physical activity can bring blood sugar levels back to normal and may prevent
type 2 diabetes from developing.4
Because gestational diabetes can only develop in women during the course of a pregnancy, in
order to better estimate the burden of diabetes in California, in this report the term diabetes
refers to California adults reporting all types of diabetes except gestational diabetes.
III. DATA SOURCES
Several data sources were used in this report to calculate diabetes prevalence and
hospitalization estimates. The California Health Interview Survey13 (CHIS) and the California
Behavioral Risk Factor Surveillance System Survey14 (BRFSS) were used to estimate the
prevalence of diabetes and other chronic disease conditions and their associated risk factors.
These surveys are both representative population-based, random-dial, cross-sectional surveys
of non-institutionalized individuals in California. Because of their cross-sectional nature, results
from these surveys cannot be used to assess the directionality of disease and associated risk
factors.
The California Office of Statewide Health Planning and Development (OSHPD) dataset of
patients discharged from non-federal hospitals in California15 was used to estimate
hospitalizations for gestational diabetes and for diabetes-related complications.
ICD-9-CM (for years through 2015) and ICD-10-CM (for years including and after 2015) codes
were used to determine the cause of hospitalizations. California Vital Statistics Death
Statistical Master Files16 were used to estimate trends in diabetes mortality rates; ICD-10
codes were used to define diabetes deaths. For a more detailed description of all data
sources, see the Appendix.

Burden of Diabetes in California 3 | P a g e California Department of Public Health
IV. BURDEN OF DIABETES AND PREDIABETES IN CALIFORNIA
Prevalence of Diabetes
• The estimated prevalence of diabetes among California adults significantly increased
from 8.7 percent in 2013 to 10.7 percent in 2017 (p< 0.05).
• In 2017, nearly 2.6 million California adults reported having type 2 diabetes, accounting
for 83.0 percent of diabetes cases among California adults.
Figure 1. Estimated prevalence of diabetes among those with or without a previous prediabetes
diagnosis, 2013-2017
3.8%
3.8%
5.2%
4.6%
5.3%
4.9%
5.1%
4.6%
4.5%
5.4%
8.7%
8.9%
9.8%
9.1%
10.7%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
2013 2014 2015 2016 2017
Diabetes Prevalence (%)
Year
Diabetes without a previous prediabetes diagnosis
Diabetes with a previous prediabetes diagnosis
Total diabetes prevalence
Source: CHIS, 2013-2017 Adult Survey.13

Burden of Diabetes in California 4 | P a g e California Department of Public Health
Estimated Prevalence of Type 2 Diabetes by County in California
• In 2017, the age-adjusted prevalence of type 2 diabetes among California adults was
8.3 percent.
• The prevalence of type 2 diabetes ranged from 3.8 percent to 13.6 percent across
California’s counties, with the highest age-adjusted prevalence of type 2 diabetes in San
Bernardino County.
Figure 2. Estimated age-adjusted prevalence of type 2 diabetes in California by county, 2017
Source: CHIS, 2017 Adult Survey.2 See Appendix Table 4 for the estimated prevalence of type 2
diabetes by county in 2017.

Burden of Diabetes in California 5 | P a g e California Department of Public Health
Prevalence of Prediabetes
• The estimated prevalence of prediabetes among all California adults significantly
increased from 10.1 percent in 2013 to 15.6 percent in 2017 (p < 0.05).
Figure 3. Estimated prevalence of prediabetes among those with and without a subsequent
diabetes diagnosis, 2013-2017
3.8%
3.8%
5.2%
4.5%
5.2%
6.3%
6.7%
8.3%
8.9%
10.4%
10.1%
10.5%
13.5%
13.4%
15.6%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
16.0%
18.0%
2013 2014 2015 2016 2017
Prediabetes Prevalence (%)
Year
Prediabetes without subsequent diabetes diagnosis
Prediabetes with subsequent diabetes diagnosis
Total prediabetes prevalence
Source: CHIS, 2013-2017 Adult Survey.13

Burden of Diabetes in California 6 | P a g e California Department of Public Health
Estimated Prevalence of Prediabetes by County in California
• In 2017, the age-adjusted prevalence of prediabetes among California’s adults was 14.9
percent.
• The prevalence of prediabetes ranged from 3.9 percent to 24.6 percent, with the highest
age-adjusted prevalence of prediabetes in Imperial County.
Figure 4. Estimated age-adjusted prevalence of prediabetes in California by county, 2017
Source: CHIS, 2017 Adult Survey.2 See Appendix Table 4 for prediabetes prevalence estimates among
all California adults by county in 2017.

Burden of Diabetes in California 7 | P a g e California Department of Public Health
Prevalence of Gestational Diabetes
• The estimated prevalence of gestational diabetes among resident California women
hospitalized for labor and delivery increased from 5.7 percent in 2004 to 9.4 percent in
2015.
• Women who experience gestational diabetes are at increased risk of developing type 2
diabetes later in life.10
Figure 5. Estimated prevalence of resident California women hospitalized for labor and delivery
with gestational diabetes mellitus, 2005-2014
* The recommendations for diagnosing gestational diabetes were revised starting January 2011.
Source: California Office of Statewide Health Planning and Development, 2005-2014 Patient Discharge
Data.15
Numerator: Gestational diabetes defined by ICD-9 CM code 648.8
Denominator: Number of women with a labor/delivery diagnosis
Analysis prepared by: Center for Family Health/Maternal, Child and Adolescent Health
Program/Epidemiology, Surveillance and Federal Reporting.
5.7%
6.1%
6.6%
6.7%
7.2%
7.3%
8.2%
9.0% 9.0%
9.4%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
2005 2006 2007 2008 2009 2010 2011 2012 2013 2014
Prevalence (%)
Year
*

Burden of Diabetes in California 8 | P a g e California Department of Public Health
Prevalence of Diabetes, Prediabetes, and Type 2 Diabetes Among California Adults by
Selected Socio-Demographic Characteristics
• The estimated prevalence of diabetes, prediabetes, and type 2 diabetes increased with
age. Adults 65 years and older self-reported the highest prevalence of diabetes.
• The estimated prevalence of diabetes, prediabetes, and type 2 diabetes was higher
among racial/ethnic minorities compared to non-Hispanic Whites.
• The prevalence of diabetes, prediabetes, and type 2 diabetes was slightly higher among
males than females.
Figure 6. Estimated prevalence of diabetes, prediabetes, and type 2 diabetes among California
adults by age, race/ethnicity, and gender, 2013-2017
8.7%
7.5%
9.7%
9.7%
9.8%
7.7%
6.8%
2.1%
11.0%
19.5%
10.2%
8.8%
11.8%
12.2%
12.0%
8.7%
7.7%
3.0%
12.9%
21.4%
13.3%
12.1%
12.4%
16.6%
17.4%
13.9%
11.8%
5.9%
17.4%
22.8%
Male
Female
GENDER
Hispanic
Non-Hispanic African
American
Non-Hispanic
American
Indian/Alaska Native
Non-Hispanic
Asian/Pacific Islander
Non-Hispanic White
RACE/ETHNICITY
18-44 years old
45-64 years old
65+ years old
AGE
0.0% 5.0% 10.0% 15.0% 20.0% 25.0%
Prevalence (%)
Prediabetes Diabetes Type 2 Diabetes
Source: CHIS, 2013-2017 Adult Survey.13

Burden of Diabetes in California 9 | P a g e California Department of Public Health
• The estimated prevalence of type 2 diabetes among California adults with a family
income below 200 percent of the federal poverty level was 21.7 percent compared to
6.0 percent among California adults with an income of 300 percent or more above the
federal poverty level.
• The prevalence of type 2 diabetes was 14.2 percent among those with less than a high
school diploma, compared to 5.7 percent among those with a college degree or higher.
• In contrast, the prevalence of prediabetes was comparable across income and
education levels.
Figure 7. Estimated prevalence of diabetes, prediabetes, and type 2 diabetes among California
adults by education and federal poverty levels, 2013-2017
14.2%
7.8%
7.8%
5.8%
10.5%
11.2%
8.4%
6.0%
17.7%
9.1%
8.9%
6.5%
13.3%
13.1%
9.9%
6.8%
14.3%
12.1%
13.2%
11.9%
0.0%
12.3%
13.4%
13.5%
12.3%
< High School
High School
Some College
College Degree or
Above
EDUCATION
0-99%
100-199%
200-299%
300% or more
FEDERAL …
0.0% 5.0% 10.0% 15.0% 20.0%
Prevalence (%)
Prediabetes Diabetes Type 2 Diabetes
Source: CHIS, 2013-2017 Adult Survey.13

Burden of Diabetes in California 10 | P a g e California Department of Public Health
Prevalence of Diabetes, Prediabetes, and Type 2 Diabetes by Selected Risk Factors
• The estimated prevalence of type 2 diabetes was higher among overweight and obese
California adults compared to adults with a normal body mass index, with the highest
prevalence was among obese adults (14.9 percent).
• Prior smoking is a risk factor for developing type 2 diabetes.17 The estimated prevalence
of type 2 diabetes was highest among former smokers (12.6 percent) followed by
current smokers (7.2 percent).
• The estimated prevalence of prediabetes was highest among obese adults (21.8
percent) and among former smokers (17.9 percent).
Figure 8. Estimated prevalence of diabetes, prediabetes, and type 2 diabetes by body mass
index and cigarette smoking status, 2013-2017
6.7%
12.6%
7.2%
14.9%
7.6%
3.8%
7.9%
14.5%
9.2%
17.1%
9.0%
4.7%
11.0%
17.9%
11.8%
21.8%
12.1%
6.9%
Never smoker
Former smoker
Current smoker
SMOKING
STATUS
Obese
Overweight
Normal
BODY MASS
INDEX
0.0% 5.0% 10.0% 15.0% 20.0% 25.0%
Prevalence (%)
Prediabetes Diabetes Type 2 Diabetes
Source: CHIS 2013-2017 Adult Survey.13 Smoking status refers to California adults reporting that they
currently (at time of interview) smoke cigarettes, were former cigarette smokers, or never smoked
cigarettes.

Burden of Diabetes in California 11 | P a g e California Department of Public Health
Summary of Diabetes Burden in California
The estimated burden of diabetes, prediabetes, and gestational diabetes among California
adults has continued to increase from 2012 through 2017. This burden varies by county,
racial/ethnic groups, age, and gender, which is consistent with the national burden of
diabetes.3 The percentage of California adults reporting they were ever told they had
prediabetes and also reporting that they had diabetes increased from 43.6 percent in 2013 to
49.2 percent in 2017.18

Burden of Diabetes in California 12 | P a g e California Department of Public Health
V. DIABETES COMORBIDITIES
• Individuals diagnosed with diabetes or prediabetes are at risk of comorbidities such as
cardiovascular disease, hypertension, high blood cholesterol, and arthritis. Therefore,
management of diabetes is also important for the prevention of cardiovascular
disease.19
• Although diabetes and hypertension can be managed by incorporating lifestyle
interventions (e.g., physical activity, weight control, and healthy food choices) into daily
routines, arthritis may make these activities more challenging.
• The estimated prevalence of heart disease, hypertension, high cholesterol, and arthritis
were significantly higher among California adults with diabetes compared to those
without diabetes (p < 0.05).
• Similarly, the estimated prevalence of heart disease, hypertension, high cholesterol, and
arthritis were significantly higher among California adults with prediabetes compared to
those without diabetes (p < 0.05).
Figure 9. Estimated prevalence of hypertension, cardiovascular disease, high cholesterol, and
arthritis among California adults with diabetes, prediabetes, and without diabetes, 2013-2017
67.2%
18.6%
64.4%
37.3%
55.6%
13.6%
57.4%
35.8%
24.0%
4.9%
29.7%
16.7%
0.0%
10.0%
20.0%
30.0%
40.0%
50.0%
60.0%
70.0%
80.0%
Hypertension Cardiovascular
Disease
High blood
cholesterol
Arthritis
Prevalence (%)
Diabetes Prediabetes No Diabetes
Source: CHIS, 2013-2017 Adult Survey13 (hypertension and cardiovascular disease data) and CA
BRFSS, 2015 Adult Survey14 (high blood cholesterol and arthritis data).

Burden of Diabetes in California 13 | P a g e California Department of Public Health
• Across all age, gender or racial/ethnic categories, California adults with diabetes had a
higher prevalence of hypertension, cardiovascular disease, high blood cholesterol, and
arthritis than California adults with prediabetes or without diabetes (see Table 1).
• Males had a higher prevalence of hypertension, cardiovascular disease, high blood
cholesterol and arthritis compared to females, regardless of whether they were diabetic,
prediabetic or had no diabetes (see Table 1).
• Among those with diabetes, the prevalence of hypertension was highest among Non-
Hispanic African Americans and the prevalence of cardiovascular disease was highest
among Non-Hispanic Native Americans/Alaska Natives in 2017 (see Table 1).
• Across all ages, gender, and racial/ethnic groups, California adults without diabetes
were more likely to be uninsured or not have a source of medical care than California
adults with diabetes or prediabetes (see Table 2).

Burden of Diabetes in California 14 | P a g e California Department of Public Health
Table 1. Estimated prevalence of other chronic conditions among California adult population with diabetes, prediabetes, and
without diabetes, by age, gender, and race/ethnicity, 2013-2017
Other Chronic
Disease lank
Total
CA
(%)
Age
18-44
(%)
Age
45-64
(%)
Age
65+
(%)
Male
(%)
Female
(%)
Hispanic
(%)
Non-
Hispanic
White (%)
Non-
Hispanic
African
American
(%)
Non-Hispanic
Asian/Pacific
Islander (%)
Non-Hispanic
Native
American/Alaska
Native (%)
Hypertension13
blan
blak
blak
blak
blank
blank
blank
blank
blank
blank
blank
Diabetes
67.2
52.2
63.9
77.0
69.3
64.9
64.1
69.0
80.4
64.8
72.9
Prediabetes
55.6
35.3
55.6
70.4
59.1
52.0
52.3
59.6
67.0
48.0
57.5
No Diabetes
24.0
11.5
31.1
54.8
25.3
23.5
20.3
28.0
34.2
19.2
31.3
Cardiovascular
Disease13
blank
blan
k
blan
k
blank
blank
blank
blank
blank
blank
blank
Diabetes
18.6
8.0
14.6
27.4
19.8
17.2
14.0
25.0
18.0
16.9
34.5
Prediabetes
13.6
4.6
10.8
24.3
15.3
11.9
9.7
18.1
12.2
11.7
20.0
No Diabetes
4.9
1.3
4.9
17.2
5.5
4.4
2.9
7.1
4.3
3.2
9.0
High Blood
Cholesterol14
blank
blan
k
blan
k
blank
blank
blank
blank
blank
blank
blank
Diabetes
64.4
47.5
70.6
62.6
63.7
65.2
63.0
67.0
66.1
61.2
59.1
Prediabetes
57.4
37.4
60.8
65.1
57.9
57.0
47.3
56.6
60.2
74.0
94.2
No Diabetes
29.7
17.7
36.5
48.7
31.5
27.9
26.8
32.6
28.9
26.0
19.5
Arthritis14
blank
blan
blan
blank
blank
blank
blank
blank
blank
blank
Diabetes
37.3
14.7
36.3
49.5
32.0
42.7
27.2
48.3
44.7
27.0
50.0
Prediabetes
35.8
8.8
37.8
52.6
31.8
38.7
25.3
48.6
38.7
20.3
91.3
No Diabetes
16.7
5.3
23.9
47.9
12.9
20.6
10.8
22.9
19.9
7.4
28.2
Source: CHIS 2013-2017 Adult Survey13 and CA BRFSS, 2015 Adult Survey 14 ** indicates unstable estimates due to small sample size.

Burden of Diabetes in California 15 | P a g e California Department of Public Health
Table 2. Estimated prevalence of insurance coverage among California adult population with diabetes, prediabetes,
and without diabetes, by age, gender, and race/ethnicity, 2013-2017
Insurance Status
Total
CA
(%)
Age
18-44
(%)
Age
45-64
(%)
Age
65+
(%)
Male
(%)
Female
(%)
Hispanic
(%)
Non-
Hispanic
White (%)
Non-
Hispanic
African
American
(%)
Non-
Hispanic
Asian/Pacific
Islander (%)
Non-Hispanic
Native
American/
Alaska Native
(%)
Private
blank
blank
blan
blan
blank
blank
blank
blank
blank
blank
Diabetes
28.6
38.1
47.2
3.3
30.4
26.6
26.3
28.7
23.2
38.5
21.5
Prediabetes
41.2
50.3
62.6
3.5
43.2
39.1
37.8
39.7
32.9
58.1
32.9
No Diabetes
52.4
56.6
68.1
4.3
54.0
50.9
40.4
58.4
46.8
64.8
43.8
Medicare only
blank
blank
blan
blan
blank
blank
blank
blank
blank
blank
Diabetes
3.6
0.4**
2.0
6.8
4.3
2.9
2.7
4.7
2.9
4.2
7.3
Prediabetes
2.6
0.1**
1.5
6.1
3.1
2.1
1.8
3.7
2.7
1.6**
3.7**
No Diabetes
1.6
0.1
1.2
7.5
1.5
1.7
0.8
2.4
1.4
0.9
1.5
Medicaid only
blank
blank
blan
blan
blank
blank
blank
blank
blank
blank
Diabetes
20.1
38.9
29.5
1.9
17.1
23.5
28.0
11.2
20.2
16.6
18.4
Prediabetes
17.5
34.2
20.5
1.0
13.9
21.2
26.4
9.7
24.2
12.9
21.4
No Diabetes
17.7
24.4
14.8
0.9
15.2
20.1
28.6
9.4
24.0
14.1
21.9
Uninsured
blank
blank
blan
blan
blank
blank
blank
blank
blank
blank
Diabetes
7.6
18.7
9.8
0.7
8.5
6.6
12.3
3.3
5.8
4.9
5.3
Prediabetes
5.8
10.8
7.2
0.2**
6.0
5.6
10.5
3.2
4.9
2.6
6.1**
No Diabetes
12.4
16.2
11.6
0.9
15.2
9.8
21.8
6.5
9.6
9.1
11.6
No Usual Source
of Care
blank
blank
blan
blan
blank
blank
blank
blank
blank
blank
Diabetes
8.9
17.0
8.8
5.9
10.6
7.0
14.9
3.4
4.0
6.2
4.5**
Prediabetes
7.0
13.0
6.0
4.1
7.7
6.2
11.5
3.3
5.5
6.8
6.9**
No Diabetes
16.0
22.1
11.0
5.4
20.5
11.8
23.1
10.0
13.9
18.0
13.8
Source: CHIS, 2013-2017 Adult Survey.13 ** indicates unstable estimates due to small sample size.

Burden of Diabetes in California 16 | P a g e California Department of Public Health
Summary of Diabetes Comorbidities
Currently, cardiovascular disease and diabetes are among the top ten leading causes of death
in California and nationally, and the risk of developing these diseases is disproportionately
shared among certain racial/ethnic groups and among various sociodemographic factors. The
figures and tables on the proceeding pages show that, compared to California adults without
diabetes, California adults with diabetes self-reported a higher prevalence of hypertension,
cardiovascular disease, high blood cholesterol, and arthritis during 2013-2017. This trend was
consistent by age, gender, and racial/ethnic groups. Because these conditions often arise as
comorbidities of diabetes, the California Department of Public Health (CDPH) recommends
prevention and management of hypertension, cardiovascular health, high blood cholesterol,
and arthritis in an effort to improve and reduce diabetes-related complications.
Burden of Diabetes in California 17 | P a g e California Department of Public Health
VI. DIABETES COMPLICATIONS AND HEALTHCARE USE
End Stage Renal Disease (ESRD)
• ESRD is the most advanced stage of chronic kidney disease, in which the kidneys
permanently fail to work. The only treatment options for ESRD are dialysis or kidney
transplant. In the United States, one-third of adults with diabetes also have chronic
kidney disease.20
• ESRD can be prevented through management of diabetes and hypertension, including
lifestyle modifications and appropriate medications.20
• The estimated prevalence of ESRD in California fluctuated between 2006 and 2016,
with an estimated 1,909 per million in 2016.21
• Figure 10 shows that in 2016, the prevalence of ESRD-related hospitalizations was 241
per 100,000 diabetes hospitalizations.
• Figure 10 shows that diabetes-related ESRD hospitalizations declined by more than 55
percent, from 539 cases in 2006 to 241 cases in 2016 per 100,000 diabetes-related
hospitalizations.
Figure 10. Estimated prevalence of diabetes-related ESRD per 100,000 adult diabetes
hospitalizations, 2006-2016
539
518
445
408
388
366
364
382
342
304
241
200
250
300
350
400
450
500
550
600
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016
ESRD per 100,000 diabetes-related
hospitalizations
Year
Source: OSHPD, 2006-2016 Patient Discharge Data.15

Burden of Diabetes in California 18 | P a g e California Department of Public Health
Ophthalmic Complications
• Individuals with diabetes are at risk of ophthalmic (eye) complications, such as diabetic
retinopathy and blindness. Comorbidities such as hypertension are also linked to
developing retinopathy.22
• In the United States, an estimated 40-45 percent of people with diabetes have some
stage of diabetic retinopathy.23
• However, early detection can occur through routine eye exam screenings. In 2010, 62.8
percent of adults with diabetes indicated that they had their eyes dilated and examined
in the past year.24
• Treatment of diabetic retinopathy can include careful management of blood glucose and
blood pressure levels, medication, and sometimes surgery.25
• Figure 11 shows that the rate of diabetes-related ophthalmic hospitalizations in
California decreased to less than a third from 32 cases in 2006 to 10 cases in 2016 per
100,000 diabetes-related hospitalizations.
Figure 11. Estimated prevalence of diabetes-related ophthalmic hospitalizations per 100,000
adult diabetes hospitalizations, 2006-2016
32
28
30
25
25
24
22
20
17
16
10
0
5
10
15
20
25
30
35
40
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016
Opthalmic complications per 100,000 diabetes-
related hospitalizations
Year
Source: OSHPD, 2006-2016 Patient Discharge Data.15

Burden of Diabetes in California 19 | P a g e California Department of Public Health
Lower Extremity Amputations
• Chronic hyperglycemia (high blood glucose) causes changes in cell function, which can
eventually progress to nerve damage known as diabetic neuropathy. This cellular
damage can also contribute to the development of foot ulcers or infections that may
require lower extremity amputations.26 Nationally, diabetes is the leading cause of lower
extremity amputations, with an estimated 60 percent of all non-traumatic lower-limb
amputations occurring among people with diabetes.27
• Diabetes-related amputations can be prevented by managing and controlling glucose
and cholesterol levels, blood pressure, and receiving routine screening and treatment
for feet.28
• Figure 12 shows the rate of diabetes-related lower limb amputations in California
increased more than 40 percent from 1,081 cases in 2009 to 1,552 cases in 2016 per
100,000 diabetes-related hospitalizations.
Figure 12. Estimated prevalence of diabetes-related lower extremity amputations per 100,000
diabetes hospitalizations, 2006-2016
1234
1167
1123
1081
1082
1166
1239
1307
1381
1415
1552
1000
1100
1200
1300
1400
1500
1600
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016
Lower extremity amputations per 100,000 diabetes-
related hospitalizations
Year
Source: OSHPD, 2006-2016 Patient Discharge Data.15

Burden of Diabetes in California 20 | P a g e California Department of Public Health
Healthcare Use
• Diabetes management, including regular health care visits to monitor blood control, eye
health, and lower extremities, is necessary to prevent diabetes complications and the
development of other comorbidities.28
• Persons with diabetes should see their doctors regularly to have their hemoglobin A1c,
an indicator of average blood glucose levels over the previous 3 months, monitored.29
Hispanics had the lowest rate of A1c test in the past year compared to non-Hispanics in
California (see Table 3). Hispanics and non-Hispanic Native American/Alaska Natives
also had a lower diabetes management screening rate for both an eye and foot exam in
the past year than the state average.
• Across age, gender, and race and ethnicity, over 70 percent of California adults with
diabetes had a diabetes management plan; however, Hispanics and non-Hispanic
Native American/Alaska Natives had the lowest proportion among California adults with
diabetes (see Table 3).
• Over 90 percent of all those with a plan were confident in their abilities to manage their
diabetes (see Table 3). In contrast, confidence in the ability to manage diabetes was
slightly lower amongst those without a diabetes management plan (see Table 3).

Burden of Diabetes in California 21 | P a g e California Department of Public Health
Table 3. Estimated prevalence of diabetes and related care among California adult population with diabetes, by age, gender,
and race/ethnicity, 2013-2016
Diabetes and
Related Care
Total
CA
(%)
Age
18-44
(%)
Age
45-64
(%)
Age
65+
(%)
Male
(%)
Female
(%)
Hispanic
(%)
Non-
Hispanic
White
(%)
Non-
Hispanic
African
American
(%)
Non-
Hispanic
Asian/Pacific
Islander
(%)
Non-Hispanic
Native
American/Alaska
Native (%)
Diabetes Management
Screening
blan
k
blank
blak
blan
blan
k
blank
blank
blank
blank
blank
blank
At least one A1C test in
past year
80.8
72.7
82.4
82.1
80.6
81.0
70.7
90.2
83.9
87.8
84.2
Eye exam within past year
70.7
52.5
67.3
81.5
70.7
70.7
66.4
74.9
71.3
73.9
62.9
At least one foot exam in
past year
72.1
59.0
72.6
76.7
73.3
70.9
70.0
74.0
79.4
70.7
60.4
Diabetes Medication
Management
blan
k
blank
blak
blak
blan
k
blank
blank
blank
blank
blank
blank
Take pills or insulin for
diabetes
82.9
76.2
84.2
84.1
83.8
82.0
82.9
80.5
84.0
88.2
81.1
Diabetes Management
Plan
blan
k
blank
blak
blak
blan
k
blank
blank
blank
blank
blank
blank
Have a diabetes
management plan
78.0
72.0
81.5
76.3
78.5
77.5
72.1
86.0
85.3
73.4
71.4
Confidence in Ability to
Control Diabetes
blan
k
blank
blan
blan
blan
k
blank
blank
blank
blank
blank
blank
Percentage of those with
a plan who are confident
in abilities to manage
diabetes
93.4
92.7
91.8
95.7
94.5
92.2
91.3
95.6
94.8
93.0
97.7

Burden of Diabetes in California 22 | P a g e California Department of Public Health
Table 3. Estimated prevalence of diabetes and related care among California adult population with diabetes, by age, gender,
and race/ethnicity, 2013-2016 (cont.)
Diabetes and
Related Care
Total
CA
(%)
Age
18-44
(%)
Age
45-64
(%)
Age
65+
(%)
Male
(%)
Female
(%)
Hispanic
(%)
Non-
Hispanic
White
(%)
Non-
Hispanic
African
American
(%)
Non-
Hispanic
Asian/Pacific
Islander
(%)
Non-Hispanic
Native
American/Alaska
Native (%)
Percentage of those
without a diabetes
management plan who
are confident in abilities
to manage diabetes
85.0 84.9
82.9
87.0
87.5
82.5
84.0
89.4
93.3
81.5
92.0
Source: CHIS, 2013-2016 Adult Survey.13 * A1c test refers to a hemoglobin A1c test, which measures the percent of hemoglobin with
attached glucose and reflects average blood glucose levels over the previous 3 months. A hemoglobin A1c test can be used alone or in
combination with other tests to diagnosis diabetes, and after a diabetes diagnosis, is used to monitor long term blood glucose
management.29

Burden of Diabetes in California 23 | P a g e California Department of Public Health
Financial Cost of Diabetes and its Complications
According to a 2016 Health Policy Brief, the current trends in diabetes and prediabetes are
alarming because of the associated health, human, and financial costs.30 Diabetes increases
the risk of serious medical complications and is extremely costly to families, businesses, health
care plans, states, and the nation. In 2017, the national estimated cost of diabetes was $327
billion, with $237 billion in direct medical costs and $90 billion in lost productivity.31 Given that
the prevalence of diabetes and prediabetes continues to increase over time, it is expected that
the costs associated with diabetes and its complications will continue to rise.
In California, the medical expenditures to treat diabetes total approximately $1.9 billion, with an
additional $800 million in lost productivity each year.32-34 Diabetes-related ESRD adds an
additional $2,693 million/year, lower limb amputations add an additional $195 million/year, and
blindness adds an additional $36 million/year in total medical expenditures.32 On average,
medical expenditures for California adults with diabetes are 2.3 times more than those without
diabetes.35

Burden of Diabetes in California 24 | P a g e California Department of Public Health
VII. DIABETES MORTALITY
• In 2017, diabetes was the seventh leading cause of death among adults (18 years and
older) in California, with 9,592 deaths attributed to diabetes as the underlying cause.
Moreover, diabetes was listed as a contributing cause of death in 32,871 deaths in
California in 2017.36
• Additionally, adults with diabetes are almost twice as likely to die from heart disease or
stroke as adults without diabetes.19
Figure 13. Leading causes of death in California, 2017
1,701
1,906
3,370
3,881
4,185
5,324
5,596
6,308
9,592
13,422
13,861
16,236
16,325
59,320
62,729
0 20,000 40,000 60,000 80,000
Pneumonitis
Homocide
Parkinson's Disease
Nephritis
Suicide
Chronic Liver
Disease/Cirrhosis
Hypertension/Hypertensive
Renal Disease
Influenza and Pneumonia
Diabetes Mellitus
Unintentional Injuries
Chronic Lower Respiratory
Diseases
Alzheimer's Disease
Cerebrovascular Diseases
Cancer
Heart Disease
Number of Deaths
Source: CDC WONDER Database, 2017.1 Deaths are amongst people ages 18 and older.

Burden of Diabetes in California 25 | P a g e California Department of Public Health
Diabetes Mortality by Race/Ethnicity
• There are disparities in diabetes mortality rates across race and ethnic groups in
California.
• African Americans experienced the highest rates of diabetes mortality between 2007
and 2016 while Whites and Asian/Pacific Islanders experienced the lowest rates.
Figure 14. Age-adjusted diabetes mortality rates per 100,000 by race and ethnicity in
California, 2007-2016
20
07
20
08
20
09
20
10
20
11
20
12
20
13
20
14
20
15
20
16
Hispanic
43.6 42.1 35.5 36.8 37.6 37.9 38.3 36.2 36.9 37.9
Non-Hispanic White
24.9 24.4 22.5 22.6 23.8 23.8 22.8 22.7 23.5 23.4
Non-Hispanic African American
63.4 58.0 53.2 50.5 55.0 53.1 50.8 55.7 58.6 57.9
Non-Hispanic Native
American/Alaskan Native
53.3 44.2 34.8 40.5 44.0 50.2 44.7 33.3 51.8 51.8
Non-Hispanic Asian/Pacific
Islander
24.7 25.3 22.0 22.0 23.8 23.5 23.9 23.7 24.6 23.8
20.0
25.0
30.0
35.0
40.0
45.0
50.0
55.0
60.0
65.0
Age-adjusted mortality rates (per 100,000 people)
Source: California Vital Statistics Death Data, 2007-2016.16 2007-2010 population data from the
California Department of Finance,37 2011-2016 population data from the United States Census
Bureau.38 Diabetes deaths defined by ICD10 codes E10x-E14x for the underlying cause of death.
Deaths are of people ages 18 and above.

Burden of Diabetes in California 26 | P a g e California Department of Public Health
VIII. DIABETES PREVENTION AND CONTROL ACTIVITIES
CDPH
To equitably address the burden of diabetes and prediabetes, the CDC suggests promotion of
evidence-based lifestyle change programs. The CDC recommends several training programs
including but not limited to: the National Diabetes Prevention Program (National DPP),
Diabetes Self-Management Education and Support (DSMES), the Expanded Food and
Nutrition Education Program (EFNEP), smoking cessation, and physical activity to prevent and
manage type 2 diabetes. Participation in lifestyle change programs can increase awareness
about lifestyle choices that reduce the risk of type 2 diabetes. Additionally, incorporating
support from a care team that includes non-physician team members such as
pharmacists39 and community health workers,40 can help individuals with type 2 diabetes or at
risk of type 2 diabetes adopt and sustain lifestyle changes as they navigate through diabetes
prevention resources.
CDPH is involved in several diabetes prevention and control activities to reduce the burden
and prevalence of type 2 diabetes in California. In 2018, CDPH received the Improving the
Health of Americans Through Prevention and Management of Diabetes and Heart Disease and
Stroke five year (2018-2023) federal grant from the CDC
(CDC-RFA-DP18-1815PPHF18), referred to at CDPH as Prevention Forward. This grant funds
efforts to work with traditional and nontraditional partners to prevent and manage chronic
conditions such as diabetes, increase monitoring of and reporting on chronic disease, and
increase referrals to and participation in lifestyle change programs. Under Prevention Forward,
CDPH focuses on communities with a high burden of chronic disease in its efforts to reduce
diabetes-related disparities and costs; to promote awareness and reporting of type 2 diabetes,
prediabetes, cardiovascular disease, and high blood pressure among at risk populations; and
to educate and train health care professionals (including physicians and non-physician team
members) in medical/academic institutions about the importance of diabetes interventions,
routine screening and glucose testing to identify and educate patients with prediabetes and
diabetes.
Prevention Forward builds upon the work CDPH mobilized under the State Public Health
Actions to Prevent and Control Diabetes, Heart Disease, Obesity and Associated Risk Factors
and Promote School Health (CDC-RFA-DP13-1305) (funded between 2013-2018) and the
Heart Disease and Stroke Prevention Program and Diabetes Prevention – State and Local
Public Health Actions to Prevent Obesity, Diabetes, and Heart Disease and Stroke (CDC-RFA-
DP14-1422PPHF14) (funded between 2014 and 2018) grants. Those grants provided
Prevention Forward with a strong foundation in the use of evidence-based strategies to
prevent and manage diabetes. Prevention Forward staff continue the partnerships and
discussions about the use of electronic health records to increase diabetes and prediabetes
screening, testing, and referrals to lifestyle change programs, to develop health system
interventions to improve the quality of health care delivered to high burden populations, and to
use team-based models to address diabetes prevention and management.

Burden of Diabetes in California 27 | P a g e California Department of Public Health
Under the 2013-2018 CDC grants, CDPH collaborated with the CDC, the American Medical
Association (AMA), and the National Association of Chronic Disease Directors (NACDD) to
establish the California Prevent Diabetes: Screen, Test, Act, TodayTM (CA PDSTAT) network.
CA PDSTAT continues under Prevention Forward, with the goal of increasing the availability of
and support for National DPPs and DSMES programs in California, increasing awareness of
diabetes and prediabetes among Californians, encouraging employers and insurers to offer
National DPP as a covered benefit, and increasing referrals of individuals to National DPP and
DSMES programs. The CA PDSTAT network consists of representatives from health care
organizations, the community at large, volunteer organizations, health insurance organizations,
government (state, county, and city) employees, and others interested in type 2 diabetes
prevention and management. Through this collaboration, CA PDSTAT developed policy
recommendations for the prevention and management of type 2 diabetes, which resulted in the
Diabetes Prevention Through Lifestyle Change Programs: 2018 Action Plan
(https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CDCB/CDPH%20Document%20Library/
DiabetesPrevActionPlan_FinalADA-07%2003%2018%20v2.pdf). This Action Plan focuses on
interventions for individuals with prediabetes to prevent progression to type 2 diabetes, namely
increased awareness, availability, coverage, and utilization of evidence-based National DPPs.
In July 2018, CDPH received funding from the California Budget Act 2018 to develop and
implement a Diabetes Awareness and Outreach Campaign. The goal of this media campaign
is to engage Californians at risk for type 2 diabetes about their risk factors, increase
awareness of the link between type 2 diabetes and cardiovascular disease, and promote
resources and National DPPs. Implementation of this campaign will include traditional media,
advertising, and social media under the guidance of an advisory committee, and will continue
through June 30, 2020.
CDPH’s Chronic Disease Control Branch (CDCB) collaborates with the California Department
of Health Care Services (DHCS) on the 6|18 Initiative. The 6|18 Initiative connects health care
purchasers, payers, and providers with CDC researchers, economists, and policy analysts to
find ways to improve health and control costs of six common health conditions through the use
of 18 proven interventions.41 DHCS and CDPH are focusing on type 2 diabetes prevention
through the expansion of access to the National DPP, which became a Medi-Cal covered
benefit on January 1, 2019.
The CDPH’s Maternal, Child, and Adolescent Health Division (MCAH) implements the
California Diabetes and Pregnancy Program (CDAPP) and Sweet Success program, funded by
the Maternal and Child Health Services Title V BlChock Grant. CDAPP’s Sweet Success
program provides technical support and education to medical personnel and community
liaisons to promote improved pregnancy outcomes for high-risk pregnant women with pre-
existing diabetes and women who develop gestational diabetes while pregnant. Medical
providers who complete a CDAPP Sweet Success application, undergo standardized CDAPP
Sweet Success training, and provide direct patient care to pregnant women with diabetes
become CDAPP Sweet Success Affiliates. The MCAH Division contracts with the CDAPP
Sweet Success Resource Center to develop and record training and education to medical
personnel to promote improved pregnancy outcomes for high-risk pregnant women with
preexisting and gestational diabetes. The Resource Center trained about 2,000 program

Burden of Diabetes in California 28 | P a g e California Department of Public Health
affiliates in 2017-2018 through online trainings that covered a range of subjects, including
gestational diabetes. In addition to training, the Sweet Success Resource Center provided
educational resources for both providers and pregnant women with diabetes. For more
information on available resources, visit the CDAPP Sweet Success program website at
www.cdappsweetsuccess.org/resources.
Community-Related Diabetes Activities
Diabetes prevention and management efforts also take place at the local level throughout
California. For example, Monterey County, with Prevention First funding, created an
educational pathway for students to serve as community health workers (CHWs) for diabetes
prevention in the county’s Latino community.42 Additionally, culturally-adapted national
Prediabetes Awareness Campaign public service announcement advertisements ran for two
years in the Central Valley, Los Angeles, and San Diego. Furthermore, in 2018, the CDC
awarded funds via the Innovative State and Local Public Health Strategies to Prevent and
Manage Diabetes and Heart Disease and Stroke grant (CDC-RFA-DP18-1817) to the Fresno,
Los Angeles, and San Diego local health departments to design, test, and evaluate innovative
approaches to address diabetes, heart disease, and stroke, which align with and support the
goal of Prevention Forward.43 The Los Angeles County Public Health Department received
funding to address diabetes as well as heart disease and stroke.43
Diabetes-Related Policies in California
Several efforts have been undertaken by the state legislature, local health departments, and
health insurance companies to address the burden of diabetes. In 2017, the California Public
Employees Retirement System (CalPERS) began offering the National DPP as a covered
benefit to its more than 1.4 million adult members.44 Additionally, in 2019, Medi-Cal began to
offer the National DPP as a covered benefit.45 CDPH’s CDCB will continue to work with health
plans to cover and promote enrollment in National DPPs and DSMES programs.
IX. CONCLUSIONS
Type 2 diabetes and prediabetes rates are increasing in California. There are geographic and
sociodemographic disparities in the prevalence of diabetes and prediabetes in California, as
well as in diabetes management and mortality rates. CDPH, local health departments, and
community partners are involved in a number of efforts to address these disparities in
California. With support from CDC grants, CDPH is working to target communities with a high
burden of chronic disease in its efforts to reduce diabetes-related disparities and costs; to
promote awareness and reporting of type 2 diabetes, prediabetes, cardiovascular disease, and
high blood pressure among at risk populations; and to educate and train health care
professionals about the importance of diabetes interventions. Additionally, Medi-Cal coverage
of the National DPP will increase access to diabetes prevention programs for low-income and
vulnerable populations. Through these efforts, California aims to improve diabetes prevention
and management throughout the state, and therefore improve the health of all Californians.

Burden of Diabetes in California 29 | P a g e California Department of Public Health
APPENDIX
Data Sources
CHIS
CHIS is a representative population-based, random-dial, cross-sectional health survey of non-
institutionalized individuals in California and covers a wide range of health topics. The survey
provides statewide information on the health and health needs of the overall population in
California including many racial and ethnic groups. CHIS is designed to meet two sampling
objectives: (1) provide estimates for 44 large and medium-size counties in California, and for
groups of counties with the smallest populations; and (2) provide estimates for California’s
overall population, major racial and ethnic groups, and for several smaller ethnic subgroups.
Sampling weights are applied to the data files and are based on the State of California’s
Department of Finance population estimates and projections with adjustment for populations
not eligible to participate in CHIS (e.g., nursing homes, prisons). The resulting weighted
estimates represent one year of California’s residential population.46 For this report, CHIS
survey data from 2013, 2014, 2015, 2016, and 2017 were pooled and weights were adjusted
accordingly.46,47 Further information on the design and methodology of CHIS is available on
the UCLA Center for Health Policy Research website (http://healthpolicy.ucla.edu/chis/).
The table below outlines the CHIS questions used to define each variable:

Burden of Diabetes in California 30 | P a g e California Department of Public Health
Appendix Table 1. Variable definitions and associated CHIS questions
Variable Definition
Associated CHIS Question
Diabetes
Calculated based on a response of “yes” to the question: “Other than during
pregnancy, has a doctor ever told you that you have diabetes or sugar
diabetes?”
Prediabetes
Calculated based on a response of “yes” to the question: “Other than during
pregnancy, has a doctor ever told you that you have diabetes or sugar
diabetes?” AND a response of “prediabetes” to the question: “Were you told
that you had Type 1 or Type 2 Diabetes?” (2015-2017) OR a response of
“yes” to the question: “Other than during pregnancy, has a doctor ever told
you that you have pre or borderline diabetes?” (2013-2017)
Type 2 Diabetes
Calculated based on a response of “yes” to the question: “Other than during
pregnancy, has a doctor ever told you that you have diabetes or sugar
diabetes?” AND a response of “type 2 diabetes” to the question: “Were you
told that you had type 1 or type 2 diabetes?”
Hypertension
Calculated based on a response of “yes” to the question: “Has a doctor ever
told you that you have high blood pressure?”
Cardiovascular
disease
Calculated based on a response of “yes” to the question: “Has a doctor ever
told you that you have any kind of heart disease?”
Smoking Status
Defined by CHIS based on several questions about smoking habits and
categorized as “Currently Smokes,” “Quit Smoking,” and “Never Smoked
Regularly.”
Body Mass Index
Defined by CHIS based on self-reported height and weight estimates, and
categorized as: “Underweight 0-18.49,” “Normal 18.5-24.99,” “Overweight
25.0-29.99,” and “Obese 30.0+”
Federal Poverty
Level
Defined by CHIS based on several questions on self-reported income level
and categorized as: “0-99% FPL,” “100-199% FPL,” “200-299% FPL,” and
“300% FPL and above”
Education Level
Defined by CHIS based on the question: “What is the highest grade of
education you have completed and received credit for?” and categorized as
“< High School Education,” “High School Education,” “Some College,” and
“College Degree or Above”
Age
Self-reported age at the time of the interview, as reported by CHIS to the
question: “What is your age, please?”
Race/Ethnicity
Defined by CHIS based on several questions about self-reported
race/ethnicity, and categorized as the Office of Management and Budget and
Census Bureau race/ethnicity categories: 1 = Hispanic, 2 = White, Non-
Hispanic, 3 = African American Only, Not Hispanic, 4 = American
Indian/Alaska Native only, Non-Hispanic, 5 = Asian Only, Non-Hispanic, 6 =
Native Hawaiian/Pacific Islander, Non-Hispanic, 7 = Two or More Races,
Non-Hispanic)
Gender
Self-reported gender based on the response to the question: “Are you male
or female?”

Burden of Diabetes in California 31 | P a g e California Department of Public Health
California BRFSS
BRFSS was established in 1984 by the CDC and is currently conducted in all 50 states and
multiple United States territories. The California BRFSS has been conducted continuously
since 1984 and provides an abundant source of information regarding health risk behaviors,
attitudes, knowledge and beliefs, preventive health practices, and disease prevalence. The
California BRFSS and its annual questionnaire development is a collaborative effort between
the CDC, CDPH, DHCS, and the California Department of Social Services. The BRFSS is a
random-digit dial telephone survey that collects data yearly from non-institutionalized adults
(18+ years of age), and includes both cell phone (since 2013) and landline random-digit dial
components.48 Once a household is identified, respondents are randomly selected from among
all eligible adults. The age, race, and sex distribution of the sample does not completely match
that of the California population because minorities are over-sampled to ensure they are
represented in the survey.48 Therefore, the sample was weighted to California population
estimates to improve the representativeness of the sample. For this report, BRFSS survey
data from 2013 and 2015 were pooled and weights were adjusted accordingly. Prevalence
estimates from this report should not be compared to estimates from before 2012 due to
changes in the weighting methodology. Further information on the design and methodology of
the California BRFSS is available on the CSUS Public Health Survey Research Program
website (https://www.csus.edu/research/phsrp/brfss.html).
The table below outlines the BRFSS questions used to define each variable:
Appendix Table 2. Variable definitions and associated BRFSS questions
Variable Definition
Associated BRFSS Question
Diabetes
Calculated based on a “yes” response to the question: “Has a
doctor, or nurse or other health professional ever told you that you
have diabetes?” (excludes the response: “Yes, but female told only
during pregnancy”)
High blood cholesterol
Calculated based on a “yes” response to the question: “Have you
ever been told by a doctor, nurse or other health professional that
your blood cholesterol is high?”
Arthritis
Calculated based on a “yes” response to the question: “Has a
doctor, nurse, or other health professional EVER told you that you
have some form of arthritis, rheumatoid arthritis, gout, lupus, or
fibromyalgia?”
Age
Self-reported age at the time of the interview, as reported by
BRFSS based on the response to the question: “What is your age?”
Race/ethnicity
Calculated based on multiple questions about self-reported race
and Hispanic status (White, Black or African American, American
Indian/Alaska Native, Asian, Pacific Islander, other; Hispanic)
Gender
Self-reported gender, as reported by BRFSS based on the
response to the question: “Are you male or female?”

Burden of Diabetes in California 32 | P a g e California Department of Public Health
CDC WONDER Database
The CDC’s Wide-ranging ONline Data for Epidemiologic Research (CDC WONDER) system
was used to generate the leading causes of death in California.1 CDC WONDER’s mortality
data was published by the National Center for Health Statistics and the CDC from the Multiple
Cause of Death Files, 1999-2017, as compiled from data provided by the 57 vital statistics
jurisdictions through the Vital Statistics Cooperative Program. Accessed at
https://wonder.cdc.gov/ucd-icd10.html on April 22, 2019.
California Vital Statistics Data
The California Vital Statistics Data was used for calculating age-adjusted mortality rates in
California.16 The death certificates contain the cause of death, coded using the International
Classification of Diseases (ICD-10). Diabetes deaths were defined by ICD10 codes E10x-
E14x.
OSHPD Patient Discharge Data
The California Office of Statewide Health Planning and Development compiles administrative
data on all patients discharged from non-federal hospitals in California.15 This discharge data
was used to calculate rates of hospitalizations for diabetes-related complications, including
end-stage renal disease, ophthalmic complications, and lower extremity amputations. Diabetes
was defined when a diabetes-related ICD code was present for any of the primary or 24 other
diagnosis codes, whereas diabetes-related complications were defined based on primary
diagnosis or primary procedure codes only.
Appendix Table 3. Diabetes complications definitions and ICD-9-CM and ICD-10-CM codes
Conditions and Procedures
ICD Codes
Gestational diabetes
ICD-9-CM diagnosis codes: 648.80-648.84
Diabetes (any diagnosis)
ICD-9-CM diagnosis codes: 250.0-250.93
ICD-10-CM diagnosis codes: E10x-E13x
Diabetes-related ESRD (primary
diagnosis)
ICD-9-CM diagnosis codes: 250.40-250.43
ICD-10-CM diagnosis codes: E10.22, E11.22, E12.22, E13.22
Diabetes-related ophthalmic
complications (primary
diagnosis)
ICD-9-CM diagnosis codes: 250.50-250.53
ICD-10-CM diagnosis codes: E10.3-E10.39, E11.3-E11.39,
E12.3-E12.39, E13.3-E13.39
Diabetes-related lower extremity
amputation (primary procedure)
ICD-9-CM procedure codes: 84.1-84.19 AND Diabetes ICD9
CM diagnosis codes
ICD-10-CM procedure codes: 0Y620ZZ-0Y6Y0Z3 AND
Diabetes ICD-10-CM diagnosis codes
For diabetes-related complications, ICD-9-CM codes were used to define conditions for years
2006-2015, and ICD-10-CM codes were used to define conditions for years 2015-2016 (the
transition from ICD-9-CM to ICD-10-CM coding occurred over the course of 2015, so both
coding schemes are present in hospitalization records in 2015).

Burden of Diabetes in California 33 | P a g e California Department of Public Health
California Department of Finance Population Data
California county population data are published by the California Department of Finance’s
Demographic Research Unit. County population estimates were from “E-2. California County
Population Estimates and Components of Change by Year—July 1, 2010-2017” (released
December 2017).37 California population data by race and age between 2007 and 2010 (for
calculating age-adjusted diabetes mortality rates in Figure 14) are from “California and
Counties by Age and Race/Ethnicity – Total Only: 2000-2010” (released March 2013).49
United States Census Bureau California Population Data
Population data by race and age in California between 2011 and 2016 (for calculating age-
adjusted diabetes mortality rates in Figure 14) are from the United States Census Bureau.38
Statistical Methods
Age Adjustment
In this report, age-adjustment was performed using the direct method and the 2000 United
States Standard Population.50 Age adjustment is a calculation that allows different populations
to be directly compared. Age adjustment is necessary because diabetes prevalence and
mortality rates increase with age. Therefore, without age adjustment, if a population with
mostly young people were compared to a population with mostly old people, the diabetes rate
would be higher in the older population, but it would be impossible to tell if the diabetes rate
was higher because of the age of the population or due to another factor. Age adjustment
adjusts the rates so that both populations have the same distribution of old and young people,
making it easier to tell if there is another factor affecting the diabetes rates aside from age.
Confidence Intervals
Confidence intervals represent the precision of an estimate where the true parameter falls.
Wide confidence intervals indicate that the true parameter could fall anywhere in a wide range,
and the measured value is subject to a large degree of random error. In contrast, narrow
confidence intervals indicate that the true parameter falls inside a small range, and random
error is less-likely to have affected the measured value. The number of individuals with the
condition used to calculate the estimate directly correlates with the precision. If the estimate is
based on a small number of individuals, the confidence interval will be wide. This report uses
the 95% confidence interval indicating our level of certainty.
Unstable Estimates
Estimates with a coefficient of variation ((standard error of the estimate/estimate)*100) ≥ 30%
are considered unstable and should be interpreted as unreliable. An estimate is unstable if
only a few respondents are represented with the specific characteristics and/or disease (small
numerator) and, thus, represented by a large standard error relative to the estimate. All
estimates in this report were evaluated for instability, and if unstable, were marked as such.

Burden of Diabetes in California 34 | P a g e California Department of Public Health
Supplementary Data
Appendix Table 4. Estimated age-adjusted prevalence of diabetes, type 2 diabetes, and
prediabetes among adults (≥ 18 years old) by counties in California in 2017
County
Estimated
Population
Size (2017)
Diabetes
Age-adjusted
Prevalence (%)
Type 2
Diabetes
Age-adjusted
Prevalence (%)
Prediabetes
Age-adjusted
Prevalence (%)
California
39,500,973
10.1
8.3
14.9
Alameda
1,646,405
9.2
8.2
19.9
Butte
226,403
8.8
7.1
12.4
Contra Costa
1,139,313
8.9
6.2
12.9
El Dorado
186,223
6.0
5.0
7.3
Fresno
995,233
12.1
9.2
12.7
Humboldt
136,430
5.6
4.7
8.9
Imperial
187,921
18.7
12.6
24.6
Kern
896,101
14.4
10.8
19.1
Kings
149,559
14.8
13.1
12.9
Lake
64,740
9.9
7.8
14.4
Los Angeles
10,231,271
11.4
9.5
16.7
Madera
156,963
9.4
9.3
13.8
Marin
263,262
3.9
3.9
6.8
Mendocino
89,092
9.5
5.1
8.4
Merced
275,104
10.7
8.2
19.7
Monterey
442,149
9.0
6.9
10.6
Napa
141,784
6.1
4.5
13.9
Nevada
98,613
5.3
4.9
3.9
Orange
3,198,968
8.5
7.0
13.3
Placer
383,173
4.8
3.8
11.0
Riverside
2,382,640
10.0
7.8
14.8
Sacramento
1,513,415
9.7
7.3
16.5
San Benito
56,879
9.5
7.7
8.7
San Bernardino
2,155,590
14.7
13.6
17.7
San Diego
3,309,509
9.3
8.0
12.6
San Francisco
874,008
6.8
5.8
11.4
San Joaquin
747,263
15.2
12.9
14.5
San Luis Obispo
279,210
5.9
3.9
8.2
San Mateo
770,256
9.5
7.7
13.1
Santa Barbara
450,025
4.4
3.9
8.9
Santa Clara
1,937,473
6.9
5.2
16.1
Santa Cruz
276,504
5.3
4.5
10.9

Burden of Diabetes in California 35 | P a g e California Department of Public Health
Source: CHIS 2017 Adult Survey,2 population estimates from the California Department of Finance
2017 county population estimates.37
County
Estimated
Population
Size (2017)
Diabetes
Age-adjusted
Prevalence (%)
Type 2
Diabetes
Age-adjusted
Prevalence (%)
Prediabetes
Age-adjusted
Prevalence (%)
Shasta
178,148
9.5
5.7
7.7
Solano
436,640
10.4
10.0
17.6
Sonoma
504,613
9.2
6.2
8.1
Stanislaus
549,976
12.8
11.0
15.0
Sutter
96,919
10.0
9.0
15.7
Tulare
470,716
13.8
12.4
12.1
Ventura
855,910
9.5
7.8
12.7
Yolo
218,673
8.5
8.4
9.7
Yuba
74,645
16.0
10.8
13.3
Tuolumne,
Calaveras,
Amador, Inyo,
Mariposa, Mono,
Alpine
189,932
5.5
5.1
13.5
Del Norte,
Siskiyou, Lassen,
Trinity, Modoc,
Plumas, Sierra
148,593
6.9
5.7
8.8
Colusa, Glenn,
Tehama
114,729
10.8
10.7
13.0

Burden of Diabetes in California 36 | P a g e California Department of Public Health
REFERENCES
1. Centers for Disease Control and Prevention- National Center for Health Statistics.
Underlying Cause of Death 1999-2017 on CDC WONDER Online Database, released
December, 2018. Data are from the Multiple Cause of Death Files, 1999-2017, as
compiled from data provided by the 57 vital statistics jurisdictions through the Vital
Statistics Cooperative Program http://wonder.cdc.gov/ucd-icd10.html. Accessed April
22, 2019.
2. California Health Interview Survey. CHIS 2017 Adult Survey. Los Angeles, CA: UCLA
Center for Health Policy Research; October 2018. 2017.
3. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017.
2017.
4. Centers for Disease Control and Prevention. Prediabetes: Your Chance to Prevent Type
2 Diabetes. https://www.cdc.gov/diabetes/basics/prediabetes.html. Accessed
November 27, 2018.
5. Forlenza GP, Moran A, Nathan B. Other Specific Types of Diabetes. Chapter 6 in
Diabetes in America, 3rd ed. In: Cowie CC, Casagrande SS, Menke A, et al., eds.
Diabetes in America, 3rd ed. Vol 17-1468. Bethesda, MD: National Institutes of Health;
2018:1-29.
6. Imperatore G, Mayer-Davis EJ, Orchard TJ, Zhong VW. Prevalence and Incidence of
Type 1 Diabetes Among Children and Adults in the United States and Comparison with
Non-US Countries. Chapter 2 in Diabetes in America, 3rd ed In: Cowie CC, Casagrande
SS, Menke A, et al., eds. Diabetes in America, 3rd ed. Vol 17-1468. Bethesda, MD:
National Institutes of Health; 2018:1-17.
7. American Diabetes Association. Hyperglycemia (High Blood Glucose). 2018;
http://diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-
control/hyperglycemia.html. Accessed November 27, 2018.
8. Genuth SM, Palmer JP, Nathan DM. Classification and Diagnosis of Diabetes. Chapter
1 in Diabetes in America, 3rd ed. In: Cowie CC, Casagrande SS, Menke A, et al., eds.
Diabetes in America, 3rd ed. Vol 17-1468. Bethesda, MD: National Institutes of Health;
2018:1-39.
9. Cleland SJ, Fisher BM, Colhoun HM, Sattar N, Petrie JR. Insulin resistance in type 1
diabetes: what is 'double diabetes' and what are the risks? Diabetologia. 2013;56:1462-
1470.
10. Centers for Disease Control and Prevention. Diabetes Basics: Who's at Risk? 2017;
https://www.cdc.gov/diabetes/basics/risk-factors.html. Accessed September 26, 2018.
11. Cowie CC, Casagrande SS, Geiss LS. Prevalence and Incidence of Type 2 diabetes
and prediabetes. Chapter 3 in Diabetes in America, 3rd ed. In: Cowie CC, Casagrande
SS, Menke A, et al., eds. Diabetes in America, 3rd ed. Vol 17-1468. Bethesda, MD:
National Institutes of Health; 2018:1-31.
12. American Diabetes Association. How to Treat Gestational Diabetes.
http://diabetes.org/diabetes-basics/gestational/how-to-treat-gestational.html. Accessed
April 30, 2019.
13. California Health Interview Survey. CHIS 2013-2017 Adult Survey. Los Angeles, CA:
UCLA Center for Health Policy Research;2013-2017.
14. California Behavioral Risk Factor Surveillance System (BRFSS). Adult Survey. Public
Health Survey Research Program, California State University, Sacramento;2013-2015.

Burden of Diabetes in California 37 | P a g e California Department of Public Health
15. California Office of Statewide Health Planning and Development. Patient Discharge
Data. 2005-2016.
16. Center for Health Statistics and Informatics. 2007-2016 Death Statistical Master Files.
California Department of Public Health.
17. Centers for Disease Control and Prevention. Smoking and Diabetes. 2018;
https://www.cdc.gov/tobacco/campaign/tips/diseases/diabetes.html. Accessed October
30, 2018.
18. UCLA Center for Health Policy Research. AskCHIS 2013-2017. Ever told has pre- or
borderline diabetes compared by Ever diagnosed with diabetes. Accessed November
28, 2018.
19. National Institute of Diabetes and Digestive and Kidney Disease. Preventing Diabetes
Problems: Diabetes, Heart Disease, and Stroke. 2017;
https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-
problems/heart-disease-stroke. Accessed August 6, 2018, 2018.
20. Centers for Disease Control and Prevention. National Chronic Kidney Disease Fact
Sheet, 2017. 2017.
21. Chronic Kidney Disease (CKD) Surveillance System. Prevalence of ESRD by U.S. State
2016. 2016; https://nccd.cdc.gov/ckd/detail.aspx?Qnum=Q69.
22. Adler AI, Stratton IM, Neil HAW, et al. Association of systolic blood pressure with
macrovascular and microvascular complications of type 2 diabetes (UKPDS 36):
prospective observational study. BMJ. 2000;321.
23. National Eye Institute. Diabetic Retinopathy: What You Should Know. 09/15 2015.
24. National Center for Chronic Disease Prevention and Health Promotion. Age-Adjusted
Percentage of Adults Aged 18 Years or Older with Diagnosed Diabetes Receiving a
Dilated Eye Exam in the Last Year, United States, 1994-2010. 2014;
https://www.cdc.gov/diabetes/statistics/preventive/fx_eye.htm. Accessed January 2,
2019.
25. American Academy of Ophthalmology. Diabetic Retinopathy Treatment.
https://www.aao.org/eye-health/diseases/diabetic-retinopathy-treatment. Accessed May
15, 2019.
26. Boyko EJ, Monteiro-Soares M, Wheeler SGB. Peripheral Arterial Disease, Foot Ulcers,
Lower Extremity Amputations, and Diabetes. In: Cowie CC, Casagrande SS, Menke A,
et al., eds. Diabetes in America, 3rd ed. Vol 17-1468. Bethesda, MD: National Institutes
of Health; 2018.
27. Centers for Disease Control and Prevention. National Diabetes Statistics Report:
Estimates of Diabetes and Its Burden in the United States. 2014. Accessed August 2,
2018.
28. Centers for Disease Control and Prevention. Diabetes: Prevent Complications.
https://www.cdc.gov/diabetes/managing/problems.html. Accessed June 19, 2019.
29. National Institute of Diabetes and Digestive and Kidney Disease. The A1C Test &
Diabetes. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-
diagnosis/a1c-test.
30. Babey SH, Wolstein J, Diamant AL, Goldstein H. Prediabetes in California: Nearly Half
of California Adults on Path to Diabetes. Los Angeles, CA: UCLA Center for Health
Policy Research and California Center for Public Health Advocacy;2016.

Burden of Diabetes in California 38 | P a g e California Department of Public Health
31. American Diabetes Association. The Cost of Diabetes. 2018;
http://www.diabetes.org/advocacy/news-events/cost-of-diabetes.html. Accessed
January 2, 2019.
32. Yoo BK, Xing G, Hoch JS, Taylor C, Núñez de Ybarra J, Peck C. Economic Burden of
Chronic Disease in California in 2018. Under Review. 2018.
33. United States Department of Labor Bureau of Labor Statistics. CPI-All Urban
Consumers (Current Series): Series Title: All items and Medical care in U.S. city
average, all urban consumers, not seasonally adjusted.
https://data.bls.gov/timeseries/CUUR0000SA0?data_tool=Xgtable
;https://data.bls.gov/timeseries/CUUR0000SAM. Accessed November 7, 2018.
34. Centers for Disease Control and Prevention. Chronic Disease and Health Promotion.
2014; http://www.cdc.gov/chronicdisease/overview/index.htm. Accessed October 24,
2018.
35. American Diabetes Association. The Burden of Diabetes in California. 2017.
36. Centers for Disease Control and Prevention- National Center for Health Statistics.
Multiple Cause of Death 1999-2017 on CDC WONDER ONline Database. Data are from
Multiple Cause of Death Files, 1999-2017, as compiled from data provided by the 57
vital statistics jurisdictions through the Vital Statistics Cooperative Program. 2017;
http://wonder.cdc.gov/mcd-icd10.html, June 18, 2019.
37. California Department of Finance. E-2. California County Population Estimates and
Components of Change by Year -- July 1, 2010-2017. Sacramento, CA.
38. United States Census Bureau. State Population by Characteristics: 2010-2017. 2018;
https://www.census.gov/data/datasets/2017/demo/popest/state-detail.html. Accessed
October 2, 2018.
39. Smith M. Pharmacists' Role in Improving Diabetes Medication Management. Journal of
Diabetes Science and Technology. 2009;3(1):175-179.
40. Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes
with community health workers. Family Practice. 2016;33(5):523-528.
41. Centers for Disease Control and Prevention. The 6|18 Initiative: Accerlating Evidence
into Action. 2018; https://www.cdc.gov/sixeighteen/index.html. Accessed January 2,
2019.
42. Institute for Community Collaborative Studies at California State University Monterey
Bay. Prevention First Monterey County.
http://www.preventionfirstmontereycounty.org/community-health-workers. Accessed
January 2, 2019.
43. National Center for Chronic Disease Prevention and Health Promotion. Innovation
Awards- Diabetes, Heart Disease and Stroke.
https://www.cdc.gov/chronicdisease/about/foa/1817/index.htm. Accessed January 2,
2019.
44. CalPERS. Diabetes Prevention Program. https://www.calpers.ca.gov/page/education-
center/member-education/diabetes-prevention. Accessed April 30, 2019.
45. California Department of Health Care Services. Diabetes Prevention Program.
https://www.dhcs.ca.gov/services/medi-cal/Pages/Diabetes-Prevention-Program.aspx.
Accessed April 30, 2019.

Burden of Diabetes in California 39 | P a g e California Department of Public Health
46. California Health Interview Survey. CHIS 2015-2016 Methodology Series: Report 5 --
Weighting and Variance Estimation. Los Angeles, CA: UCLA Center for Health Policy
Research;2017.
47. California Health Information Survey. Pooling CHIS Data Files from Multiple Years. Los
Angeles, CA: UCLA Center for Health Policy Research.
48. Public Health Survey Research Program CSU, Sacramento. California Behavioral Risk
Factor Surveillance System (BRFSS) SAS Dataset Documentation and Technical
Report. 2017.
49. California Department of Finance. Race/Ethnic Population with Age and Sex Detail,
2000-2010. Sacramento, California.
50. Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population.
Hyattsville, Maryland: National Center for Health Statistics; January 2001.
